How is an ETV surgery performed?
In this procedure, surgeons use a tiny camera called an endoscope to enter the ventricles in the brain. They then make a small opening in one of the ventricles, which relieves the pressure buildup by allowing fluid to flow again. The procedure is called an ETV, or "endoscopic third ventriculostomy."
How long does it take to recover from ETV?
Avoid baths, hot tubs, and swimming pools for at least 2 weeks after your surgery. Don't use a hair dryer, creams, ointments, or hair products on your incision until it's completely healed. This takes about 6 weeks.
How long does an ETV last?
ETV failure occurred in 51 patients, with a median time to failure of 2 months (range, 0-124 months). Although the majority (86%) of ETV failures occurred within 2 years postoperatively, failure was noted in 3 cases between 5 and 10 years after intervention, including in 1 patient at a 124-month follow-up.
Is ETV a major surgery?
ETV surgery is a relatively short procedure that varies slightly depending upon the anatomy inside your brain.
How successful is ETV surgery?
Duru et al. documented their experience with ETV in 51 children under the age of 16; they reported an overall success rate of 80% for all etiologies and ages [14]. Their success rate was 56.2% (9/16) in patients < 6 months of age, 88.9% (16/18) in 6–24 months of age, and 94.1% (16/17) in > 24 months.
Who is a good candidate for ETV?
The preoperative findings of lethargy and transependymal flow statistically correlated with success. This suggests that the best candidates for ETV are those with a relatively acute elevation of intracranial pressure.
Is ETV better than a shunt?
There are several benefits of an ETV versus a ventriculoperitoneal shunt. Compared to a shunt, there are no implanted foreign bodies, fewer incisions and an overall lower long term complication rate. This means there is less discomfort, a lower infection rate, and less time in the hospital.
What can I expect after ETV surgery?
Nausea and vomiting: Nearly 50% of patients undergoing an ETV experience nausea and vomiting for hours to several days after the procedure. Management is with IV fluids and bed rest. Headaches: Air and blood in the ventricles can cause headaches of varying severity. Headaches are managed with routine analgesics.
What happens when ETV fails?
Usually, if a patient initially tolerates an ETV and fails in a delayed fashion, this is due to the reclosure of the stoma. The stoma itself may close or stenosis due to scarring or gliosis, causing the floor of the third ventricle to appear intact either by ventriculoscopy or imaging.
How long does an ETV procedure take?
The procedure takes around 1 hour. There's less risk of infection after ETV than with shunt surgery. However, as with all surgical procedures, there are some risks. Read more about the complications of hydrocephalus.
Is ETV surgery safe?
INTRODUCTION. Although endoscopic third ventriculostomy (ETV) is a safe procedure, a variety of complications have been reported, mostly related with the surgical procedure. The overall morbidity rate reported is 8.5%, ranging from 0 to 31.2%, and the overall rate of permanent morbidity is 2.38%6,7,19,25).
Is endoscopic third ventriculostomy safe?
The mean follow-up lasted 17.9 months. No postoperative complications were observed. Conclusion: ETV seems to be a safe and efficient alternative to shunt for chronic hydrocephalus with obstruction; the clinical improvement is usual and ventricular size decreases slightly.
What are the possible complications for ETV?
The most frequent intraoperative complications of ETV are hemorrhage (the most severe being due to basilar rupture) and injury of neural structures. In the immediate postoperative period, hematomas, infections, and cerebrospinal fluid leaks may present. Morbidity can be neurological and/or hormonal.
Is ETV better than shunt?
There are several benefits of an ETV versus a ventriculoperitoneal shunt. Compared to a shunt, there are no implanted foreign bodies, fewer incisions and an overall lower long term complication rate. This means there is less discomfort, a lower infection rate, and less time in the hospital.
What happens when ETV fails?
Usually, if a patient initially tolerates an ETV and fails in a delayed fashion, this is due to the reclosure of the stoma. The stoma itself may close or stenosis due to scarring or gliosis, causing the floor of the third ventricle to appear intact either by ventriculoscopy or imaging.
How long does an ETV procedure take?
The procedure takes around 1 hour. There's less risk of infection after ETV than with shunt surgery. However, as with all surgical procedures, there are some risks. Read more about the complications of hydrocephalus.
What is it?
ETV is an abbreviation that stands for endoscopic third ventriculostomy. An ETV is a highly specialized treatment performed by Rochester Neurosurgery Partners for hydrocephalus (extra fluid in the brain causing pressure). This treatment can be an alternative to the placement of a shunt (see ventriculoperitoneal shunt) but is only performed in a select group of patients. This technique uses cameras navigated through the brain to create a small hole which relieves the increased pressure. The procedure is most common performed for patients with aqueductal stenosis; a blockage that prevents the outflow of cerebrospinal fluid (water that bathes the brain).
How is it done?
The patient goes to sleep with general anesthesia. A small dime-sized hole in the skull, usually in the front behind the hairline. Next a small camera is inserted and navigated to the part of the brain that holds cerebrospinal fluid. An opening is made through normal brain tissue which allows this fluid to drain and get reabsorbed by the body. This opening does not normally result in any harmful permanent effects. Once the flow is diverted, a titanium cover is placed over the hole in the skull and the skin is closed. The procedure usually takes less than one hour to complete
What is the success rate?
With good patient selection, an ETV can be very effective treatment for hydrocephalus. For patients with obstructive hydrocephalus, some studies show that 70% get better. This treatment does not prevent the future use of a shunt if the ETV fails to cure the hydrocephalus.
What is special about the way we deliver this treatment?
Rochester Neurosurgery Partners use the most up-to-date technology to perform these operations. A high-definition camera is used which allows excellent visualization of brain structures and assures that the procedure is performed correctly.
What is the procedure used to create a small hole in the brain?
This technique uses cameras navigated through the brain to create a small hole which relieves the increased pressure. The procedure is most common performed for patients with aqueductal stenosis; a blockage that prevents the outflow of cerebrospinal fluid (water that bathes the brain).
What happens after ETV?
The most common complications after an ETV are fever and bleeding. The light from the camera and heat from the instruments can heat the fluid in the brain causing a fever which usually resolves within a few hours. Sometimes when the brain is perforated to allow diversion of cerebrospinal fluid, blood vessels are damaged causing bleeding. The chances of a catastrophic bleed are very low. Other potential complications after ETV are short-term memory loss or endocrinologic disorders which occur infrequently and usually get better over time.
What is the opening in the skull?
An opening is made through normal brain tissue which allows this fluid to drain and get reabsorbed by the body. This opening does not normally result in any harmful permanent effects. Once the flow is diverted, a titanium cover is placed over the hole in the skull and the skin is closed.
What is a PST appointment?
Presurgical Testing (PST) Before your surgery, you will have an appointment for presurgical testing (PST). Depending on your age, your testing can take place in a variety of places. The date, time, and location of your PST appointment will be printed on the appointment reminder from your surgeon’s office.
What is ETV surgery?
ETV is a surgery to drain extra cerebrospinal fluid (CSF) from your brain. CSF is the fluid that surrounds your brain and spinal cord. It’s made in the ventricles (hollow spaces) inside your brain.
How long after surgery can you shower?
Your doctor or nurse will tell you when it’s safe to shower after your surgery. Keep your incision dry for 5 days following your surgery. If your doctor or nurse says it’s okay to shower before then, wear a shower cap to keep your incision dry. When you wash your hair, use a gentle shampoo, such as baby shampoo.
How long does it take for staples to be removed after surgery?
The sutures or staples in your incision will be removed 7 to 10 days after your surgery. They may need to stay in longer if you have had this surgery before. Your doctor or NP will remove them during your follow-up visit at the clinic.
What is the most common breathing disorder that causes a person to stop breathing for short periods of time while sleeping?
Sleep apnea is a common breathing disorder that causes a person to stop breathing for short periods of time while sleeping. The most common type is obstructive sleep apnea (OSA). With OSA, the airway becomes completely blocked during sleep. It can cause serious problems during and after surgery.
How long do you stay in the hospital?
Most people stay in the hospital 1 night, but this will depend on your recovery.
What happens if you drink alcohol after surgery?
These include bleeding, infections, heart problems, and a longer hospital stay.
What is ETV used for?
Medical uses. The ETV procedure is used as an alternative to a cerebral shunt mainly to treat certain forms of noncommunicating obstructive hydrocephalus (such as aqueductal stenosis), but since the ETV was introduced as an accepted treatment modality the range of etiologies for which it is used has grown significantly.
What is ETV in neurosurgery?
In most countries and neurosurgical centres, the ETV procedure is part of the basic neurosurgery training program. For the sake of teaching and practicing, various simulation models have been developed. Virtual reality simulators, and synthetic simulators. This allows neurosurgical trainees to practice skills in a low-risk environment. Educators can select either a virtual reality simulator or a physical model for the training of residents, the selection should be based on educational objectives. Where training focused on anatomy and using anatomical landmarks for decision making may better be aided with virtual reality model, the focus on familiarizing the resident with endoscopic equipment and developing manual dexterity may be better learned on a physical model. The technical skill and competency of a trainee can be evaluated using the Neuro-Endoscopic Ventriculostomy Assessment Tool (NEVAT).
What is the procedure for a third ventriculoscopy?
Endoscopic third ventriculostomy ( ETV) is a surgical procedure for treatment of hydrocephalus in which an opening is created in the floor of the third ventricle using an endoscope placed within the ventricular system through a burr hole. This allows the cerebrospinal fluid to flow directly to the basal cisterns, bypassing the obstruction.
What are the complications of endoscopic third ventriculostomy?
Complications of ETV include hemorrhage (the most severe being due to basilar artery rupture), injury to neural structures (e.g. hypothalamus, pituitary gland or fornix of the brain ), and late sudden deterioration. Infection, hematoma, and cerebrospinal fluid leaks may present in the direct postoperative period.
What is the best treatment for hydrocephalus?
The surgical treatment options for hydrocephalus are, as previously mentioned, implantation of a cerebral shunt and ETV. Especially in the youngest age group (younger than two years of age) it remains uncertain what is the superior treatment modality. Currently, a large international, multicenter study is conducted to address this issue. Patients under the age of two, diagnosed with aqueductal stenosis without a history of preterm birth or other associated brain anomalies are being included (International Infant Hydrocephalus Study).
What are the complications of ETV?
Complications of ETV include hemorrhage (the most severe being due to basilar artery rupture), injury to neural structures ( e.g. hypothalamus, pituitary gland or fornix of the brain ), and late sudden deterioration. Infection, hematoma, and cerebrospinal fluid leaks may present in the direct postoperative period.
When it is not possible to perform an ETV for different reasons, an alternative treatment is?
When it is not possible to perform an ETV for different reasons, an alternative treatment is opening the lamina terminalis anterior to the third ventricle. The effectiveness of this approach is not certain.
What is the procedure for a third ventriculoscopy?
Endoscopic third ventriculostomy is a surgical procedure offered to children and adults diagnosed with obstructive or non-communicating hydrocephalus. Shunting, or using a small silicone tube to carry the cerebrospinal fluid (CSF) to a different body cavity for reabsorption, is the most common treatment for hydrocephalus.
What is endoscopic surgery?
Endoscopic means that the surgery is performed with the use of an endoscope. An endoscope is a thin tube that has a strong light, a powerful magnifying lens and an opening where tiny instruments are passed.
Where does cerebrospinal fluid flow?
The cerebrospinal fluid may then flow from the lateral to the third ventricle and from the third ventricle through the new opening to the normal fluid chambers below the base of the brain. The cerebrospinal fluid then flows up and over the surface of the brain where it is reabsorbed into the bloodstream.
How long after a child's shunt surgery can they go to school?
Wash your child's incision every day with a mild shampoo or soap and water. Your child may return to school or daycare 10-14 days after surgery, depending on how they feel. Watch your child for any signs of hydrocephalus (the same symptoms that prompted the surgery). (See Shunt Malfunction for signs of hydrocephalus.)
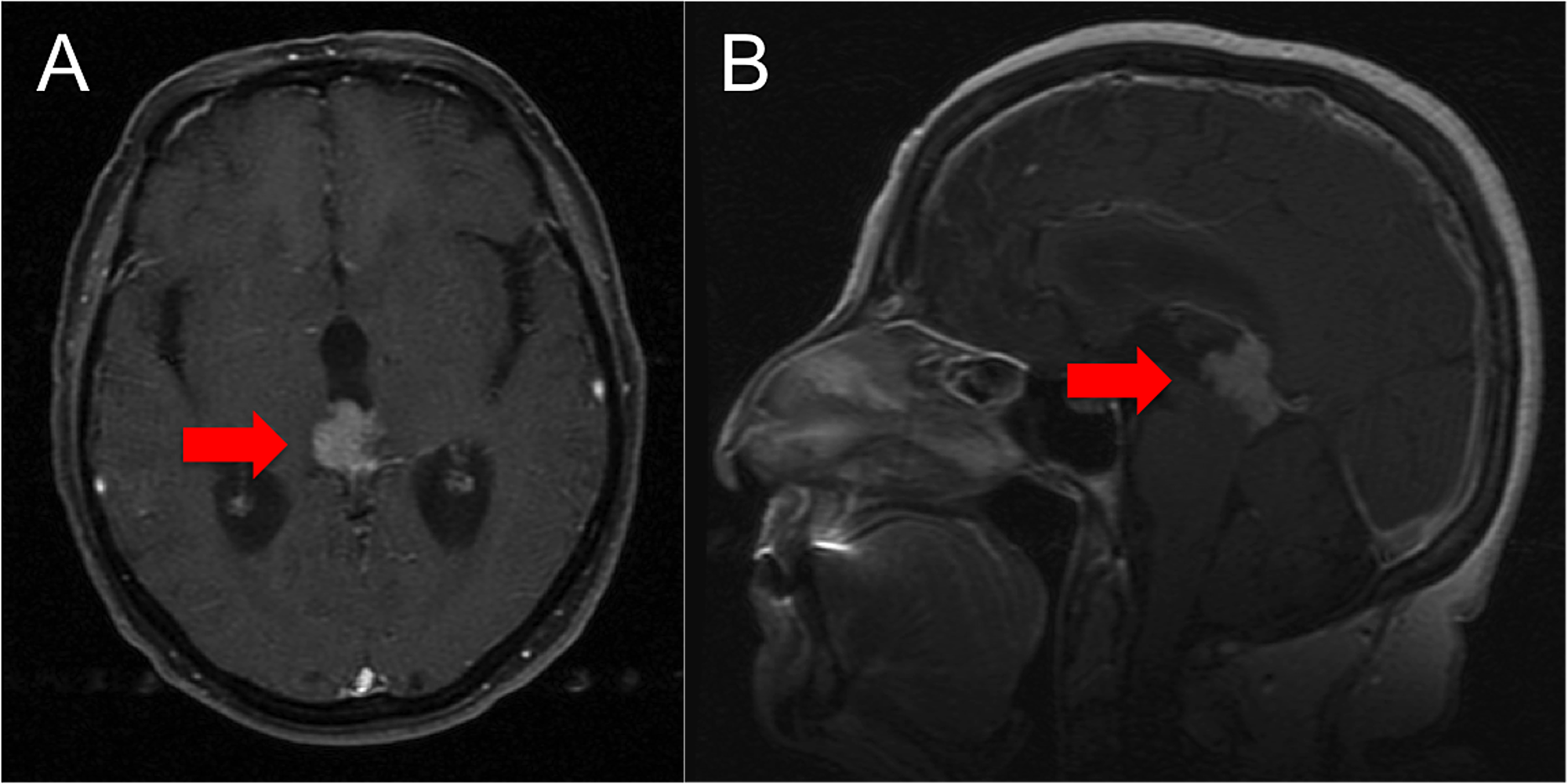
How long does it take for a child to see a doctor after a brain surgery?
Your child will need to see the doctor in 7-10 days after the procedure to have their wound checked. They will also need to have a motion MRI of the brain before this visit. This x-ray allows the doctor to check the opening made during surgery.
Is a third ventriculostomy a man made procedure?
While shunts may be lifesaving, they are man-made devices and may fail for a variety of reasons. Endoscopic third ventriculostomy is an alternative surgical procedure that creates a bypass for the cerebrospinal fluid in the head that eliminates the need for a shunt.
How long does a child stay in the hospital after a PACU?
After your child is awake and alert, they will go to their hospital room. Children typically stay in the hospital for 2-3 days and can go home once the doctor feels the surgery was effective and they are: Drinking well.
What is the choroid plexus?
The choroid plexus is vascular tissue within the ventricles of the brain and is the source of CSF production. The fluid then passes normally through the opening made during the ETV and into the space surrounding the surface of the brain. Not everyone is a candidate for ETV/CPC treatment. ETV/CPC is a very technical surgery ...
Why do most ventriculostomy patients remain shunt dependent?
Doctors attribute failed procedures to a patient’s inability to absorb the CSF or a block in the subarachnoid pathways. Because CSF reabsorption pathways might require some time to normalize following ventriculostomy, it may not be possible to determine success immediately after the operation.
What is the third treatment option for ETV?
The third treatment option involves an ETV with the addition of a procedure called choroid plexus cauterization (CPC). This treatment is primarily used in children under 2.
What is the procedure for hydrocephalus?
Endoscopic Third Ventriculostomy (ETV) A second treatment option for hydrocephalus is a surgical procedure called endoscopic third ventriculostomy (ETV). This is typically used for children over the age of 2 with non-communicating hydrocephalus; hydrocephalus caused by a blockage in the brain like aqueductal stenosis.
How successful is ETV?
The success rate for ETV or ETV/CPC depends upon patient factors such as age, cause of hydrocephalus, and whether there is scarring in the fluid space below the floor of the third ventricle (subarachnoid pathway). For some patients, the chance for success of the ETV may be up to 90%; however, for others, ETV or ETV/CPC may not be recommended because the chances for success are sufficiently low.
Where does the endoscope go to get CSF?
With the use of a camera, the endoscope then passes down into the third ventricle and punctures the membrane on the floor of the third ventricle. This creates an alternative pathway for CSF to flow out of the ventricles and around the brain.
How many chances of success for ETV?
For some patients, the chance for success of the ETV may be up to 90%; however, for others, ETV or ETV/CPC may not be recommended because the chances for success are sufficiently low. The results of ETV are determined by assessing clinical signs of raised intracranial pressure, head circumference measurements, and fontanelle tension, ...
