An outpatient department visit/use/event is any visit made during the person's reference period to a hospital outpatient department, such as a unit of a hospital, or a facility connected with a hospital, providing health and medical services to individuals who receive services from the hospital but do not require hospitalization overnight.
What's the difference between inpatient and outpatient?
The Differences Between Inpatient and Outpatient
| Inpatient | Outpatient |
| Inpatient entails being admitted into a ... | Outpatient refers to medical services of ... |
| Inpatient care is usually provided for m ... | Outpatient care is usually provided in l ... |
| Inpatient care involves more costs and h ... | Outpatient care usually entails fewer co ... |
What is considered outpatient treatment?
What is considered outpatient treatment? Outpatient treatment is generally described as mental health or medical care that you receive that does not require more than a 24-hour hospitalization period. Even patients who spend overnights in the hospital but return home within 24 hours may be considered to be a part of outpatient treatment.
What to expect in outpatient rehab?
What to Expect in Outpatient Rehab
- Enrollment in Our Program
- Quality Outpatient Programs. To develop a treatment plan customized for your individual needs, our treatment team will perform a full medical assessment.
- Clinical Intake Assessment
Are visitors allowed during inpatient treatment?
Visiting a loved one during treatment helps promote emotional healing, boost morale, and build trust, both for the individual in treatment and their loved ones. Many inpatient drug rehab centers allow residents to have visits from friends or family members.
What are examples of outpatient services?
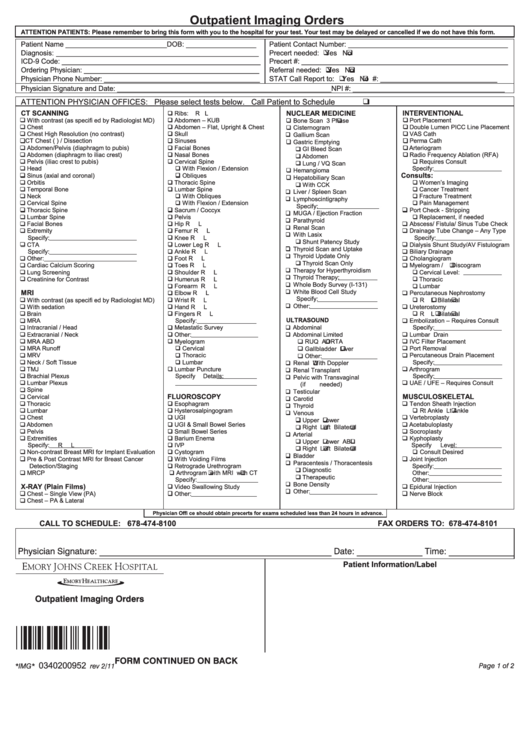
Outpatient care, sometimes called ambulatory care, is any service you receive without being admitted to a hospital or for a stay shorter than 24 hours. Some examples of outpatient services are X-rays and other imaging procedures, minor surgeries, some cancer treatments, and routine physicals.
What is the difference between inpatient and outpatient visit?
The basic difference between inpatient and outpatient care is that inpatient care requires a patient to stay in a hospital overnight and outpatient does not. If you receive inpatient care, you will be monitored by a healthcare team in a hospital throughout your treatment and recovery.
What means outpatient services?
Outpatient services are medical procedures or tests that can be done in a medical center without an overnight stay. Many procedures and tests can be done in a few hours. Outpatient services include: Wellness and prevention, such as counseling and weight-loss programs. Diagnosis, such as lab tests and MRI scans.
What happens when you are an outpatient?
You're an outpatient if you're getting emergency department services, observation services, outpatient surgery, lab tests, X-rays, or any other hospital services, and the doctor hasn't written an order to admit you to a hospital as an inpatient.
Why is outpatient care better than inpatient?
Outpatient surgeries are usually much less complicated than inpatient surgeries. This means that patients are discharged home after their procedure. Inpatient surgeries are more complex thus, patients must stay in the hospital to be monitored by health professionals.
Why is outpatient care important?
With outpatient services, patients recover at home instead of staying in the hospital. Patients who receive care in an outpatient setting are at lower risk for hospital-acquired infections. Most payors reimburse hospitals more for outpatient services than for inpatient care.
What are the five main types of outpatient services?
What are the five main types of hospital-based outpatient services?...Terms in this set (25)Wellness and Prevention (counseling)Diagnosis (lab tests)Treatment (surgery)Rehabilitation (PT)
What is considered an outpatient facility?
Outpatient care is defined as hospital or medical facility care that you receive without being admitted or for a stay of less than 24 hours (even if this stay occurs overnight). Outpatient care also includes any health care services that you receive while at the facility.
Where are the majority of outpatient services performed?
primary care officesThe majority of outpatient visits for US adults with diabetes, as well as visits in which diabetes was a patient reason for visit, occurred in primary care offices, followed by specialist offices.
How long do you stay after outpatient surgery?
In general, most patients go home between one and four hours after outpatient surgery.
What is the difference between outpatient and observation?
When the doctor orders observation or tests to help with the diagnosis, you remain outpatient until inpatient admission. Outpatient is when you get care without admission or have for a stay of fewer than 24 hours, even if overnight. Health services you get at a facility can be outpatient care.
What is health insurance outpatient?
An outpatient treatment is when you receive a medical treatment without being admitted into a hospital. The treatment could comprise of Doctor consultations, various diagnostic tests and medicines.
What is an inpatient and outpatient?
Outpatient. Definition. When the patient has been formally admitted to a hospital, either more than a day (at least 24 hours) or an extended period, the patient is called an inpatient.
What does inpatient mean in medical terms?
What is an inpatient? In the most basic sense, this term refers to someone admitted to the hospital to stay overnight, whether briefly or for an extended period of time. Physicians keep these patients at the hospital to monitor them more closely.
What does outpatient in a bed mean?
Purpose of Outpatient in a Bed The OPIB designation provides a way to generally classify patients occupying acute care beds in a hospital without medical necessity.
Does inpatient mean overnight?
Inpatient care tends to be directed toward more serious ailments and trauma that require one or more days of overnight stay at a hospital. Health insurance plans require you to be formally admitted into a hospital for a stay for a service to be considered inpatient.
What is the difference between inpatient and outpatient care?
The difference between inpatient versus outpatient care matters for patients because it will ultimately affect your eventual bill. Outpatient care involves fees related to the doctor and any tests performed. Inpatient care also includes additional facility-based fees.
What is an inpatient?
What is an inpatient? In the most basic sense, this term refers to someone admitted to the hospital to stay overnight, whether briefly or for an extended period of time. Physicians keep these patients at the hospital to monitor them more closely.
What is an annual exam?
An annual exam with your primary care physician is an example of outpatient care, but so are emergent cases where the patient leaves the emergency department the same day they arrive.
Is a primary care physician considered an outpatient?
Primary care physicians have traditionally been considered outpatient providers, while specialists are thought of as inpatient physicians. But that’s really an oversimplification, particularly when you consider that hospitalists bridge the gap by providing general medical care to inpatients.
What is an outpatient visit?
Outpatient visit. definition. Outpatient visit means those hospital - based outpatient services which are billed on a single claim form. Outpatient visit means those hospital - based outpatient services which are billed on a single UB-92 claim form, and which occur within 72 hours of initiation of service, with exceptions as noted in paragraph “m.”.
How to determine outpatient visit days?
Outpatient visit days will be determined by counting one visit day for each calendar day that a patient visits the outpatient department.
What are the conditions that are not considered outpatient visits?
Outpatient visit and inpatient daylimits do not apply to the following conditions: serious emotional disturbances of a child (as defined in Section 1374.72 (e) of the California Health and Safety Code), schizophrenia, schizoaffective disorder, bipolar disorder (manic-depressive illness), major depressive disorders, panic disorder, obsessive-compulsive disorder, pervasive developmental disorder or autism, anorexia nervosa, and bulimia nervosa.
What does "outpatient" mean in the military?
Outpatient status means the status of a servicemember assigned to (a) a military medical treatment facility as an outpatient; or (b) a unit established for the purpose of providing command and control of members of the Armed Forces receiving medical care as outpatients.
How long does an insured person have to stay in a hospital?
Inpatient care means treatment for which the insured person has to stay in a hospital for more than 24 hours for a covered event.
What is outpatient treatment?
Outpatient treatment means mental health or substance abuse treatment services rendered to a person as an individual or part of a group while not confined as an inpatient. Such treatment shall not include services delivered through a partial hospitalization or intensive outpatient program as defined herein.
What is inpatient hospital?
Inpatient hospital services means any health care service provided to a patient who has been admitted to a hospital and is required to remain in that hospital overnight, but does not include any secure forensic mental health services;
Why do patients feel more comfortable in outpatient clinics?
On the other hand, some patients may feel more comfortable at a hospital outpatient clinic, simply because of its institutional setting. Patients may feel more comfortable knowing the outpatient clinic they are visiting is connected to a larger in-house network of other departments and providers. Where a patient requires several different services, all of which may be provided by the hospital system, there may also be an ease of sharing of records and interdepartmental communication. Patients may also prefer visiting an outpatient clinic because they may be more easily transferred to the hospital should an emergency arise.
Why do people go to private medical offices?
Other reasons patients may seek treatment at private medical offices compared to a hospital outpatient center include ease of access and parking, or simply the personal touch of a private practice , when compared to the often institutional setting of a hospital outpatient center.
Why do patients go to private clinics?
A patient who visits a private practice will also likely spend far less out-of-pocket than those who choose a hospital- based clinic . The fees at a hospital outpatient clinic can be more than four times higher than in a private office, which are then passed on to patients through higher co-insurance or co-pay responsibilities. Not only are the fees higher, hospital-based clinics require two co-pays, as there are two separate components of payment. Incidentally, cost-savings is one of the main reasons commercial insurance companies and Medicare often require their insureds visit a private practice, as in the MRI example cited above.
Can you go to a private doctor for a MRI?
Patients occasionally have a choice to go to either a hospital outpatient center or a private physician's office for certain non-emergency medical procedures, like hyperbaric oxygen therapy (HBOT). This is unlike certain other procedures, including an MRI, for instance, where most commercial insurance companies and Medicare require their insureds visit a private diagnostic center, rather than a hospital.
What is an office visit?
An office visit is designed to discuss new or existing health issues, concerns, worries or symptoms. Your provider may order tests, prescribe medication, refer you to a specialist or provide advice and education. Office visits are covered by a standard insurance co-pay or deductible.#N#“We take care of people as individuals. The care involved even for the same problem is often very different. It’s not unusual for two appointments to be on the schedule for ‘headache,’ and one will be a migraine episode, while the other is related to underlying depression and insomnia. We allot the necessary amount of time to come up with a treatment plan specific to each person’s case,” Dr. Kemp says.
What is preventive care?
A preventive visit is a yearly appointment intended to prevent illnesses and detect health concerns early, before symptoms are noticeable. Preventive visits could be an annual physical, well-child exam, Medicare wellness exam or welcome to Medicare visit. Insurance companies are required to cover preventive care services at no cost to patients. During your appointment, you’ll review your overall health and well-being. Depending on your age, services may include: 1 Complete physical exam 2 Immunization review and update 3 Age-appropriate heart disease screenings (blood pressure, blood glucose and cholesterol tests) 4 Cancer risk screenings (pelvic exam, Pap smear, prostate and colorectal screenings) 5 Sexually-transmitted disease testing 6 Evaluation for signs of depression 7 Alcohol, depression, obesity and tobacco counseling
What is the official source of CPT code information and guidelines?
AMA is the official source of CPT® code information and guidelines. This website provides information on the revised E/M codes and provides a learning module to assist physicians and their staff in navigating those changes.
When was the CPT code 99202 revised?
On Jan. 1, 2021, revised office/outpatient visit E/M CPT® codes (99202-99215) and associated documentation went into effect. The revised codes are the culmination of collaboration among the Centers for Medicare & Medicaid Services, American Medical Association and other medical specialty societies, including IDSA. The changes to these codes were the start of a multi-year, multi-phase AMA project to revise nearly all the CPT® E/M code set. The revisions are long overdue, as the codes were established nearly 20 years ago and, in that time, patient care along with how to document that care has changed. Reducing provider burden by decreasing charting requirements was also a primary driver for the revision of the codes.
How long does an outpatient visit take?
Usually, the presenting problem (s) are minimal. Typically, 5 minutes are spent performing or supervising these services.
What is the E/M code for outpatient visits?
Some of the most commonly reported E/M codes are 99201-99215, which represent office or other outpatient visits. In 2020, the E/M codes for office and outpatient visits include patient history, clinical examination, and medical decision-making as the key components for determining the correct code level, and that is the version ...
What is the coding code for outpatient E/M in 2021?
For information about coding office and other outpatient E/M services in 2021, Please see 99202-99215: Office/Outpatient E/M Coding in 2021.
How to get reimbursement for 99211?
Don’t underestimate the importance of documentation. Documentation is essential when requesting reimbursement for 99211 visits. The care provider must document details including the reason for the encounter, which may include educational services as well as evaluation of the patient’s condition with management directed by the physician. You also must have documentation to show that the supervising provider was in the office at the time of the visit. Documentation might be a statement indicating that the nurse was working under a physician in the office, a copy of the physician’s schedule that shows the physician was in the office at the time of the nurse visit, or a statement by the physician with signature and date.
How long is a minor surgical procedure?
A minor surgical procedure is a procedure with a global period of 0 days or 10 days on the Medicare Physician Fee Schedule (MPFS). Many payers other than Medicare use this definition, as well. The global period refers to the length of time the global surgical package applies.
