
Symptoms
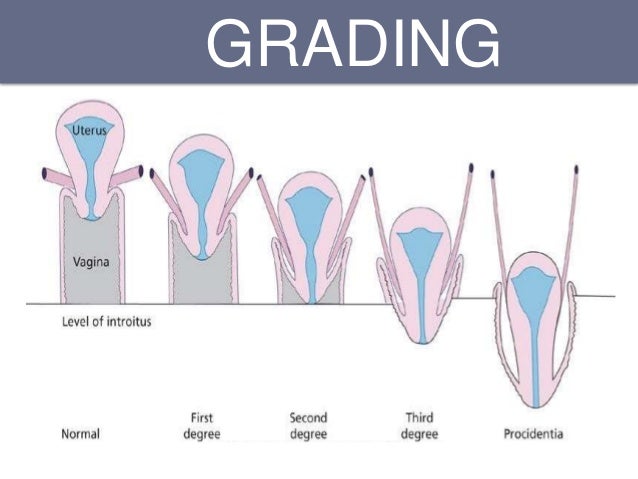
This can occur along with vaginal vault prolapse. Grade 1: This is also called mild cystocele. In this condition, the bladder sags only a short way into the vagina. Grade 2: This is a more severe condition in which the bladder slips down further to reach the opening of the vagina.
Causes
Lower back pain. What are the stages (grades) of cystocele or prolapsed bladder? Depending on how far the bladder has fallen/prolapsed, cystocele is classified into 4 grades: Grade IV – Entire bladder is completely out of the vagina. This is usually associated with other pelvic organ prolapse such as uterine prolapse, rectocele or enterocele.
Prevention
Mild Cystocele (Stage 1) – You can see that the bladder is protruding slightly into the vaginal canal. Moderate Cystocele (Stage 2) – You can see that the bladder is pulled further into the vaginal canal and the urethra is beginning to kink.
Complications
A cystocele ― also known as a prolapsed, herniated, dropped or fallen bladder (where your urine or “water” is stored) ― occurs when ligaments that hold your bladder up and the muscle between a woman’s vagina and bladder stretches or weakens, allowing the bladder to sag into the vagina. There are three grades...
What is a Grade 2 cystocele?
What are the stages (grades) of cystocele or prolapse?
What does Stage 1 cystocele look like?
What is a cystocele?
Does Stage 2 cystocele require surgery?
Grade 2 Cystocele This type of cystocele causes major discomfort and severe urinary incontinence. The treatment for this type of cystocele is usually some form of cystocele repair surgery but the cystocele may also be treated with a pessary device.
Can Stage 2 cystocele be reversed?
Can Pelvic Prolapse be Reversed? Yes! Pelvic organ prolapse can be treated and improve without surgery in some women. Prolapse results when the pelvic floor tissues are overstretched and weakened, just like overstretching a spring.
Can you correct stage 2 prolapse?
Stage I and II uterine prolapse in particular can be helped by pelvic floor muscle exercises, but they need to be done correctly and practised long enough to strengthen the muscles.
How do you fix a Stage 2 bladder prolapse?
Severe prolapsed bladders that cannot be managed with a pessary usually require surgery to correct them. Prolapsed bladder surgery is usually performed through the vagina, and the goal is to secure the bladder in its correct position. The bladder is repaired with an incision in the vaginal wall.
How serious is a cystocele?
Grade 1 is the mildest form of the condition, and grades 3 and 4 are the most serious. With a more advanced cystocele, your bladder and vaginal wall may drop down far enough that they reach or bulge into the vaginal canal and potentially out through the opening of the vagina.
When is surgery needed for cystocele?
If you have incontinence. If you're pregnant or thinking about becoming pregnant, you might need to delay surgery until after you're done having children. Pelvic floor exercises or a pessary may help relieve your symptoms in the meantime.
Can stage 2 prolapse be fixed without surgery?
The two non-surgical options for prolapse are pelvic floor muscle training (PFMT) and a vaginal pessary. PFMT can be effective for mild prolapse but is usually not successful for moderate and advanced prolapse. The main alternative to surgery for prolapse is a vaginal pessary.
Does walking make prolapse worse?
Prolapse symptoms may be worse at different times in the day. Some women notice that they feel more pressure after walking or standing for long periods of time.
Can a woman's bladder fall out?
A cystocele ― also known as a prolapsed, herniated, dropped or fallen bladder (where your urine or “water” is stored) ― occurs when ligaments that hold your bladder up and the muscle between a woman's vagina and bladder stretches or weakens, allowing the bladder to sag into the vagina.
How painful is cystocele surgery?
You may experience discomfort in the vagina for 1-2 weeks following the surgery. The physician may place a medicated vaginal packing in the vagina overnight. The catheter stays for 2-6 days to give the bladder more time to function normally. You may notice bloody discharge and/or odor from the vagina for 1-2 weeks.
Can a cystocele get worse?
Treatment depends on the grade of the cystocele and may include: Activity changes. Avoiding certain activities, such as heavy lifting or straining during bowel movements, that could cause the cystocele to worsen.
Can you leave a prolapsed bladder untreated?
If prolapse is left untreated, over time it may stay the same or slowly get worse. In rare cases, severe prolapse can cause obstruction of the kidneys or urinary retention (inability to pass urine). This may lead to kidney damage or infection.
How can I stop my cystocele from getting worse?
The 4 first-line treatment options for a cystocele includes:Pelvic floor muscle exercises or Kegel exercises. These exercises help strengthen pelvic floor muscles, allowing them to support the bladder and other pelvic organs more effectively. ... A supportive device (pessary) ... Estrogen replacement therapy. ... Surgery.
How do you stop a cystocele from getting worse?
Avoiding certain activities, such as heavy lifting or straining during bowel movements, that could cause the cystocele to worsen. Kegel exercises. Regular, daily exercises of the pelvic muscles to make them stronger.
Can a cystocele get better?
In mild cases, non-surgical treatments may be all that is needed to successfully deal with a cystocele. When surgery is performed for more serious cases, some women will eventually need another surgery because the first surgery failed, the cystocele returned or another pelvic floor problem developed.
Can cystocele improve?
Cystocele repair (bladder prolapse repair) is one of the most commonly performed types of prolapse surgery. Some women with cystocele problems remain active and largely symptom free while others require prolapse surgery for debilitating symptoms.
What is a cystocele?
When the wall between the bladder and the vagina weakens, the bladder may drop or sag into the vagina. This disorder in women is called a cystocele.
How to tell if you have cystocele?
Symptoms of cystocele include: Feeling of pelvic heaviness or fullness. Bulge in the vagina that you can feel. Aching or a feeling of pressure in the lower belly or pelvis. Lower back pain. Frequent urinary tract infections. Need to urinate often or urgently. Leakage of urine. Incomplete emptying of the bladder.
How to make cystocele worse?
Avoiding certain activities, such as heavy lifting or straining during bowel movements, that could cause the cystocele to worsen. Kegel exercises. Regular, daily exercises of the pelvic muscles to make them stronger. Pessary. This is a device placed in the vagina to hold the bladder in place. Surgery.
What tests are done for cystocele?
Tests for a cystocele may include a pelvic exam and urodynamics, a group of tests to evaluate bladder function. Women with moderate to advanced symptoms may opt for a vaginal pessary, a support device that is inserted into the vagina, or cystocele repair surgery.
What is the best way to move the bladder back into a normal position?
May be used to move the bladder back into a more normal position. Hormone replacement therapy . This may help to strengthen the muscles around the vagina and bladder. If you are thinking about hormone replacement therapy , talk to your healthcare provider about the risks and benefits first.
What are the factors that increase the risk of cystocele?
Factors that increase your risk of a cystocele are childbirth, age, obesity, chronic constipation and heavy lifting. Signs and symptoms can include the feeling that something has dropped out of your vagina, leaking urine or a feeling of incomplete emptying of your bladder. In more advanced cases, the vaginal wall that supports ...
What is the test for bladder prolapse?
Other tests may include: Cystourethrogram (also called a voiding cystogram). This is an X-ray of the bladder taken while the woman is urinating and with the bladder and urethra filled with contrast dye. It shows the shape of the bladder and any blockages. MRI can be used to determine the extent of bladder prolapse.
What stage is cystocele graded?
You can see the change in cystocele grading between stage 0 and 1 , stage 1 and 2 and stage 2 and 3 but dragging on the purple sliders on the images below. Note: Surgery is often required when cystocele has reached stages 3 or 4. More information on the condition and treatments.
What is a cystocele?
A cystocele (also known as an anterior prolapse) is a hernia of the front vaginal wall resulting in the bladder bulging into the vaginal passage. Pelvic organ prolapse is often measured in stages ranging from stage 1 which is a minor prolapse, to stage 4 which is complete prolapse. If you are suffering from one type of pelvic organ prolapse, ...
How to make a positive difference in prolapse?
By working on increasing the strength and tone of your pelvic floor muscles, combined with hypopressive style exercises that work to enhance the relationship between the diaphragm and pelvic floor , you can make a positive difference to the grade of you prolapse.
Can cystocele cause UTI?
Sometimes women with cystocele have to splint by lifting the bladder from inside the vagina in order to pee. There can also be difficulty with emptying the bladder fully which can lead to urinary tract infections (UTI). Cystocele symptoms can also have negative impact on sexual function. You can see the change in cystocele grading between stage 0 ...
What is a cystocele?
A cystocele is a condition in which supportive tissues around the bladder and vaginal wall weaken and stretch, allowing the bladder and vaginal wall to fall into the vaginal canal.
How does a cystocele surgery work?
During this procedure, a surgeon puts the bladder back in its normal position and tightens the muscles and tissues that hold the bladder in place using stiches. Your health care professional may perform a procedure to treat or prevent urinary incontinence at the same time as the surgery to repair the cystocele.
How common is a cystocele?
A cystocele is common. Experts estimate that nearly half of women who have given birth have some degree of pelvic organ prolapse. 1 However, many other women with the condition do not have symptoms or do not seek care from a health care professional. As a result, the condition is underdiagnosed, and it is not known exactly how many women are affected by cystoceles.
Who is more likely to have a cystocele?
A cystocele can affect women of any age, but your chances of developing a cystocele increase with age because muscles and tissues often become weaker over time. Other factors that increase your risk of having a cystocele include
What causes a cystocele?
Weakened or damaged muscles and connective tissues that support the bladder and vaginal walls cause a cystocele. Multiple factors may contribute to the stretching or weakening of these muscles and tissues, including
How do health care professionals treat a cystocele?
Your cystocele usually does not need treatment if you don’t have symptoms.
What is the procedure to repair a cystocele?
The most common surgical procedure to repair a cystocele is anterior vaginal repair, also called anterior colporrhaphy.
Why do women get cystoceles?
A woman’s chance of developing a cystocele increases with age, possibly because aging tends to weaken the muscles and supportive tissues of the pelvic floor. Whether menopause increases a woman’s chances of developing a cystocele is unclear.
What is the term for a woman's bladder that bulges into the vagina?
Cystocele, also known as anterior prolapse (or a prolapsed bladder), happens when the supportive tissue between a woman's bladder and vaginal wall weakens and stretches, allowing the bladder to bulge into the vagina.
Do cystoceles show symptoms?
Women with mild cystoceles often do not have any symptoms.
Can cystocele cause bladder infections?
If you are having trouble emptying your bladder or are experiencing heaviness or fullness of the bladder, contact your doctor. If you do have a cystocele, emptying your bladder can be difficult and can lead to bladder infections. If you are suffering from bladder or incontinence issues, Advanced Gynecology is here for you.
Overview
Anterior vaginal prolapse, also known as a cystocele (SIS-toe-seel) or a prolapsed bladder, is when the bladder drops from its usual position in the pelvis and pushes on the wall of the vagina.
Symptoms
In mild cases of anterior prolapse, you may not notice any signs or symptoms. When signs and symptoms occur, they may include:
Causes
Your pelvic floor consists of muscles, ligaments and connective tissues that support your bladder and other pelvic organs. The connections between your pelvic organs and ligaments can weaken over time, or as a result of trauma from childbirth or chronic straining.
Risk factors
Pregnancy and childbirth. Women who have had a vaginal or instrument-assisted delivery, multiple pregnancies, or whose infants had a high birth weight have a higher risk of anterior prolapse.
What are the stages (grades) of cystocele or prolapsed bladder?
Depending on how far the bladder has fallen/prolapsed, cystocele is classified into 4 grades:
What are the causes of bladder prolapse in women?
Incorrect ways of lifting weights. When you lift any weight, pressure must be on the legs but not on the abdomen or on lower back.
What should you do when you see your bladder or anything protruding out of your vagina?
This should be a no-brainer. Talk to your gynecologist, if you have one or look for good gynecologists near you and get in touch as soon as possible. Before the symptoms worsen and the cystocele gets into grade III or grade IV, it is best to get the problem addressed/treated by a specialist.
What is the grade of a cystocele?
Grade 1: This is also called mild cystocele. In this condition, the bladder sags only a short way into the vagina. Grade 2: This is a more severe condition in which the bladder slips down further to reach the opening of the vagina. Grade 3: This is the most severe condition in which the bladder sags so low that it comes out of the vagina.
What is cystocele in a woman?
What is cystocele? Cystocele is the prolapse of the bladder. Cystocele, or bladder prolapse, is a condition in which the bladder sags down into the vagina due to the weakening of the supporting structure between the bladder and the vagina. Pelvic organ prolapse is a condition in which the structures that support the pelvic organs (the pelvic floor) ...
What are the symptoms of cystocele?
Some women with this condition may not have any symptoms or pain. The most common symptom is a bulge through the vagina that may be felt or seen. Other symptoms of cystocele may include
How to tell if you have cystocele?
Other symptoms of cystocele may include. Frequent urge to urinate. Inability to empty the bladder. Loss of bladder control or urinary incontinence. Feeling pressure or fullness in the vagina. Discomfort or pain while passing urine. Discomfort or pain during sexual intercourse. Frequent urinary tract infections.
What happens after a hysterectomy?
Following hysterectomy, the top of the vagina is repaired to form a vaginal vault. During vault prolapse, the vaginal vault drops down into the vaginal canal. Cystocele: In this condition, the bladder bulges into the vagina.
What is it called when the rectum bulges?
Rectocele: When the rectum (the last part of the large bowel) bulges into the vagina, it is called rectocele. Enterocele: This refers to the bulging of the small bowel against the vaginal wall. This can occur along with vaginal vault prolapse. Depending on the severity, cystocele may be. Grade 1: This is also called mild cystocele.
What are the treatment options for a syphilis?
Treatment options include. Watchful waiting: In the absence of symptoms, the doctor may suggest no treatment. They may keep the patient under observation for the development of any symptoms or complications. Conservative (nonsurgical) therapy: This may include.
