What is the medically needy program?
What is the Medically Needy Program? A Medicaid program for people who have too much income or assets are over the limits for Medicaid, Some people call it the “share of cost” program. The Department of Children & Families (DCF) determines eligibility for the Medically Needy Program.
What is aid to families with Dependent Children (AFDC)?
Aid to Families with Dependent Children (AFDC) was established by the Social Security Act of 1935 as a grant program to enable states to provide cash welfare payments for needy children who had been deprived of parental support or care because their father or mother was absent from the home, incapacitated, deceased, or unemployed.
What are medically needy individuals for Medicaid?
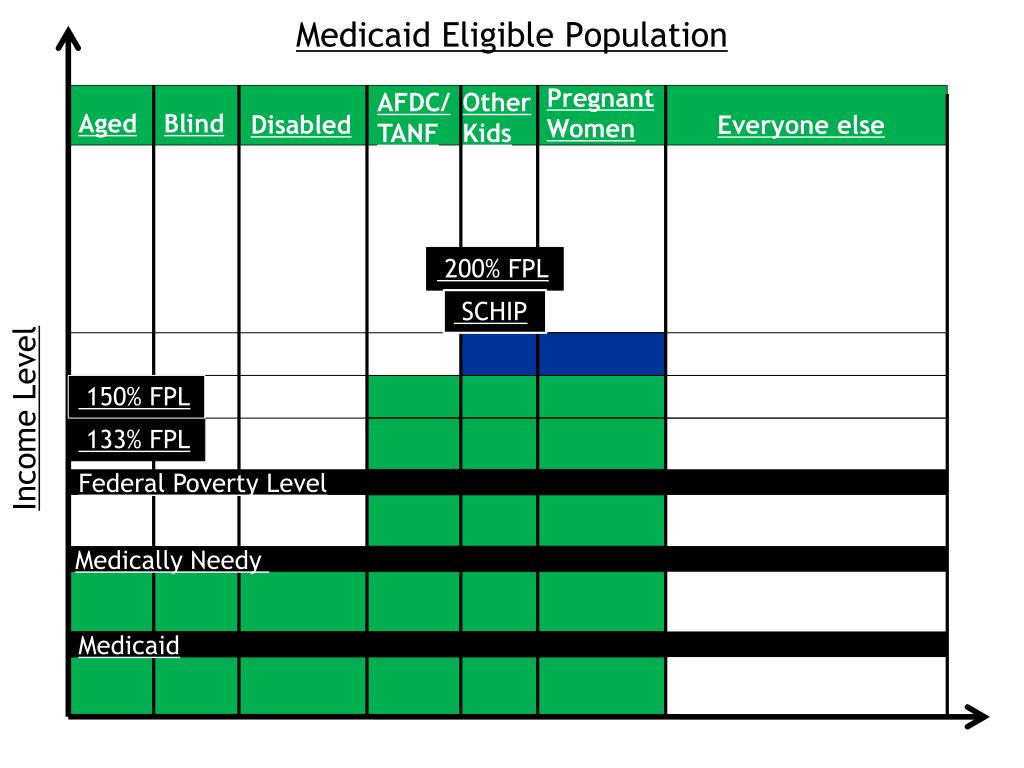
In some states, those individuals may still qualify for Medicaid if they have significant medical expenses that reduce their income below a certain level, through what are called "medically needy" programs. All states have the option of covering so-called medically needy individuals, but not all do.
How many states have AFDC programs?
All 50 states, the District of Columbia, Guam, Puerto Rico, and the Virgin Islands operated an AFDC program. States defined "need," set their own benefit levels, established (within federal limitations) income and resource limits, and administered the program or supervised its administration.
What is the purpose of TANF?
What is the PRWORA program?
What was the purpose of Section 1115 of the Social Security Act?
What is AFDC in social security?
How long can you be on TANF?
Which states have AFDC?
See 3 more
About this website

What is the definition of medically needy?
The Medicaid medically needy option extends Medicaid eligibility to individuals with high medical expenses whose income exceeds the maximum limit for other pathways, but who would otherwise be eligible for Medicaid. As of 2022, 34 states have a Medicaid medically needy program in place.
What does Florida Medically Needy cover?
Health insurance premiums • Medical bills that will not be paid by health insurance or any other source. Co-pays for medical bills. Medical services prescribed by a doctor. Transportation by ambulance, bus or taxi to get medical care.
What is the main difference between AFDC and TANF?
The main difference between the two schemes is that, contrary to the TANF, the AFDC was an entitlement program. This means that it guaranteed benefits to all eligible individuals whose income and assets were below the eligibility levels.
Does Florida Medically Needy cover prescriptions?
Medicaid pays for medical costs such as prescription drugs, hospital bills and doctor bills. You can only get Medicaid if you have very little income. Under medically needy Medicaid, your medical bills can help you qualify.
What is the maximum income to qualify for free health care in Florida?
Who is eligible for Florida Medicaid?Household Size*Maximum Income Level (Per Year)1$18,0752$24,3533$30,6304$36,9084 more rows
Does Florida Medically Needy cover dental?
Dental: Provides all Medicaid dental services for children and adults. All people on Medicaid must enroll in a dental plan.
Why did they get rid of AFDC?
But by evaluating success in terms of declining welfare caseloads instead of declining child poverty, these welfare-to-work programs led to repeal of the entire AFDC program in 1996.
Do you get cash assistance twice a month?
Cash Assistance Benefits. FA and SNA provide a cash benefit twice per month that can be used for food, utilities and housing expenses. If you are eligible for FA, you can only receive benefits for a lifetime total of five years (60 months).
What happened to the AFDC?
Congress created the TANF block grant through the Personal Responsibility and Work Opportunity Reconciliation Act (PRWORA) of 1996, as part of a federal effort to “end welfare as we know it.” TANF replaced AFDC, which had provided income support in the form of cash assistance to families with children in poverty since ...
What are the income limits for Medicaid 2022 in Florida?
In 2022, the medically needy income limit in FL is $180 / month for a single applicant and $241 / month for a married couple. The “spend-down” amount is the difference between one's monthly income and the medically needy income limit.
What is the income limit for Florida Blue?
By Florida BlueIf you're a single adult with no kids and your annual income is:If you're a family of four and your annual household income is:$12,760 to $19,140$25,520 to $39,300$19,141 to $51,040$39,301 to $104,800More than $51,040More than $104,800Apr 1, 2021
Is needy medicine legit?
Don't be fooled — NeeedyMeds never charges for our information or help. We are a 501(c)(3) Non-Profit and will always provide you with accurate information at no cost. You can also call our toll-free helpline at 800-503-6897. We also have a list of local programs that either don't charge or charge for a small fee.
What does Florida Medicaid pay for?
Medicaid services may include: physician, hospital, family planning (birth control, pregnancy and birth care), home health care, nursing home, hospice, transportation, dental and visual, community behavioral health, services through the Child Health Check-Up program, and other types of services.
What does Florida Medicaid waiver cover?
Provides adult day health care, case management, homemaker, respite, attendant care, intermittent and skilled nursing, medical equipment and supplies, occupational therapy, personal care, physical therapy, respiratory therapy, speech therapy, transportation, adult companion, assisted living, behavior management, ...
Are there copays with Florida Medicaid?
(1) The agency shall require, subject to federal regulations and limitations, each Medicaid recipient to pay at the time of service a nominal copayment for the following Medicaid services: (a) Hospital outpatient services: up to $3 for each hospital outpatient visit.
What is the difference between categorically needy and medically needy?
MEDICALLY NEEDY MEDICAID recipients are those who would be eligible for Categorically Needy except that their income and/or assets are too high. However, even though their resources are too high for Categorically Needy Medicaid eligibility, they cannot afford to pay their medical bills.
Aid to Families With Dependent Children: An Overview, October 1977
Istered, who 1s ehglble for aid, and how much aid ehglble persons shall receive As long as It 1s complying w:th its approved plan, the State IS
Aid to Families with Dependent Children The Baseline | ASPE
Introduction The term “welfare” has long been identified with the Aid to Families with Dependent Children (AFDC) program. While the AFDC program was an important component of the safety net for low-income families with children, there was a near universal consensus that the program contained serious flaws. In August 1996, the Personal Responsibility and Work Opportunity Reconciliation Act ...
Aid to Families With Dependent Children: Characteristics of Recipients ...
-The average size of AFDC families has been de- creasing for a decade. In 1979, the average number of children in AFDC families was not much different
Welcome to Benefits.gov | Benefits.gov