What is the difference between placenta accreta and percreta?
Placenta increta and placenta percreta are similar to placenta accreta, but more severe. Placenta increta is a condition where the placenta attaches more firmly to the uterus and becomes embedded in the organ's muscle wall.
What is placenta accreta spectrum (Pas)?
Placenta accreta, also known as placenta accreta spectrum (PAS), is a pregnancy complication that occurs when the placenta attaches too deeply into the wall of the uterus. The risk for developing accreta increases with each C-section or uterine surgery.
What is the difference between normal delivery and accreta?
During a normal delivery, the placenta detaches from the uterus during the last stage of labor. This can also be referred to as the “afterbirth.” With accreta, the placenta is tightly attached to the uterine wall and does not separate naturally during delivery. This causes several complications for the baby and mother.
What is National accreta Foundation doing for You?
National Accreta Foundation helps connect placenta accreta, increta and percreta patients & families with resources and content of value. October is Accreta Awareness Month and focuses attention on placenta accreta, one of the fastest growing life-threatening complications of pregnancy.
What is the difference between placenta accreta and Percreta?
Placenta increta – The placenta attaches itself even more deeply into the muscle wall of the uterus. Placenta percreta – The placenta attaches itself and grows through the uterus, sometimes extending to nearby organs, such as the bladder.
What does Accreta mean?
Placenta accreta is a serious pregnancy condition that occurs when the placenta grows too deeply into the uterine wall. Typically, the placenta detaches from the uterine wall after childbirth. With placenta accreta, part or all of the placenta remains attached.
What are the symptoms of placenta accreta?
Typically, women with placenta accreta do not have any signs or symptoms, although you might experience bleeding during the second half of pregnancy. If you have had multiple C-sections or surgery on or around your uterus, you should see a doctor as early as possible to make sure you and your baby are safe.
What causes Accreta?
Placenta accreta occurs during pregnancy when the placenta attaches too deeply into the wall of your uterus. People who have had multiple C-sections, other placenta disorders or a history of uterine surgery are at higher risk of developing placenta accreta. This condition can be life-threatening.
What is the death rate of placenta accreta?
Introduction. Placenta accreta spectrum (PAS) is a serious condition with a mortality as high as 7%.
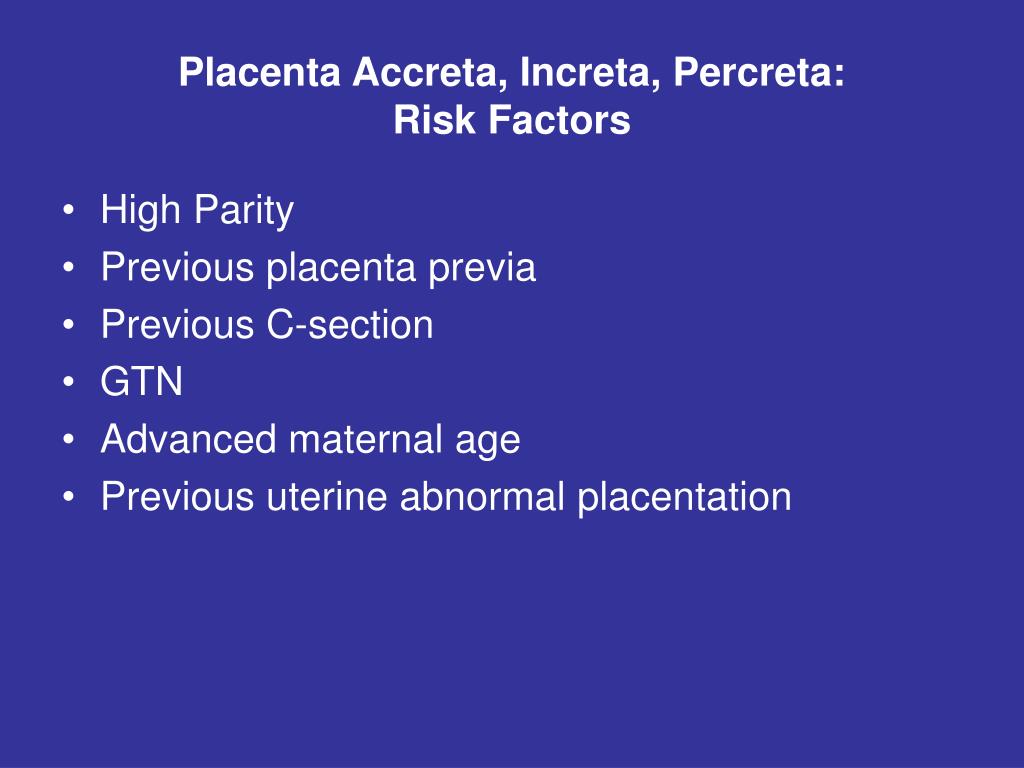
Who is at risk for placenta accreta?
Additional risk factors include advanced maternal age, multiparity, prior uterine surgeries or curettage, and Asherman syndrome 8 11 12. Placenta previa is another significant risk factor. Placenta accreta spectrum occurs in 3% of women diagnosed with placenta previa and no prior cesarean deliveries.
What is the treatment for placenta accreta?
Surgery is the most common and effective treatment for accreta. After the birth of the baby, this usually involves either the surgical removal of the placenta, or a hysterectomy to remove the uterus along with the accreta. The ovaries are almost always left in place if a hysterectomy is performed.
How long does it take to recover from placenta accreta?
Placenta Accreta and Hysterectomy Almost all hysterectomies with placenta accreta take place right after delivery. Severe cases may require a delayed hysterectomy several weeks later. In either case, you will remain in the hospital for several days. Total recovery takes about eight weeks.
How do you treat placenta accreta?
In the case of extensive placenta accreta, a C-section followed by the surgical removal of the uterus (hysterectomy) might be necessary. This procedure, also called a cesarean hysterectomy, helps prevent the potentially life-threatening blood loss that can occur if there's an attempt to separate the placenta.
What is placenta accreta?
Placenta Accreta: A condition of pregnancy where the placenta's blood vessels attach too deeply to the uterine wall. Placenta Increta: A condition where the placenta attaches more firmly to the uterus and becomes embedded in the organ's muscle wall.
Is placenta Percreta fatal?
Placenta percreta, the rarest and most severe form of placenta accreta, can involve the urinary bladder. Because of its propensity for severe hemorrhage, it is a potentially life-threatening condition.
What is morbidly adherent placenta?
Morbidly adherent placenta is one of the most devastating complications in pregnancy [10]. It is characterized by the attachment of placental villi directly to the myometrium, sometimes invading deeper into the uterine wall or surrounding organs.
What is the least common type of placenta creta?from babymed.com
A placenta percreta is the least common type of the placenta creta conditions, presenting itself in about 5% of all these cases. This occurs when the placenta attaches itself so deeply that it attaches to another organ, such as the bladder.
How much blood did the placenta lose?from uchealth.org
The placenta had pushed through the uterus and invaded a quarter-sized patch of the bladder’s outer wall. As Corr and a big OR team worked, she lost half her total blood volume. That was far from the worst the team had seen: a new mother lost 13 liters of blood in a surgery Guntupalli recently led.
What is the placenta that hangs on?from uchealth.org
It hangs on in one of three ways. Placenta accreta occurs when the placenta binds itself to the uterus wall. Placenta increta involves invasion into the uterus’s muscles. Placenta percreta is when the placenta becomes a sort of malignancy, growing through the uterus wall and, often, into neighboring organs such as the kidney and bowels.
What is the placenta accreta?from uchealth.org
The various forms of placenta accreta happen when the life-giving placenta decides to cling to its own existence rather than be birthed with the baby for whom it provided oxygen and removed waste as surrogate in-womb lungs and kidneys. It hangs on in one of three ways. Placenta accreta occurs when the placenta binds itself to the uterus wall. Placenta increta involves invasion into the uterus’s muscles. Placenta percreta is when the placenta becomes a sort of malignancy, growing through the uterus wall and, often, into neighboring organs such as the kidney and bowels.
How many pregnancies does the placenta creta occur in?from babymed.com
Depending on how deep the placenta invades the uterus, placenta creta can present itself in three different forms: A placenta creta is present in about 1 in 2500 pregnancies today. Read on to find out more about each placenta condition, what it means for you, and what it means for your unborn child.
What is the term for the placenta that grows during pregnancy?from babymed.com
A placenta creta, accreta, increta, or percreta is a placenta that grows during pregnancy into or through the uterus. Having this condition is life-threatening and requires expert surgical and medical care.
What happens when the placenta attaches too much to the uterus?from babymed.com
When the placenta attaches too much to the uterus, only a hysterectomy, the removal of the uterus with the placenta attached, can save the mother's life and prevent too much bleeding.
What is the term for the placenta that grows too deeply into the uterine wall during pregnancy?
Close. Placenta accreta. Placenta accreta. Placenta accreta occurs when the placenta grows too deeply into the uterine wall during pregnancy. Scarring in the uterus from a prior C-section or other uterine surgery may play a role in developing this condition.
Why is my placenta accreta sore?
Placenta accreta is thought to be related to abnormalities in the lining of the uterus, typically due to scarring after a C-section or other uterine surgery. Sometimes, however, placenta accreta occurs without a history of uterine surgery.
What are the risks of a placenta accreta?
Placenta accreta can cause: 1 Heavy vaginal bleeding. Placenta accreta poses a major risk of severe vaginal bleeding (hemorrhage) after delivery. The bleeding can cause a life-threatening condition that prevents your blood from clotting normally (disseminated intravascular coagulopathy), as well as lung failure (adult respiratory distress syndrome) and kidney failure. A blood transfusion will likely be necessary. 2 Premature birth. Placenta accreta might cause labor to begin early. If placenta accreta causes bleeding during your pregnancy, you might need to deliver your baby early.
What happens if the placenta is in the lower part of the uterus?
If the placenta partially or totally covers your cervix (placenta previa) or sits in the lower portion of your uterus, you're at increased risk of placenta accreta.
Can a placenta accreta cause bleeding?
Heavy vaginal bleeding. Placenta accreta poses a major risk of severe vaginal bleeding (hemorrhage) after delivery. The bleeding can cause a life-threatening condition that prevents your blood from clotting normally (disseminated intravascular coagulopathy), as well as lung failure (adult respiratory distress syndrome) and kidney failure. A blood transfusion will likely be necessary.
Is placenta accreta a high risk pregnancy?
Placenta accreta is considered a high-risk pregnancy complication. If the condition is diagnosed during pregnancy, you'll likely need an early C-section delivery followed by the surgical removal of your uterus (hysterectomy).
Can the placenta detach from the uterus?
Typically, the placenta detaches from the uterine wall after childbirth. With placenta accreta, part or all of the placenta remains attached. This can cause severe blood loss after delivery. It's also possible for the placenta to invade the muscles of the uterus (placenta increta) or grow through the uterine wall (placenta percreta).
What is the National Accreta Foundation?
National Accreta Foundation helps connect placenta accreta, increta and percreta patients & families with resources and content of value. October is Accreta Awareness Month and focuses attention on placenta accreta, one of the fastest growing life-threatening complications of pregnancy.
How many births are there in the placenta accreta spectrum?
Placenta accreta spectrum (PAS) is made up of three different levels of invasion: placenta accreta, placenta increta, and placenta percreta. 1 in 272 Births. The estimated incidence of placenta accreta spectrum pregnancies has quadrupled since the 1980s, from 1 in 1250 births to 1 in 272 births. The rates of placenta accreta, increta ...
What is the term for a pregnancy where the placenta attaches too deeply into the wall of the?
Placenta accreta, also known as placenta accreta spectrum (PAS), is a pregnancy condition in which the placenta attaches too deeply into the wall of the uterus. The risk for developing accreta increases with each C-section or uterine surgery.
What are the risk factors for accreta?
Other risk factors include placenta previa, advanced maternal age, multiparity, and curettage. Placenta accreta puts the mother at risk of severe blood loss and other complications. The rates of maternal death, transfusion, prolonged hospital stay and hysterectomy are all increased for women with accreta. Placenta accreta spectrum (PAS) is made up ...
When is Accreta Awareness Month?
October is Accreta Awareness Month and focuses attention on placenta accreta, one of the fastest growing life-threatening complications of pregnancy. Help us spread the word about accreta and get involved in our community efforts to raise awareness.
Is placenta accreta spectrum a condition?
Placenta Accreta Spectrum (PAS) is associated with significant complications. It is imperative that women at risk of developing accreta receive prenatal care at facilities with expertise in diagnosing and treating the condition . See National Accreta Foundation’s Patient FAQ for more information on the latest literature and care recommendations for pregnancies complicated by placenta accreta spectrum.
Who is at Risk for Placenta Accreta?
Placenta accreta, often referred to as simply “accreta,” occurs in about 0.2 percent of all pregnancies. Women who have experienced one or more of the following factors are at a higher risk for this condition:
What is the National Accreta Foundation?
National Accreta Foundation offers information and support for women with placenta accreta. Find a local chapter to meet with other women in your area.
What is the term for the placenta that is attached to the uterus during labor?
During a normal delivery, the placenta detaches from the uterus during the last stage of labor. This can also be referred to as the “afterbirth.”. With accreta, the placenta is tightly attached to the uterine wall and does not separate naturally during delivery.
What happens when the placenta is removed?
This often leads to two major complications: the placenta cannot normally deliver after the baby’s birth, and attempts to remove the placenta can lead to heavy bleeding.
What is the procedure to remove a placenta accreta?
If a placenta accreta is diagnosed before labor, the provider may recommend a Cesarean section. A hysterectomy (the surgical removal of the uterus) may be required after delivery to remove the placenta and end blood loss. Resources and Support Services. The BWH Abnormal Placentation Program.
What is the term for a condition where the placenta sits low in the uterus?
Placenta Percreta: A condition where placenta attaches itself and grows through the uterus and potentially to the nearby organs. Placenta Previa: A condition of pregnancy where the placenta sits low in the uterus, usually over the cervix.
Where does the placenta percreta grow?
Placenta percreta is a condition where placenta attaches itself and grows through the uterus and potentially to the nearby organs (such as the bladder).
What is the definition of placenta accreta?
Definition / general. Abnormal placental adherence to the uterine wall. Placenta accreta: villi implant on the myometrial surface without intervening decidua. Placenta increta: villi extend into the myometrium. Placenta percreta: villi penetrate the entire myometrial thickness and through the uterine serosa.
What happens if you delay placental separation?
Delayed placental separation or manual removal increases the risk for accreta in future pregnancies
Why is invasion through the myometrial wall important?
It is critical that invasion through the myometrial wall is identified in this area to exclude the possibility that the protruding placental tissue was displaced during surgery through the cesarean section incision
Where is the placenta accreta implanted?
Placenta accreta: Chorionic villi implant directly on the surface of the myometrium without intervening decidua. Fibrin and extravillous trophoblast (EVT) are often present between the villi and myometrial fibers, in which case a diagnosis of accreta should still be made, given that intervening decidua is not present.
Which trophoblast normally infiltrates the inner third of the myometrium?
Extravillous trophoblast normally infiltrates the inner third of the myometrium and this is not accreta
What to do if you can't see placental implantation?
If not visible, check medical records for site of placental implantation and sample the area indicated
Where does the placenta extend?
Placenta increta: placenta extends into the uterine wall, usually in a blunt manner; myometrium thinned. Placenta percreta: placenta penetrates through the uterine or lower uterine segment wall; protruding placental tissue on external surface (should be inked) and adherent structures (bladder, bowel) Note where the placenta is implanted (lower ...
What is the preoperative approach to placenta accreta?
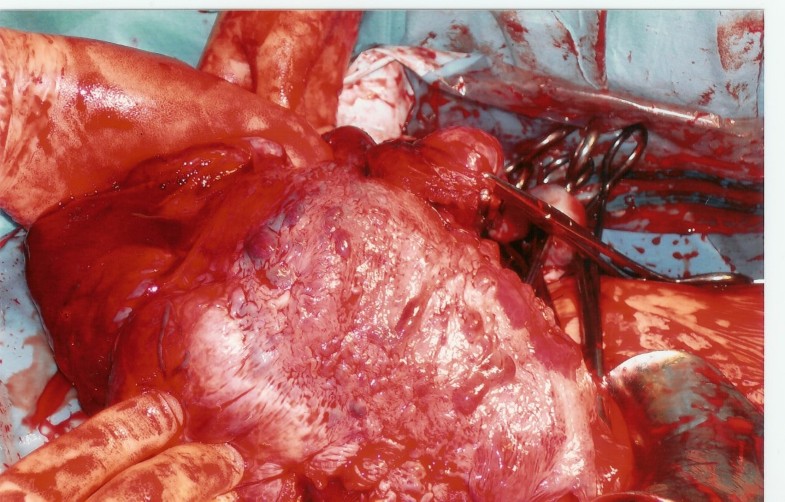
The most generally accepted approach to placenta accreta spectrum is cesarean hysterectomy with the placenta left in situ after delivery of the fetus (attempts at placental removal are associated with significant risk of hemorrhage). Many standard routine operative procedures, including use of standard perioperative antibiotic prophylaxis, remain applicable 68. Many clinicians will rapidly close the uterine incision and then proceed with hysterectomy after verification that the placenta will not spontaneously deliver. Attempts at forced placental removal often result in profuse hemorrhage and are strongly discouraged 24 26. If an antenatal diagnosis of placenta accreta spectrum is uncertain or the preoperative diagnosis is unclear, a period of intraoperative observation for spontaneous uterine placental separation is appropriate as long as preparations for uterine removal are in place. Alternative conservative approaches aimed at fertility preservation have been used and are discussed in subsequent sections.
What is the best time to have a cesarean delivery?
Timing of delivery decisions need to balance maternal risks and benefits with those of the fetus or neonate. It appears that performing a cesarean delivery followed immediately by cesarean hysterectomy before the onset of labor improves maternal outcomes, yet the optimal timing remains unclear 46. A decision analysis suggests that 34 weeks of gestation is optimal given the ability of most large centers to handle neonatal complications at that gestational age and the increased risk of bleeding after 36 weeks 26 49 50 51. Although individual factors are relevant, a window of 34 0/7–35 6/7 weeks of gestation is suggested as the preferred gestational age for scheduled cesarean delivery or hysterectomy absent extenuating circumstances in a stable patient 52. No amniocentesis is necessary at these gestational ages because data regarding pulmonary maturity do not change clinical recommendations for delivery. Earlier delivery may be required in cases of persistent bleeding, preeclampsia, labor, rupture of membranes, or fetal compromise, or developing maternal comorbidities. Waiting beyond 36 0/7 weeks of gestation is not advised because approximately one half of women with placenta accreta spectrum beyond 36 weeks require emergent delivery for hemorrhage. Use of antenatal corticosteroids for lung maturation is appropriate in women with antenatally diagnosed accreta and anticipated delivery before 37 0/7 weeks of gestation and is consistent with current gestational age-based recommendations 53.
What is the most common finding of placenta accreta spectrum on color flow doppler imaging?
The use of color flow Doppler imaging may facilitate the diagnosis. Turbulent lacunar blood flow is the most common finding of placenta accreta spectrum on color flow Doppler imaging. Other Doppler findings of placenta accreta spectrum include increased subplacental vascularity, gaps in myometrial blood flow, and vessels bridging the placenta to the uterine margin 9 28 29.
What is the best way to diagnose placenta accreta?
The primary diagnostic modality for antenatal diagnosis is obstetric ultrasonography. Features of accreta visible by ultrasonography may be present as early as the first trimester; however, most women are diagnosed in the second and third trimesters. Ideally, women with risk factors for placenta accreta spectrum, such as placenta previa and previous cesarean delivery, should be evaluated by obstetrician–gynecologists or other health care providers with experience and expertise in the diagnosis of placenta accreta spectrum by ultrasonography.
What is the rate of placenta accreta?
Rates of placenta accreta spectrum are increasing. Observational studies from the 1970s and 1980s described the prevalence of placenta accreta as between 1 in 2,510 and 1 in 4,017 compared with a rate of 1 in 533 from 1982 to 2002 4. A 2016 study conducted using the National Inpatient Sample found that the overall rate of placenta accreta in the United States was 1 in 272 for women who had a birth-related hospital discharge diagnosis, which is higher than any other published study 4 5 6 7. The increasing rate of placenta accreta over the past four decades is likely due to a change in risk factors, most notably the increased rate of cesarean delivery.
Why is a total hysterectomy required?
In most cases when hysterectomy is necessary, a total hysterectomy is required because lower uterine segment or cervical bleeding frequently precludes a supracervical hysterectomy 55. Regardless, extensive vascular engorgement with challenging anatomy is the rule, and having the most experienced pelvic surgeons involved from the outset is recommended. Careful dissection in the retroperitoneal space with attention to devascularization of the uterine corpus in proximity to the placenta often is required given the overwhelming vascularity and friability of involved tissues. Further technical specifics are beyond the scope of this document. These procedures are preferably performed at a level III or IV center with considerable expertise with placenta accreta spectrum.
What is the placenta accreta spectrum?
ABSTRACT: Placenta accreta spectrum, formerly known as morbidly adherent placenta, refers to the range of pathologic adherence of the placenta, including placenta increta, placenta percreta, and placenta accreta.
What happened before the Placenta Accreta Response Team formed?
Before the Placenta Accreta Response Team formed, placenta accreta surgeries happened ad-hoc at UCH, which is the case at most hospitals capable of handling them at all. Now the same doctors, nurses and support staff would come together as a group to plan and see each case through, then debrief afterwards to understand what went well and where they might improve. In addition to Guntupalli, Bradley Corr, MD, a gynecologic oncologist who trained under Guntupalli as a fellow, joined the CU faculty – and the team – in September 2016.
What is the placenta that hangs on?
It hangs on in one of three ways. Placenta accreta occurs when the placenta binds itself to the uterus wall. Placenta increta involves invasion into the uterus’s muscles. Placenta percreta is when the placenta becomes a sort of malignancy, growing through the uterus wall and, often, into neighboring organs such as the kidney and bowels.
What is the placenta accreta?
The various forms of placenta accreta happen when the life-giving placenta decides to cling to its own existence rather than be birthed with the baby for whom it provided oxygen and removed waste as surrogate in-womb lungs and kidneys. It hangs on in one of three ways. Placenta accreta occurs when the placenta binds itself to the uterus wall. Placenta increta involves invasion into the uterus’s muscles. Placenta percreta is when the placenta becomes a sort of malignancy, growing through the uterus wall and, often, into neighboring organs such as the kidney and bowels.
How much blood did the placenta lose?
The placenta had pushed through the uterus and invaded a quarter-sized patch of the bladder’s outer wall. As Corr and a big OR team worked, she lost half her total blood volume. That was far from the worst the team had seen: a new mother lost 13 liters of blood in a surgery Guntupalli recently led.
What is the most serious form of three life-threatening problems grouped under the umbrella of placenta acc?
In early October, she was diagnosed with placenta percreta, the most serious form of three life-threatening problems grouped under the umbrella of placenta accreta. It’s become much more common as C-sections – a big risk factor – have proliferated, increasing from about one in 4,000 pregnancies in the 1970s to one in about 530 pregnancies today.
Where is Guntupalli practicing?
The two others are practicing in Ohio and Oregon, where they can use the skills they developed under Guntupalli’s guidance to help placenta accreta patients far from Colorado.
When did Guntupalli join CU?
The day before Guntupalli joined the CU faculty in August 2012, a placenta accreta patient had died. There were extenuating circumstances: as a Jehovah’s Witness, she declined a blood transfusion despite such surgeries involving 2 liters to 5 liters of blood loss, on average, and often much more.
