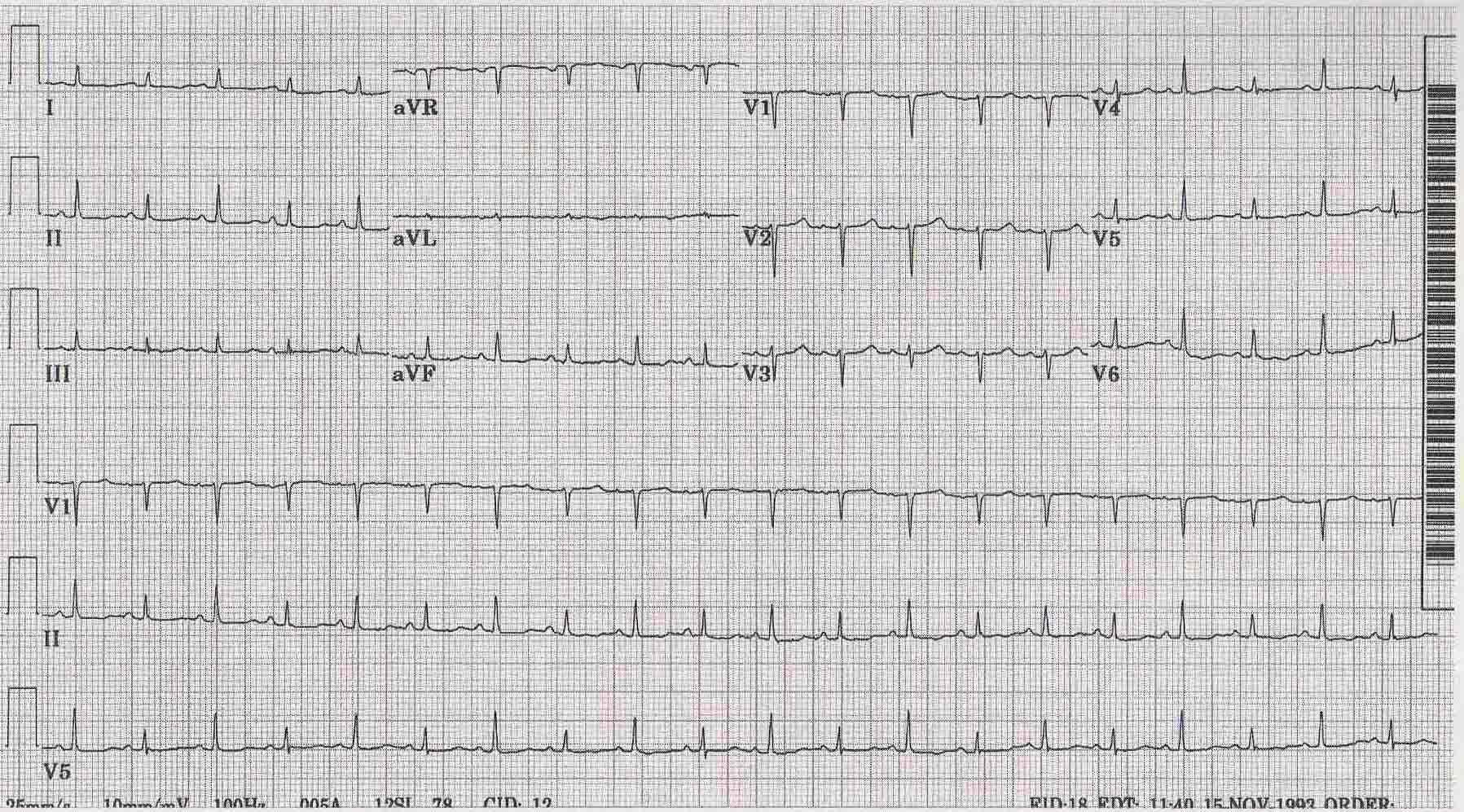
ST depression. ST depression refers to a finding on an electrocardiogram, wherein the trace in the ST segment is abnormally low below the baseline.
What are the causes of St depression?
ST depression refers to a finding on an electrocardiogram, wherein the trace in the ST segment is abnormally low below the baseline. It is often a sign of myocardial ischemia, of which coronary insufficiency is a major cause. Other ischemic heart diseases causing ST depression include: Subendocardial ischemia or even infarction.
What does ST depression mean on a stress test?
What does ST depression mean on a stress test? In a cardiac stress test, an ST depression of at least 1 mm after adenosine administration indicates a reversible ischaemia, while an exercise stress test requires an ST depression of at least 2 mm to significantly indicate reversible ischaemia.
What does ST depression indicate?
What is ST depression in stress test? A test that indicates a high probability of coronary artery disease is one in which there is substantial ST depression at low work rate associated with typical angina-like pain and a drop in blood pressure. Deeper and more widespread ST depression generally indicates more severe or extensive disease.
What does ST depression on an ECG mean?
What does ST depression on an ECG mean? S T depression in ECG at entry indicates severe coronary lesions and large benefits of an early invasive treatment strategy in unstable coronary artery disease; the FRISC II ECG substudy. The Fast Revascularisation during InStability in Coronary artery disease.

What does ST depression indicate?
ST depression occurs when the J point is displaced below baseline. Just like ST elevation, not all ST depression represents myocardial ischemia or an emergent condition. There are multiple conditions associated with ST depression. Some of these include hypokalemia, cardiac ischemia, and medications such as digitalis.
Is it normal to have ST depression?
ST segment depression less than 0.5 mm is accepted in all leads. ST segment depression 0.5 mm or more is considered pathological. Some expert consensus documents also note that any ST segment depression in V2–V3 should be considered abnormal (because healthy individuals rarely display depressions in those leads).
How serious is ST depression?
Men with asymptomatic ST-depression during exercise had a 2.1-fold risk of sudden cardiac death and a 2.5-fold risk of CHD death compared with men without silent ischaemia after adjusting for conventional risk factors (Table 3). Asymptomatic ST-depression was associated with a 3.2-fold risk of sudden cardiac death.
Which is worse ST depression or elevation?
Conclusion: In patients with a first acute anterior MI treated with primary PCI, ST elevation in inferior leads had significantly worse short-term and long-term outcomes compared to no ST change or ST segment depression.
What is the treatment for ST depression?
A person may treat the underlying condition that is causing their ST depression. A person with an ST depression may also wish to make some lifestyle changes to help improve their heart health. This can include eating a healthy diet, getting regular physical exercise, avoiding smoking, and maintaining a moderate weight.
Can anxiety cause ST depression on ECG?
Anxiety-related ECG changes The ECG changes in anxiety are: ST flattening, the commonest finding. Frank ST depression; not rare, especially in hyperventilation.
What is the most common cause of ST segment depression?
Causes. It is often a sign of myocardial ischemia, of which coronary insufficiency is a major cause. Other ischemic heart diseases causing ST depression include: Subendocardial ischemia or even infarction.
Can stress cause ST segment depression?
Interpretation of the treadmill ECG stress test In general, the occurrence of horizontal or down-sloping ST-segment depression at a lower workload (calculated in METs) or heart rate indicates a worse prognosis and higher likelihood of multi-vessel disease.
What does ST depression look like on ECG?
The ECG is characterized by deep and persistent, concave-upward ST-segment depression in multiple limb and chest leads. ECG changes are stable over time and accentuated during exercise.
Can ST depression be reversed?
The quick reversibility response of ST-segment depression after using short-acting nitrates had achieved in my 3-case series. ST-segment depression reversibility with nitrates means that the ST-segment depressions for all cases were transient coronary vasospasm. However, coronary angiography was normal in all 3-cases.
What does ST depression mean on a stress test?
Objective: The electrocardiogram (ECG) obtained during stress testing often shows a typical pattern of primary ST depression. A similar pattern can occur in unstable angina. Current textbooks consider ST depression as a direct result of partial occlusion of a coronary artery.
Can ST depression be reversed?
The quick reversibility response of ST-segment depression after using short-acting nitrates had achieved in my 3-case series. ST-segment depression reversibility with nitrates means that the ST-segment depressions for all cases were transient coronary vasospasm. However, coronary angiography was normal in all 3-cases.
What does ST depression mean on a stress test?
Objective: The electrocardiogram (ECG) obtained during stress testing often shows a typical pattern of primary ST depression. A similar pattern can occur in unstable angina. Current textbooks consider ST depression as a direct result of partial occlusion of a coronary artery.
What does ST abnormality mean on EKG?
Abstract. An ST-T abnormality on an electrocardiogram (ECG) is known to independently predict subsequent morbidity and mortality from cardiovascular diseases. But how ST-T abnormality develops in relation to chronologic changes in cardiovascular risk factors has not been fully discussed.
What does ST changes mean on ECG?
Nonspecific ST-T-wave changes are very common and may be seen in any lead of the electrocardiogram. The changes may be seen in all or most of the leads (diffuse changes), or they may be present contiguous leads, such as the inferior, lateral, or anterior leads.
What is ST depression?
ST depression refers to a finding on an electrocardiogram, wherein the trace in the ST segment is abnormally low below the baseline.
How to determine ST segment depression?
ST segment depression may be determined by measuring the vertical distance between the patient's trace and the isoelectric line at a location 2 -3 millimeters from the QRS complex.
What is the difference between a cardiac stress test and an exercise stress test?
In a cardiac stress test, an ST depression of at least 1 mm after adenosine administration indicates a reversible ischaemia, while an exercise stress test requires an ST depression of at least 2 mm to significantly indicate reversible ischaemia.
Is ST elevation transmural?
Subendocardial means non full thickness ischemia. In contrast, ST elevation is transmural (or full thickness) ischemia. Depressed but upsloping ST segment generally rules out ischemia as a cause. Also, it can be a normal variant or artifacts, such as: Other, non-ischemic, causes include:
Can ST segment depression cause angina?
ST segment depression and T-wave changes may be seen in patients with unstable angina. Depressed but upsloping ST segment generally rules out ischemia as a cause. Also, it can be a normal variant or artifacts, such as: Pseudo-ST-depression, which is a wandering baseline due to poor skin contact of the electrode.
What is the normal ST segment depression?
Normal (physiological) ST segment depressions occur during physical exercise. These ST segment depressions have an upsloping ST segment. The depression in the J 60 point is usually <1 mm and they resolve rapidly once the exercise is stopped. Some experts believe that these ST segment depressions represent a benign form of subendocardial ischemia. Refer to Exercise Stress Testing for details.
What causes ST segment depression in left sided leads?
Heart failure may cause ST segment depressions in left sided leads (V5, V6, I and aVL). These depressions are horizontal or downsloping.
What causes a ST segment to be downsloping?
ST segment depression due to acute myocardial ischemia. ST segment depressions caused by ischemia are characterized by a horizontal or downsloping ST segment. Indeed, North American and European guidelines assert that the ST segment must be either downsloping or horizontal; otherwise ischemia is unlikely to be the cause of the ST segment depression.
What is resting ST segment depression?
Resting ST-segment depression has been identified as a marker for adverse cardiac events in patients with and without known CAD. 45–49 Miranda et al 50 performed a retrospective study of 223 patients without clinical or ECG evidence of prior MI. Excluded were women, patients with resting ECGs showing LBBB or left ventricular hypertrophy (LVH) and those on digoxin or with valvular or congenital heart disease. Ten percent of patients had persistent resting ST-segment depression and nearly twice the prevalence of severe coronary disease (30%) than those without resting ST-segment depression (16%). The criterion of 2 mm of additional exercise-induced ST-segment depression or downsloping depression of 1 mm or more in recovery was a particularly useful marker for the diagnosis of any coronary disease (likelihood ratio 3.4, sensitivity 67% and specificity 80%).
What causes ST elevation on treadmill?
These include left ventricular aneurysm, variant angina, severe ischemic heart disease, and left ventricular wall motion abnormalities. Left ventricular aneurysm after MI is the most frequent cause of ST-segment elevation on the resting ECG and occurs over Q waves or in ECG leads adjacent to Q waves. Early repolarization is a normal variant pattern of ST elevation that occurs in normal individuals who rarely exhibit diagnostic Q waves.
What is ST elevation in right precordial leads?
Grand et al. [20] found that ST-segment elevation in the right precordial leads is a transient ECG manifestation of moderate to severe acute pulmonary embolism. This phenomenon indicates transmural ischemia in the right ventricle due to hypotension, hypoxemia, right ventricular strain, and catecholamine surge [14,15]. Although ST-segment elevation in the right precordial leads (<2 mm) is not a rare phenomenon, prominent ST-segment elevation (≥0.2 mV) and confined to leads V1–V3 are not seen so frequently. The majority of the patients presenting prominent ST-segment elevation in the right precordial presented with hypotension or cardiogenic shock [6,21–23]. Negative T-waves in the right precordial leads are a frequent ECG manifestation of acute pulmonary embolism and may represent an evolutionary “post-ischemic” stage following ST-segment elevation [14,15]. In case of a new episode of transmural right ventricular ischemia, usually in the context of hypotension or cardiogenic shock, the deep negative T-waves will reduce or disappear or even pseudonormalize and the ST-segment elevation may reappear. Mohsen [21] and Wilson [22] respectively reported similar ECG findings to ours. The “coved” ST-segment elevations in leads V1–V4 [21,22] were identical to type-1 Brugada ECG pattern during cardiogenic shock. At baseline during hemodynamic stability before the Brugada ECG pattern, both cases presented with deep negative T-waves in leads V1–V4.
Can ST segment depression occur during exercise?
ST-segment depression can occur during exercise or in recovery, and both are important to evaluate. It has been proposed that changes limited to the recovery period are more likely to represent false-positive responses 24 or are due to coronary artery spasm. 25 To facilitate imaging as soon as possible during recovery, studies including postexercise nuclear and echocardiographic imaging sometimes do not include an ECG evaluation after exercise. 26 Though a cool-down walk is known to obscure recovery ST shifts, 27 a cool-down walk has been implemented for safety concerns. 28
Is ST segment depression a sign of ischemia?
ST segment depression is a consistent finding in patients during ritodrine infusion, and should therefore not always be interpreted as an indication of myocardial ischemia.
Is ST segment elevation always considered from baseline?
However, ST-segment elevation is always considered from the baseline ST level. Whether the elevation occurs over or adjacent to Q waves or in non-Q wave areas is important.
Is ST depression a prognostic factor?
ST-segment depression on initial ECG is strongly associated with unfavorable outcomes in NSTE-ACS and is a major independent prognostic factor in most risk prediction models. Its presence at admission has been shown to significantly correlate with short-term ( Savonitto et al., 1999) and long-term (≥ 1 year) ( Kaul et al., 2001; Cannon et al., 1997) mortality. While ST depression as minimal as 0.5 mV has been demonstrated to reflect myocardial ischemia and unfavorable prognosis ( Cannon et al., 1997 ), greater magnitudes of depression predict higher short-term mortality. Both the depth of the ST depression within a single lead ( Kaul et al., 2001) and the cumulative sum of the depressions in all leads ( Savonitto et al., 2005) carry independent prognostic weight. In an analysis from GUSTO-IIb, the latter was demonstrated to have a graded association with 30-day mortality and to predict the presence of three-vessel or left main coronary disease on angiography ( Savonitto et al., 2005 ).
What causes depression in ST segment?
Digoxin causes generalized ST segment depressions with a curved ST segment (generalized implies that the depression can be seen in most ECG leads). Figure 15 B.
What causes ST segment depression in left lateral leads?
Heart failure may cause ST segment depression in the left lateral leads (V5, V6, aVL and I) and these depressions are generally horizontal or downsloping.
What is ischemia ST segment?
Ischemic ST depressions display a horizontal or downsloping ST segment (this is a requirement according to North American and European guidelines). The horizontal ST segment depression is most typical of ischemia ( Figure 15 C ). ST segment depressions with upsloping ST segments are rarely caused by myocardial ischemia. However there is one notable exception, when an upsloping ST segment is actually caused by ischemia and the condition is actually alarming. Upsloping ST segment depressions which are accompanied by prominent T-waves in the majority of the precordial leads may be caused by an acute occlusion of the left anterior descending coronary artery (LAD). This constellation – with upsloping ST depression and prominent T-waves in the precordial leads during chest discomfort – is referred to as de Winters sign ( Figure 15 C ).
Why is the J point suboptimal for measuring ST segment deviation?
It must also be noted that the J point is occasionally suboptimal for measuring ST segment deviation. This is explained by the fact that the J point is not always isoelectric; this occurs if there are electrical potential differences in the myocardium by the end of the QRS complex (it typically causes J point depression). The reason for such electrical potential difference is that not all ventricular myocardial cells will finish their action potential simultaneously. Myocardial cells which depolarized at the beginning of the QRS complex will not be in the exact same phase as cells which depolarized during the end of the QRS complex. Due to this it is sometimes recommended that ST segment deviation be measured in the J-60 point, or J-80 point, which is located 60 and 80 milliseconds, respectively, after the J point ( Comprehensive Electrocardiology, MacFarlane et al, Springer, 2010; Chou’s Electrocardiologi, Surawicz, Elsevier 2010 ). At the time of J-60 and J-80, there is minimal chance that there are any electrical potential differences in the myocardium. Current guidelines, however, still recommend the use of the J point for assessing acute ischemia ( Third Universal Definition of Myocardial Infarction, Thygesen et al, Circulation ). A notable exception to this rule is the exercise stress test, in which the J-60 or J-80 is always used (because exercise frequently causes J point depression).
Why is ST segment elevation important?
Displacement of the ST segment is of fundamental importance, particularly in acute myocardial ischemia. Because myocardial ischemia affects a limited area and disturbs the cells’ membrane potential (during phase 2), it engenders electrical potential difference in the myocardium.
What causes ST segment elevation?
Ischemia typically causes ST segment elevations with straight or convex ST segments ( Figure 16, panel A ). The straight ST segment can be either upsloping, horizontal or (rarely) downsloping. Non-ischemic ST segment elevations are typically concave ( Figure 16, panel B ). Concave ST segment elevations are extremely common in any population; e.g ST segment elevation in leads V2–V3 occur in 70% of all men under the age of 70. There is no definite way to rule out myocardial ischemia by judging the appearance of the ST segment, which is why North American and European guidelines assert that the appearance of the ST segment cannot be used to rule out ischemia. ECG changes in ischemia are discussed in detail in section 3 ( Acute & Chronic Myocardial Ischemia & Infarction ) and a specific chapter discusses ST elevation in detail.
What is secondary ST-T?
Secondary ST-T changes occur when abnormal depolarization causes abnormal repolarization. This is seen in bundle branch blocks (left and right bundle branch block), pre-excitation, ventricular hypertrophy, premature ventricular complexes, pacemaker stimulated beats etc. In each of these conditions the depolarization is abnormal and this affects the repolarization so that it cannot be carried out normally.
What is ST depression?
A finding on an electrocardiogram (EKG) may often be referred to as a ST depression. The measurement of the vertical distance between the trace and isoelectric lines at a location of 2-3 millimeters from the QRS complex may often be used in order to determine ST depression. If the measurement is more than 1 millimeter in V5-V6 or 1.5 millimeters in AVF or III the ST depression may be significant. If the ST depression of at least 1 millimeter after adenosine has been administered a reversible ischemia may present itself on a cardiac stress test. However, a ST depression of at least 2 millimeters may present itself to be reversible on an exercise stress test. In the case of non-transmural ischemia, the cause of ST depression may be an elevated resting potential in the myocardial cells. However, the ST segment may less likely be affected as it shows in a depolarized state. ST depression may often cause many commonly asked questions regarding the causes and treatments. Read below where Experts have answered many commonly asked questions regarding ST depression.
How much ST depression is needed for AVF?
If the measurement is more than 1 millimeter in V5-V6 or 1.5 millimeters in AVF or III the ST depression may be significant. If the ST depression of at least 1 millimeter after adenosine has been administered a reversible ischemia may present itself on a cardiac stress test.
What does ST elevation mean?
An ST elevation or ST depression may be an indicator of IHD (ischemic heart disease) is either situation of resting or while performing a stress test. In the case that ST elevation or ST depression is present, the stress test may need to be stopped and chest pain may become present with or without sweating. The chest pain may be present in the ...
How high is a false positive stress test?
However, false positive stress test may be as high as 40% in women and 10% in men. A myocardial perfusion imaging test may be the next test that a medical practitioner may decide to perform in order to confirm a diagnosis.
Can ischemia be a stress test?
A myocardial inducible ischemia may be implied on a stress test by a ST depression. This could also mean that there could be some narrowing of the coronary arteries. In the case of narrowed arteries then the arteries may not be able to supply enough oxygenated blood during exercise related stress.
Can ST depression be reversible?
However, a ST depression of at least 2 millimeters may present itself to be reversible on an exercise stress test. In the case of non-transmural ischemia, the cause of ST depression may be an elevated resting potential in the myocardial cells.