How do you get a VRE infection?
VRE are often spread indirectly from person to person on the hands of caregivers or contact with contaminated items (e.g., medical equipment) or surfaces (e.g., toilet seats, door knobs). VRE can also spread directly from person to person by contact with body fluids containing VRE (e.g., blood, feces, urine).
What is VRE infection symptoms?
Symptoms of a VRE infection depend on where the infection is: If VRE is in a wound, that area of your skin may be red or tender. If VRE is in the urinary tract, you may have back pain, a burning sensation when you urinate, or a need to urinate more often than usual.
How serious is VRE infection?
VRE infections typically affect people who are already sick and in the hospital. These infections can be hard to treat because doctors have fewer options that are effective against the resistant bacteria. Some VRE infections may be life-threatening.
Is VRE the same as MRSA?
Methicillin-resistant Staphylococcus aureus (MRSA) and vancomycin-resistant Enterococci (VRE) are specific, antibiotic-resistant bacteria that spread by contact and can cause serious infections.
How long does it take to recover from VRE?
In some people, the VRE infection can go away on its own as their bodies naturally become stronger. This process can take a few months or even longer.
How long does VRE last for?
The VRE germ can survive on hard surfaces for five to seven days and on hands for hours.
Can VRE cause death?
Forty percent of patients with VRE bacteremia died within 30 days. Patients with a bone marrow transplant, solid organ transplant, cancer, or who are admitted to the intensive care unit are at highest risk of VRE bacteremia.
What is the treatment for VRE?
VRE infections may be difficult to cure because the bacteria do not respond to many antibiotics. If you have an infection, your doctor will order antibiotics that may be given by mouth or into a vein through an IV (intravenously). Sometimes more than one antibiotic is prescribed to help stop the infection.
What antibiotic is used for VRE?
For treatment of severe VRE infections, options include penicillin or amoxicillin +/– aminoglycoside, QPD, or newer agents such as LZD, daptomycin, and tigecycline.
What is VRE and how is it contracted?
VRE can spread from one person to another through contact with contaminated surfaces or equipment or through person to person spread, often via contaminated hands. It is not spread through the air by coughing or sneezing.
What is one of the best ways to prevent the spread of MRSA and VRE?
Clean hands often, and clean your body regularly, especially after exercise. Keep cuts, scrapes, and wounds clean and covered until healed. Avoid sharing personal items such as towels and razors.
What do most cases of MRSA and VRE have in common?
MRSA and VRE are both spread by contact, either with the contaminated hands of caregivers and/or with objects contaminated by the skin or body fluids of an infected person. They are not spread through the air like the common cold or influenza.
What is the treatment for VRE?
VRE infections may be difficult to cure because the bacteria do not respond to many antibiotics. If you have an infection, your doctor will order antibiotics that may be given by mouth or into a vein through an IV (intravenously). Sometimes more than one antibiotic is prescribed to help stop the infection.
What antibiotic is used for VRE?
For treatment of severe VRE infections, options include penicillin or amoxicillin +/– aminoglycoside, QPD, or newer agents such as LZD, daptomycin, and tigecycline.
What are the signs and symptoms of Enterococcus faecalis?
Symptoms of E. faecalis infectionsfever.chills.fatigue.headache.abdominal pain.pain or burning when you urinate.nausea.vomiting.More items...
Who is at risk for VRE?
Patients at high risk for VRE infections include those who are undergoing complex or prolonged healthcare (such as patients in long-term acute care hospitals or ICUs) or patients with weakened immune systems (such as patients undergoing cancer treatment or with organ transplants).
How is it spread?
It is not spread through the air by coughing or sneezing.
How are these infections treated?
In order to identify the best antibiotic to treat a specific infection, healthcare providers will send a specimen (often called a culture) to the laboratory and test any bacteria that grow against a set of antibiotics to determine which are active against the germ. The provider will then select an antibiotic based on the activity of the antibiotic and other factors like potential side effects or interactions with other drugs.
What is CDC doing to address VRE infections?
This surveillance system collects reports of VRE from device-associated infections, such as central-line associated bloodstream infections.
Why are enterococci resistant to antibiotics?
Antibiotic resistance occurs when the germs no longer respond to the antibiotics designed to kill them.
How many deaths from VRE in 2017?
In 2017, VRE caused an estimated 54,500 infections among hospitalized patients and 5,400 estimated deaths in the United States [ Source: 2019 AR Threats Report ].
What areas of the home can be contaminated with VRE?
frequently cleaning areas of the home, such as bathrooms, that may become contaminated with VRE
Why should you wash your hands?
keeping your hands clean to avoid getting sick and spreading germs that can cause infections. patients and their caregivers should wash their hands with soap and water or use alcohol-based hand sanitizer, particularly: after using the bathroom. before and after handling medical devices or caring for wounds. before preparing food.
What is a VRE patient?
People with a history of surgical procedures, such as abdominal or chest surgery. People with invasive medical devices, such as urinary catheters and central intravenous (vein) catheters. People who are colonized with VRE.
How is VRE spread?
VRE can also spread directly from person to person by contact with body fluids containing VRE (e.g., blood, feces, urine). ...
What is a VRE?
What are vancomycin-resistant enterococci (VRE)? Enterococci are a type of bacteria (germ) normally present in the gut and in the female genital tract. They are also found in the environment. Vancomycin is an antibiotic often used to treat infections caused by enterococci.
Where do most VRE infections occur?
Most VRE infections occur in hospitals. People with the following conditions are at increased risk for getting infected with VRE: People with previous treatment with vancomycin or other antibiotics for long periods of time. People with a recent hospitalization (s), especially if long courses of antibiotic treatment are involved.
How to take antibiotics if you feel better?
Follow the healthcare provider’s instructions. If your provider prescribes you antibiotics, take them exactly as instructed and finish the full course, even if you feel better. Follow any other medical or hygiene advice your provider gives you.
What are the symptoms of a wound infection?
Wound infection symptoms might also include swelling, redness, and discharge (pus).
How to wash your hands after a sneeze?
Always wash your hands with soap and water, especially before eating or preparing food, before and after changing wound dressings or bandages, after using the bathroom, and after blowing your nose, coughing, or sneezing. Use alcohol-based hand sanitizer when soap and water are not available.
How Is VRE Diagnosed?
To confirm a VRE infection, your doctor will send a sample of your infected wound, blood, urine, or stool to the lab for analysis. At the lab, technicians will grow the bacteria and test it to see which antibiotics can kill the bacteria. If vancomycin can’t kill it, that confirms the existence of VRE.
What are the symptoms of VRE?
VRE can infect the bloodstream, the urinary tract (as a UTI ), and wounds associated with catheters or surgery. Bloodstream infections can cause: Fever. Chills.
How does VRE evolve?
To understand how antibiotic-resistant bacteria such as VRE emerges, it helps to first understand how bacteria and fungi change in response to medicines designed to kill them. According to the CDC Antibiotic Resistance Threats Report, germs naturally evolve constantly, and can develop new ways to avoid the effects of antibiotics. Once that happens, the resistant germ survives and multiplies, and the surviving germs, which now have resistance traits in their DNA, pass on this genetic information to subsequent generations. These resistant germs can continue to spread and pose an increasing threat to people’s health.
What does VRE stand for?
Copy Link. Medically Reviewed. VRE stands for vancomycin - resistant enterococci. Enterococci are bacteria that normally live in the intestines and in the female genital tract, and are also present in soil and water. Most of the time, these germs don’t cause any harm, but if they get into certain places in the body, such as the urinary tract, ...
Why is VRE so hard to treat?
National Library of Medicine, VRE infections can be difficult to treat because there are fewer antibiotics that can fight this resistant bacteria. In fact, VRE is listed as one of the key antibiotic-resistant pathogens that pose a threat to human health in the Centers for Disease Control and Prevention’s 2019 Antibiotic ...
How is VRE spread?
VRE is typically not spread through the air like a cold or the flu and it cannot be spread through casual contact such as hugging. It is spread by direct contact with an infected person’s bodily fluids, such as blood, phlegm, urine, or stool, or by touching surfaces that have been contaminated by the bacteria.
What is the treatment for a VRE infection?
Treatment and Medication Options for VRE. When someone develops a VRE infection, doctors typically turn to antibiotics that are alternatives to vancomycin.
How To Treat VRE Infection?
When a person is suffering from VRE infection he is kept in an isolated ward so that he may not spread infection to others. Extra precautionary measures are taken by the attending health care workers and doctors, such as wearing gloves and gowns while handling the patient or examining him.
What are the symptoms of antibiotic resistant infection?
The systemic symptoms may include high fever, headache, chills, fast heart rate, giddiness, low appetite, weakness and drowsy feeling. Low blood pressure is also common if there is septic shock as a result of VRE infection.
What is the problem with enterococci?
The problem arises when enterococci cause infection. The common sites of enterococcus infection include intestine, skin and urinary tract. VRE infection can have serious outcome especially in people who have low immune level and those who are weak, suffering from chronic ailments such as diabetes, kidney disease and cancer.
How does VRE spread?
Causes Of VRE Infection. It is usually transmitted from one person to other person in hospital. Microscopic amount of fecal matter of the patient contaminates hospital environment and the hands of health care personal of the hospital. The soiled bed linen and clothes of a person who has VRE are also the source of spreading the infection.
What are the symptoms of a urinary infection?
If infection is limited to urinary tract, there is burning urination, fever, pain in back, red urine and other urin ary tract symptoms.
How many antibiotics are used for drug resistant?
Sometime two antibiotics are used in drug resistant cases. Except vancomycin, many other potent antibiotics are used to treat the condition. In most people the symptoms may alleviate once the immune system becomes stronger. Often it may take long time.
Is VRE a hard infection to treat?
VRE infection is difficult to treat as the enterococci bacteria have become resistant to many antibiotics. For this reason doctors may advise culture and sensitivity of blood, urine and stool and cerebrospinal fluid as the case may be.
What is the name of the bacteria that live in the intestines?
Everyone has certain bacteria, called enterococci, that live in their intestines and genital tract. They’re also found in the environment. Most of the time they don’t cause any problems, but sometimes they can trigger infections. When they do, they’re treated with a powerful antibiotic called vancomycin. Sometimes, the bacteria become resistant ...
What happens if a lab test is positive for VRE?
If the sample tests positive -- meaning you have VRE -- they’ll do more tests to find out which antibiotic will best treat it .
Why are superbugs dangerous?
These superbugs are called vancomycin-resistant enterococci, or VRE. They’re dangerous because they’re more difficult to treat than regular infections.
How to wash your hands after a VRE?
Wash your hands with soap and water after using the bathroom and before making food -- especially if you’re in contact with someone who has VRE. A good rule of thumb is to wash up long enough to sing “Happy Birthday to You” twice.
Can VRE cause urinary tract infections?
VRE comes with a number of symptoms. Yours might actually be caused not by VRE, but by other infections it can trigger, like urinary tract infections, bloodstream infections, and wound infections. The time between when you’re infected and when you develop symptoms varies, too.
What increases my risk for a VRE infection?
Treatment with vancomycin or other antibiotics for an extended length of time
What are the signs and symptoms of a VRE infection?
Symptoms may depend on where the infection is. You may have any of the following:
How is a VRE infection diagnosed?
Blood tests check for VRE and help healthcare providers plan which antibiotics are best for treatment.
How do I prevent the spread of VRE?
Do the following if you or someone you care for has an active VRE infection:
What is a VRE?
What is a vancomycin resistant enterococcus (VRE)? VRE is a strain of bacteria that can cause infection. Usually the antibiotic vancomycin is used to kill the bacteria. However, VRE is resistant to vancomycin and makes it difficult to treat. VRE most commonly causes an infection in the urinary tract, blood, or a wound.
How does VRE spread?
VRE spreads if the person touches something that comes in contact with your urine, bowel movements, or infected wound. For example, VRE can be transferred on towels, wash cloths, and surfaces that touch body fluids. VRE bacteria can live in the intestines, urinary tract, vagina, or mouth without causing infection.
How to clean a kitchen counter?
Use disinfecting cleaners if you do not have wipes. You can create a disinfecting cleaner by mixing 1 part bleach with 10 parts water. In the kitchen, clean countertops, cooking surfaces, and the fronts and insides of the microwave and refrigerator. In the bathroom, clean the toilet, the area around the toilet, the sink, the area around the sink, and faucets. Clean surfaces in the person's room, such as a desk or dresser.
What are the precautions to prevent VRE?
These precautions include: Single room accommodation (the door can remain open). A long-sleeved gown and gloves must be worn by everyone who cares for you.
What is VRE in medical terms?
Vancomycin Resistant Enterococcus (VRE) Fact Sheet. Information for Patients and Visitors. What is VRE? Enterococci are germs that live in the gastrointestinal tract (bowels) of most individuals and generally do not cause harm (this is termed “colonization”). Vancomycin-resistant enterococci ...
How is VRE spread?
VRE is spread from one person to another by contact, usually on the hands of caregivers. VRE can be present on the caregiver’s hands either from touching contaminated material excreted by an infected person or from touching articles soiled by faeces.
What is a VRE?
Vancomycin-resistant enterococci (VRE) are strains of enterococci that are resistant to the antibiotic vancomycin. If a person has an infection caused by VRE, such as a urinary tract infection or blood infection, it may be more difficult to treat. How is VRE Spread?
How long should you rub your hands before touching them?
Remind all staff and visitors to practice good hand hygiene before and after they touch you. Ask your nurse or doctor to demonstrate proper hand hygiene techniques (15 seconds of soap and running water OR waterless alcohol hand rub until hands are dry).
Should you wash your hands after going to the toilet?
Everyone who might help you with your personal hygiene or with going to the toilet should wash his or her hands after contact with you.
Can clothes be laundered?
Clothing may be laundered in the same manner as the rest of the household laundry.
Who Is at Risk?
Medically ill patients are at increased risk of developing and dying from a VRE infection. This includes:
What are the risks of VRE?
Medically ill patients are at increased risk of developing and dying from a VRE infection. This includes: 1 People who are elderly and frail 2 Those previously treated for long periods of time with vancomycin or other antibiotics 3 Hospitalized patients, particularly those receiving long courses of antibiotics 4 Immunocompromised patients in such as those in intensive care units, cancer or transplant units 5 Surgical patients who have undergone procedures involving the abdomen or chest. 6 People with medical devices such as urinary catheters or central intravenous (IV) catheters 7 People who are colonized with VRE
What is VRE in hospitals?
Vancomycin-resistant enterococci, or VRE, is an infection that began appearing in hospitals in the early 1990s. While not as terrifying as flesh-eating bacteria, VRE can cause significant problems.
What is vancomycin used for?
It was originally developed for infections that are resistant to penicillin, including MRSA (methicillin-resistant Staphylococcus aureus) and the oral form is used to treat another tough infection, C. difficile .
What is the name of the drug that kills bacteria?
Antibiotics are drugs that can kill or inhibit disease-causing bacteria. Unfortunately, antibiotics are commonly overused and misused. As a result, bacteria that should be destroyed by antibiotics have, in some cases, become antibiotic-resistant. Vancomycin is an antibiotic that has been around for more than 50 years.
When did VRE start?
Vancomycin-resistant enterococci, or VRE, is an infection that began appearing in hospitals in the early 1990s. While not as terrifying as flesh-eating bacteria, VRE can cause significant problems. Maskot / Getty Images.
What are the steps to prevent a hospital acquired infection?
These include: Careful and frequent hand-washing. Immediate and appropriate treatment of cuts, scrapes, or other breaks in the skin.
What causes endocarditis in the GI tract?
Enterococci are the second most common cause of infective endocarditis. Common sources are central lines, GI or GU tracts after manipulation, damaged mitral or aortic valve infections, or liver transplantation. Community-acquired endocarditis can occur, and it is usually due to E. faecalisin patients with no risk factors. Clinically, they present subacutely with fevers and constitutional symptoms. Typical signs of infection include fevers or a new murmur. Typical stigmata of endocarditis such as petechiae, Osler nodes, and Roth spots are rare and, as with other etiologies, typically occur with subacute infection rather than acute infection.
How can VRE be transmitted?
There are reports that VRE can be transmitted by direct patient contact, touching of contaminated surfaces/equipment or through hand transfer after contact with the affected patient. In almost every hospital in the US, VRE has become a serious problem. In response to this epidemic, almost every hospital now has an infectious disease committee that oversees the use of antibiotics and audits procedures at the bedside for sterility. It is here that the role of the infectious disease nurse and pharmacist is vital. The current recommendations are to 1) only use vancomycin when absolutely needed, and permission must be obtained from the board-certified infectious disease pharmacist and clinician infectious disease specialist 2) educate all healthcare workers about VRE 3) implement infection control measures including hand washing, gloves, and gowns when coming into contact with patients who have VRE and 4) maintain a clean working environment with strict aseptic control. There is evidence to support the use of an interprofessional approach to prevent nosocomial spread of VRE. Many hospitals have now enforced the use of contact isolation and regular surveillance cultures. [17][18][19](Level V)
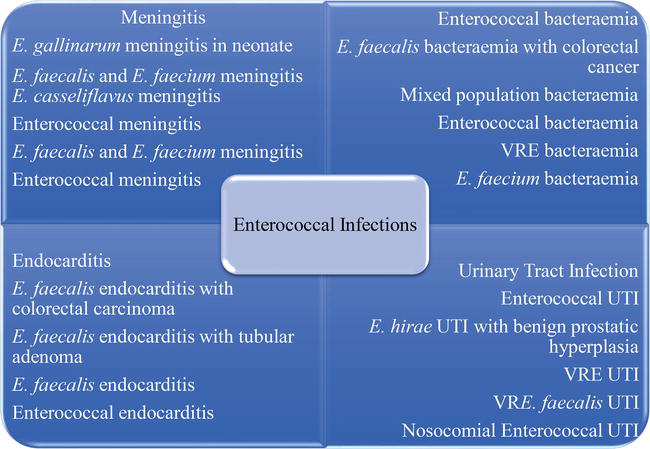
What is the most common clinical presentation of Enterococcus?
Enterococcus can cause a wide range of clinical diseases. The most common clinical presentation is bacteriuria, though it is becoming increasingly clear that many of these cases are due to colonization rather than infection. Other frequent causes of infection are bacteremia without endocarditis, followed by endocarditis.
What are the risk factors for vancomycin-resistant Enterococcus?
The most commonly observed risk factor is previous antimicrobial therapy. This mechanism likely is due to alteration in bowel flora. Furthermore, patients at increased risk are those with severe underlying illnesses or immunosuppression. This also includes patients with a long hospital stay, admission to long-term care facilities, extended use of antibiotics, and proximity to other patients with vancomycin-resistant Enterococcus. [8][9]
What is tigecycline used for?
Tigecycline, a glycylcycline antibiotic, can be used for patients who are intolerant to other agents. It also can be used if other infections are present with the vancomycin-resistant Enterococcus as it has good coverage against gram positives, some gram negatives, and anaerobes. Although it is off-label, it is specifically considered a preferred agent for polymicrobial intraabdominal infections. It should not be used for vancomycin-resistant Enterococcus bacteremia as it distributes primarily to tissues and achieves low serum concentrations. Typical dosing is 100 mg IV once followed by 50 mg IV twice a day. Patients should be monitored for major adverse effects such as nausea and vomiting.
What is the Creative Commons 4.0 license?
This book is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits use, duplication, adaptation, distribution, and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, a link is provided to the Creative Commons license, and any changes made are indicated.
Is vancomycin resistant to beta lactams?
E. faecalistends to be susceptible to beta-lactams and aminoglycosides. Vancomycin resistance is more frequent in undifferentiated E. faecalisthan resistance to aminopenicillins, stressing that beta-lactams should remain the first choice in most infections before culture data. Conversely, most strains of E. faeciumare highly resistant to beta-lactams and aminoglycosides. In general, if vancomycin-resistant Enterococcus is highly resistant to other antimicrobial therapies; the two major treatments are linezolid and daptomycin. A meta-analysis of these two therapies has shown that the overall mortality, clinical cure, microbiological cure, and relapse rate were not significantly different. Importantly, the most common genotypic causes of vancomycin resistance are VanAand VanBwhich are inducible resistance genes. As a result, patients with initially vancomycin sensitive isolates that do not respond to treatment should be re-cultured.