Will my compression fracture heal on its own?
Most people can get by without it. Compression fractures usually heal on their own in about 3 months. While that happens, your doctor may suggest you try some things at home that can make you feel better, such as pain medicines, rest, physical therapy, or a back brace.
What you should know about spinal compression fractures?
Symptoms of a Spinal Compression Fracture
- Symptoms
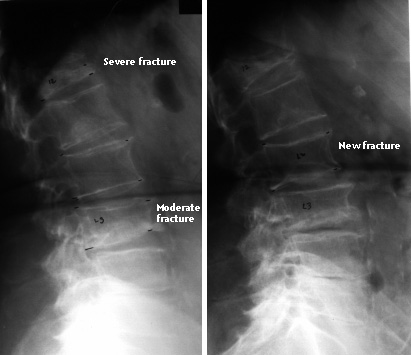
- Different Signs of Spinal Compression Fractures. For many people, a spinal compression fracture will hurt less as the bone heals. ...
- Signs of Multiple Spinal Compression Fractures. When you have multiple spinal compression fractures, your spine will change a lot. ...
- Diagnosing Spinal Compression Fractures. ...
How to treat spinal compression fractures without surgery?
Treatment for Spinal Compression Fractures
- Nonsurgical Treatment for Spinal Compression Fractures. Pain from a spinal compression fracture allowed to heal naturally can last as long as three months. ...
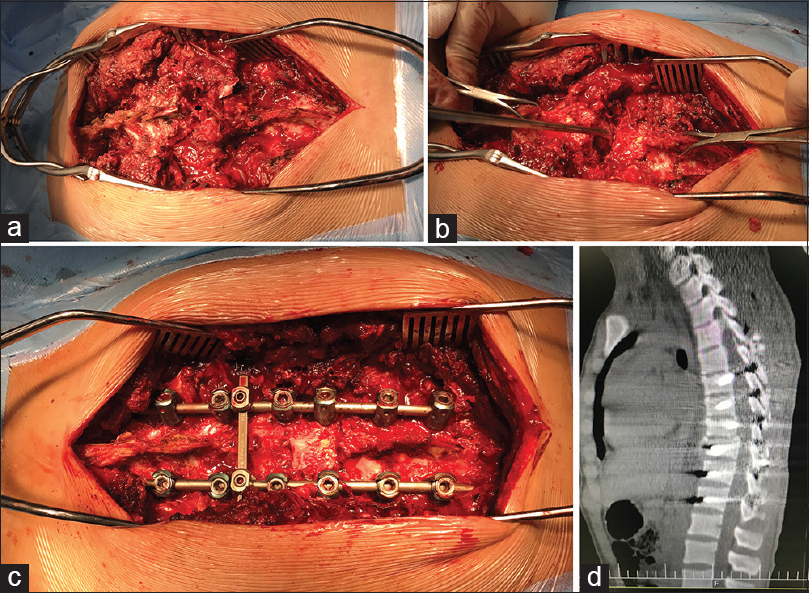
- Surgical Treatment for Spinal Compression Fractures. ...
- Vertebroplasty and Kyphoplasty. ...
- Spinal Fusion Surgery. ...
What do doctors do for broken vertebrae?
You may need any of the following, depending on how severe the fracture is:
- Bed rest may be needed for a mild fracture.
- A back brace may be needed for 8 to 12 weeks. ...
- A cane or walker can help you keep your balance when you walk. ...
- Medicines may be given for pain. ...
- Physical or occupational therapy may be recommended. ...
- Surgery may be needed if your pain, weakness, or numbness does not go away with other treatment. ...
How is a T10 fracture treated?
The most common treatments for a thoracic compression fracture are: pain medications, decreasing activity, and bracing. In rare cases, surgery may also be necessary. Mild pain medications can reduce pain when taken properly. However, remember that medications will not help the fracture to heal.
How long does it take for a T10 compression fracture to heal?
Most compression fractures due to injury heal in 8 to 10 weeks with rest, wearing of a brace, and pain medicines. However, recovery can take much longer if surgery was done. You will lose some height and have a more bent back. Fractures due to osteoporosis often become less painful with rest and pain medicines.
What is a T10 compression fracture?
These compression fractures can occur in vertebrae anywhere in the spine, but they tend to occur most commonly in the upper back (thoracic spine), particularly in the lower vertebrae of that section of the spine (e.g. T10, T11, T12). They rarely occur above the T7 level of the spine.
What does T10 vertebrae control?
The nerve bundles protected by the T10 region have to do with our kidney function and cardiovascular system. As such, those who suffer a subluxation to the T10 can suffer from kidney problems, hardened arteries, exhaustion and chronic fatigue, pyelitis (renal pelvic inflammation) and nephritis (kidney inflammation).
Is walking good for a fractured vertebrae?
Activity Modification However, this does not mean you should stay sedentary until the fracture heals. Low impact activities, such as walking or tai chi, are good for your heart, and a healthy circulatory system can increase blood flow to the fracture and help your bones heal faster.
Is a compression fracture considered a break?
A compression fracture is a type of broken bone that can cause your vertebrae to collapse, making them shorter. This often happens to the front of the vertebrae but not the back, causing you to stoop forward over time.
What does a T10 injury affect?
An injury to the T10 vertebra will likely result in a limited or complete loss of use of the lower abdomen muscles, as well as the buttocks, legs, and feet. A minor injury will result in minor symptoms such as weakness, numbness, as well as partial or complete lack of muscle control over only one side of the body.
Do compression fractures get worse over time?
Multiple untreated compression fractures can eventually lead to severe symptoms and reduced mobility.
Can you walk with a compression fracture in your back?
A compression fracture in the spine does not always need surgery, so doctors may choose some other form of treatment. Treatments that may be used include low-impact activities, so in certain cases, yes, you can walk with a broken vertebra!
Can you walk after T10 spinal cord injury?
There is potential to walk again after SCI because the spinal cord has the ability to reorganize itself and make adaptive changes called neuroplasticity. With an effective rehabilitation plan and consistency, individuals may be able to promote neuroplasticity to optimize their mobility.
Where is T10 on your back?
The T10 vertebra is near the bottom of the twelve (12) thoracic vertebrae (T1-T12) within the torso and making up the central portion of the spinal column. This particular vertebra has a complete articular facet and the thoracic spinal nerves passes out under it. T10 innervates the muscles of the lower abdomen.
What nerve is at T10?
The thoracic spinal nerve 10 (T10) is a spinal nerve of the thoracic segment....Thoracic spinal nerve 10.Thoracic spinal nerveLatinNervi spinalisFMA6309Anatomical terminology3 more rows
Do compression fractures go back to normal?
With the proper precautionary measures and plenty of rest, a compression fracture can typically heal in about three months. During those three months, however, you will need plenty of bed rest, pain medication, calcium supplements, routine icing and heating to mitigate pain.
Does compression fracture pain ever go away?
Pain from a spinal compression fracture allowed to heal naturally can last as long as three months. But the pain usually improves significantly in a matter of days or weeks. Pain management may include analgesic pain medicines, bed rest, back bracing, and physical activity.
How long does pain last with a thoracic compression fracture?
Compression fractures caused by osteoporosis usually become less painful with medicines and rest. They usually heal within 3 months. But some can cause long-term problems.
What aggravates a compression fracture?
In most people, compression fractures due to osteoporosis do not cause any symptoms, but when pain occurs, walking, standing, or sitting for a long time worsens the pain.
How long does it take for a t9 fracture to heal?
Depends: If bones are normal density, no pathology, and was related to no trauma and no nerve damage ... Generally about 6 weeks.
How long does it take to heal a slight fracture of the rib?
Pain is worse : For a few days, followed by 6-8 weeks for healing. After a few days the worst pain usually is gone and it just aches with deep breathing and certain motions and many dont need pan meds. It is important to make sure you are getting a good deep breath and dont develop other issue and to determine the cause or quality of the break with xrays .....Just dont assume.
How long does it take to get answers from a doctor?
Ask U.S. doctors your own question and get educational, text answers — it's anonymous and free! Doctors typically provide answers within 24 hours. Educational text answers on HealthTap are not intended for individual diagnosis, treatment or prescription. For these, please consult a doctor (virtually or in person).
How long does it take to heal a compression fracture?
Depending on the age: Of the patient and severity/type of the fracture as well as patient issues like cigarrette smoking it can vary but on average about 12 weeks for a compression fracture.
How long does it take to video chat with a doctor?
Video chat with a U.S. board-certified doctor 24/7 in less than one minute for common issues such as: colds and coughs, stomach symptoms, bladder infections, rashes, and more.
Can you call 911 for healthtap?
For these, please consult a doctor (virtually or in person). For potential or actual medical emergencies, immediately call 911 or your local emergency service.
What is the T9 Vertebra?
The ninth thoracic vertebra is also known as T9. It is a segment of the thoracic level of the spinal column and is the first of the four transition vertebrae. The T9 vertebra directly communicates to the adrenal glands through nerves.
Where is the T10 Vertebra Located?
The T10 vertebrae location can be found between the T9 and T11 vertebrae within the torso.
Why do thoracic vertebrae fracture?
Thoracic Vertebrae Fractures. Thoracic vertebrae fractures are usually due to accidents with hard falls and physical trauma, or conditions such as osteoporosis. This injury occurs when the vertebrae spine collapses in its weakened state due to pressure.
What is the eleventh thoracic vertebra?
The eleventh thoracic vertebra (T11) is one of the last thoracic spinal vertebrae. It’s the first of the transitional vertebra that is not attached to a true rib, meaning a rib bone that connects to the chest’s sternum.
Why are T9 and T12 considered transitional vertebrae?
Sections T9 - T12 are known as transitional vertebrae because of their proximity and similarity to the lumbar vertebrae. The spinal cord and nerves’ correlation to these levels, along with the rest of the thoracic spine, aid in controlling the trunk of the body. The completeness of the spinal cord damage will determine how severe an injury truly is ...
What are the symptoms of a T11 injury?
A T11 injury will demonstrate itself by severe back and leg pain. If the nerves in the T11 vertebrae are damaged, common symptoms include weakness and numbness in these areas.
What happens if you get a T10 vertebrae?
An injury to the T10 vertebra will likely result in a limited or complete loss of use of the lower abdomen muscles, as well as the buttocks, legs, and feet. A minor injury will result in minor symptoms such as weakness, numbness, as well as partial or complete lack of muscle control over only one side of the body. Severe damage to this vertebra can result in complete paraplegia .
Can You Fully Recover from a Thoracic Spinal Cord Injury?
Recovery from a thoracic spinal cord injury depends on many different factors.
How does spinal cord injury recovery work?
Spinal cord injury recovery primarily focuses on promoting neuroplasticity through massed practice. Neuroplasticity is the spinal cord’s ability to rewire itself and make adaptive changes so that functions affected by damage can be relearned. However, only undamaged neural pathways are capable of utilizing neuroplasticity. Therefore, those with milder SCIs generally have a better recovery prognosis.
What is T5 spinal cord injury?
T1-T5 thoracic spinal cord injuries primarily affect the muscles in the upper chest, mid-back, and inner arms. As a result, individuals with higher-level thoracic injuries may experience difficulties sitting upright due to a lack of trunk stability. The T1 nerve roots affect sensation in your inner forearm and the ability to spread your fingers ...
How does spinal cord injury affect functional abilities?
It’s important to remember that while the level of the SCI provides general information regarding functional outcomes, the severity of the spinal cord injury greatly affects the functional abilities retained following the injury. The affected motor control and sensation of someone with any specific level of SCI can vary significantly, resulting in differing functional abilities.
What to expect after a thoracic spinal injury?
Wondering what to expect after a thoracic spinal cord injury? Following a thoracic spinal cord injury, individuals experience loss of motor control and sensation in the trunk and/or legs (paraplegia). Depending on the level and severity of the spinal cord injury, the amount of motor control and sensation spared will vary.
Why do people with spinal cord injuries have paralysis?
This occurs because signals from the brain are not able to pass through the damage, disrupting the transmission of messages to areas below the level of injury. As a result, individuals with thoracic spinal cord injuries also experience paralysis in their lower ...
How to promote neuroplasticity?
Therefore, those with milder SCIs generally have a better recovery prognosis. The best way to promote neuroplasticity is to consistently practice affected movements. Highly repetitive movements help stimulate the spinal cord and reinforce demand for those functions to promote neurological adaptations.
What are the functions of T12?
T12 Spinal Cord Injury: Functions Affected and Recovery Outlook. A T12 spinal cord injury affects lower body functions such as walking and bowel and bladder functions. Fortunately, individuals with T12 spinal cord injuries generally have normal, full functioning of their upper bodies, which allows a great deal of independence.
What is the treatment for T12 spinal cord injury?
Rehabilitation after a T12 spinal cord injury primarily consists of physical and occupational therapy. These rehabilitative therapies will assess your functional abilities and strive towards maximizing your mobility and independence.
How many segments are there in the T12?
Photo Credit: Ralf Stephan. The thoracic region of your spinal cord is divided into 12 segments that innervate the muscles in your trunk. T12 spinal cord injury patients generally have full function in their upper limbs and trunk. The T12 nerve roots innervate the very lower abdominal muscles. Therefore, individuals with T12 SCIs will focus on ...
What causes a leaky bowel?
1. Bladder and Bowel Dysfunction. Inability to control the bowel and bladder muscles or inability to feel when they are full can cause leakage that you cannot feel or be aware of. Catheterization, bladder augmentation surgery, and medications can help control and better predict bowel and bladder movements. 2.
How does repetition help you move?
The more you repeat a movement, the more you stimulate neuroplasticity in spared neural pathways. With enough practice, your brain, spinal cord, and body can learn to work in sync again. Ultimately, you’re relearning how to move again by promoting neural adaptation.
What is the function of the spinal cord?
Your spinal cord relays messages between your brain and body. After a spinal cord injury, these messages may not be able to make a connection past the site of injury.
Why do I feel spasms after SCI?
Many patients experience spasticity after an SCI because messages between their brain and body are not being communicated properly.
How does kyphoplasty work?
Kyphoplasty involves inserting a tube into the vertebral column under X-ray guidance, followed by the insertion of an inflatable bone tamp. A tiny incision is made in the back. Once inflated, the tamp restores the vertebral body back toward its original height, while creating a cavity to be filled with bone cement.
What happens if the vertebral column breaks?
If the entire vertebral column breaks, it results in a burst fracture. If the compression is mild, you will experience only mild pain and minimal deformity. If the compression is severe, affecting the spinal cord or nerve roots, you will experience severe pain and a hunched forward deformity (kyphosis). Osteoporosis is the most common risk factor ...
What is the purpose of a spinal catheter?
The catheter is used to inject the fractured vertebrae with bone cement, which hardens, stabilizing the vertebral column. This procedure has been shown to reduce or eliminate fracture pain, enabling a rapid return to mobility and preventing bone loss due to bed rest. However, it does not correct the spinal deformity.
What causes spinal cord pain?
These severe injuries frequently result in spinal instability, with a high risk of spinal cord injury and pain. Osteoporosis, or weakening of the bones, can lead to painful vertebral compression fractures. Until recently the only treatment was bracing and narcotic medications which frequently lead to ongoing pain and progressive deformity.
What causes a fractured spine?
Spinal fractures can be caused by accidents or occur as a result of osteoporosis. Surgery may be needed for severe cases. Appointments & Access. Contact Us.
How to stabilize a vertebra?
Stabilization can also be achieved by removing broken vertebra and replacing them with a plate, screws, or cage.
How long does it take to heal a fractured bone?
Most fractures are treated with immobilization in a brace or corset for up to 12 weeks. Bracing helps to reduce pain and prevent deformity.
How to treat unstable T12 and L1?
Treatment for unstable T12 and L1 burst fractures require a surgical procedure to connect your spine to keep it together and straight. Your surgeon may also use bone grafts to help heal the T12 and L1 vertebrates that were injured.
What is the prognosis for a burst fracture?
The prognosis for your burst fracture highly depends on the severity of your L1 and T12 fracture. Burst fractures are classified either stable or unstable. When the burst fracture is stable, the amount of spinal nerve compression is low. Whereas an unstable fracture has a high degree of nerve compression, which can result in neurological issues such as loss of motor functions. Initially, you will most likely require medical attention immediately after your injury to help determine the severity of your fracture.
How long do you need to wear compression brace for a T12 fracture?
Typically, individuals suffering from a stable T12 burst fracture have to wear a compression brace for around 8 to 12 weeks, depending on how fast your spine is healing. Thoracic spine braces for a burst fracture should apply an adequate amount of pressure while simultaneously reducing the amount of movement in your back.
What is wedge fracture?
A wedge fracture is a type of spinal fracture in which the front part of the spinal bone becomes a wedge shape. Wedge fractures can occur either anteriorly or laterally ...
What does it mean when you have a T12 or L1 vertebral burst?
What Does it Mean If I’ve Been Diagnosed with a T12 or L1 Vertebral Burst Fracture? If you’re diagnosed with a burst fra cture, it’s likely the vertebrates you’ve fractured are located in the thoracic spine (middle spinal region). Burst fractures are commonly found in the lower thoracic back due to its natural curve and are considerably more ...
How to treat a L1 burst fracture?
If there are no neurologic malfunctions, the best way to treat a stable L1 burst fracture is by wearing an orthopedic brace to support your spine. Wearing such back braces can help prevent your spine from going out more and can help get it on the right track to recovery.
Where are burst fractures most common?
Since burst fractures typically don’t just occur in one vertebra, the most common direct locations for a burst fracture is in the T12 and L1 vertebrates. A burst fracture frequently results from a severe trauma such as a fall or car accident for example. When you’ve endured a burst fracture to your spine, one part of your vertebrae essentially ‘bursts’ in many different directions. This is the most severe type of spinal fracture because it can result in compressing the nerves, leading to neurological complications.
What is a Burst Fracture?
A burst fracture is a descriptive term for an injury to the spine in which the vertebral body is severely compressed. They typically occur from severe trauma, such as a motor vehicle accident or a fall from a height. With a great deal of force vertically onto the spine, a vertebra may be crushed.
What happens if you burst a bone?
With a greater amount of force, more bony fragments can be forced into the spinal canal causing greater loss of spinal cord function. This may cause loss of strength, sensation or reflexes below the level of the injury.
What happens if you crush the entire margin of the vertebral body?
Also, by crushing the entire margin of the vertebral body the spine is much less stable than a compression fracture.
What does it mean when a vertebral bursts?
The term burst implies that the margins of the vertebral body spread out in all directions. This is a much more severe injury than a compression fracture for two reasons. With the bony margins spreading out in all directions the spinal cord is liable to be injured. The bony fragment that is spread out toward the spinal cord can bruise ...
What happens if you crush a vertebra?
Photo Source: 123RF.com. If it is only crushed in the front part of the spine, it becomes wedge shaped and is called a compression fracture. However, if the vertebral body is crushed in all directions it is called a burst fracture. The term burst implies that the margins of the vertebral body spread out in all directions. This is a much more severe injury than a compression fracture for two reasons. With the bony margins spreading out in all directions the spinal cord is liable to be injured. The bony fragment that is spread out toward the spinal cord can bruise the spinal cord causing paralysis or partial neurologic injury. Also, by crushing the entire margin of the vertebral body the spine is much less stable than a compression fracture.
What is a physical exam for spinal deformity?
The physical exam should be performed to document both spinal deformity, that is, angulation of the spine or tenderness of the spine at the level of fracture, as well as, a neurologic exam.
How to diagnose a burst fracture?
The diagnosis of a burst fracture is usually made by x-rays and a CAT scan. Occasionally, an MRI scan may be ordered as well, in order to assess the amount of soft tissue trauma, bleeding or ligament disruption. The review of the CAT scan and x-rays allows the treating physician to make a determination as to the level of the fracture, whether it is a compression fracture, burst fracture or fracture dislocation, and to determine the amount of spinal canal compromise and spinal angulation. All of these factors enter into the treatment decision process.
