
What is central positional nystagmus (CPN)?
Two types of central positional nystagmus (CPN). When the head is moved from left ear-down to right ear-down position, right beating horizontal nystagmus changes into left beating nystagmus. The velocity of left beating nystagmus shows a peak initially (about 40°/s) and then decreases exponentially.
Is positional nystagmus associated with central lesions in brain tumors?
However, positional nystagmus is also encountered in central lesions. We aimed to determine clinical characteristics of the structures responsible for central positional nystagmus (CPN) associated with brain tumors.
What causes positional nystagmus in peripheral vestibular disease?
Abstract Purpose: Positional nystagmus is usually caused by peripheral vestibular disorder, mostly benign paroxysmal positional vertigo (BPPV). However, positional nystagmus is also encountered in central lesions.
Does long duration of nystagmus indicate central paroxysmal positional vertigo (CPN)?
It is, however, a well-known clinical notion that vertical PN, lack of latency, and long duration of nystagmus may indicate CPN, but to date this has not been evaluated in a systematic way.
What is central nystagmus?
Nystagmus of central origin characteristically is worsened by fixation of gaze, while peripheral nystagmus may be ameliorated. Central nystagmus may be unidirectional or multidirectional and may change direction with an alteration in the direction of gaze (ie, gaze evoked), while peripheral nystagmus is unidirectional.
What causes positional nystagmus?
A change in the orientation of the head with respect to the pull of gravity may induce paroxysmal (transient) or persistent positional nystagmus in central as well as peripheral vestibular disorders (Büttner et al., 1999; Bisdorff et al., 2009; Kim and Zee, 2014).
Is positional nystagmus normal?
Conclusion: Positional nystagmus is a common finding in normal subjects and occurred in 88% of the healthy subjects in the present study. Horizontal direction-changing apogeotropic or geotropic nystagmus may occur in asymptomatic subjects.
What is central positional vertigo?
Central vertigo is a clinical condition in which an individual experiences hallucinations of motion of their surroundings, or a sensation of spinning, while remaining still, as a result of dysfunction of the vestibular structures in the central nervous system (CNS).
What is a positional nystagmus test?
Positional testing determines whether a change of position of the patient's vestibular systems in space provokes nystagmus. Some nystagmus is only evident with changes in head position with respect to gravity.
What nerve causes nystagmus?
The vestibulocochlear nerve (cranial nerve eight) mediates your sense of sound and balance. It does not control eye movement, but a deficit in this nerve can impair balance to a degree that causes nystagmus.
Is positional nystagmus central or peripheral?
In most instances the cause is a peripheral vestibular disorder, as in benign paroxysmal positioning vertigo (BPPV). Central lesions can lead to positional nystagmus (central PN) or to paroxysmal positioning nystagmus and vertigo (central PPV).
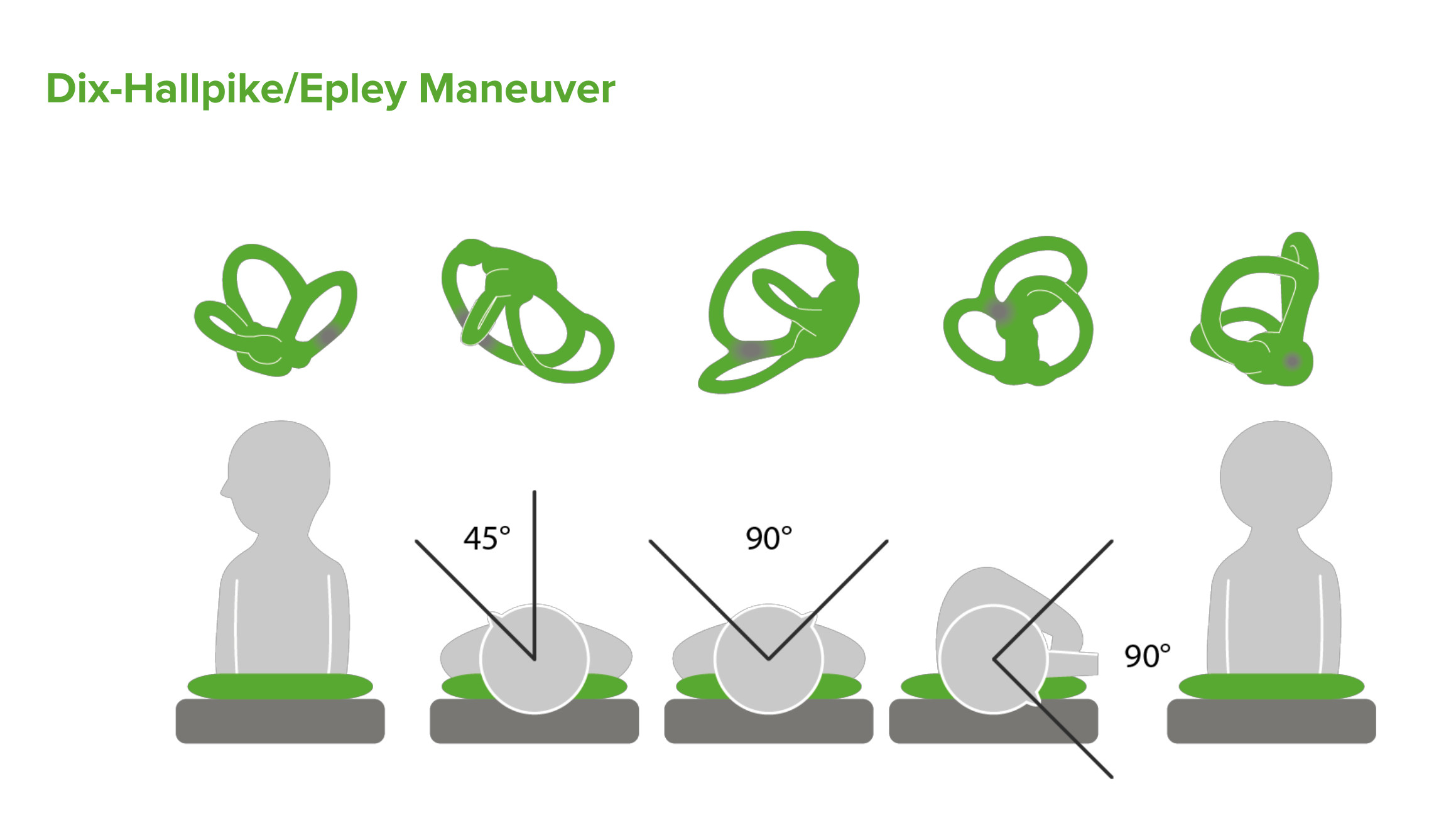
How do you test for BPPV vertigo?
Diagnosing BPPV involves taking a detailed history of a person's health. The doctor confirms the diagnosis by observing nystagmus — jerking of the person's eyes that accompanies the vertigo caused by changing head position. This is accomplished through a diagnostic test called the Dix-Hallpike maneuver.
What does direction changing nystagmus mean?
Direction-changing positional nystagmus (DCPN) is a nystagmus that changes its direction with different body and head positions. Many authors consider that it indicates the presence of a central nervous system lesion.
Is Central vertigo life threatening?
Central Vertigo is linked with serious conditions such as stroke, multiple sclerosis, and brain tumor. So yes, in this case, vertigo can be quite dangerous. And you should seek the emergency room immediately. (Read about the Warning Signs of Central Vertigo.)
What is the most common cause of central vertigo?
The most common central causes of dizziness and vertigo are cerebrovascular disorders related to the vertebrobasilar circulation, migraine, multiple sclerosis, tumors of the posterior fossa, neurodegenerative disorders, some drugs, and psychiatric disorders.
How common is central positional vertigo?
Central Positional Vertigo (CPV) CPV is a rare cause of positional vertigo. It is especially common due to structural lesions in the cerebellum, especially the cerebellar nodulus and uvula (Lee et al, 2014).
What inner ear problems cause nystagmus?
Inner ear disorders such as labyrinthitis or Meniere's disease can lead to acquired nystagmus. However, the most common cause is probably toxic — certain drugs or medication, including Dilantin (an antiseizure medication), alcohol intoxication, or any sedating medicines can harm the labyrinth.
What does a person with nystagmus see?
If you have nystagmus, your eyes move or “wobble” constantly. This can be in a side to side, an up and down, or a circular motion, or a combination of these. This uncontrolled movement can affect how clearly you can see. Most people with nystagmus have reduced vision.
What causes involuntary eye rolling?
Nystagmus is most commonly caused by a neurological problem that is present at birth or develops in early childhood. Acquired nystagmus, which occurs later in life, can be the symptom of another condition or disease, such as stroke, multiple sclerosis or trauma.
Does anxiety cause nystagmus?
Nystagmus. According to the American Optometric Association, nystagmus is generally triggered by stress and overall fatigue.
What is persistent nystagmus?
Persistent nystagmus in a specific head position from a central lesion implies an involvement of the central gravity processing ( Glasauer et al., 2001 ). Since the persistent and paroxysmal CPN often co-exist, the characteristics of persistent CPN can be assessed only after the paroxysmal component disappears. In most studies, the persistence of CPN has been defined by the duration of induced nystagmus of more than 1 min with a stable intensity ( Bisdorff et al., 2009 ).
What is the central vestibular system?
The central vestibular system operates to precisely estimate the rotational velocity and gravity orientation using the inherently ambiguous information from peripheral vestibular system. Therefore, any lesions disrupting this function can generate positional nystagmus. Central positional nystagmus (CPN) can be classified into the paroxysmal (transient) and persistent forms. The paroxysmal CPN has the features suggesting a semicircular canal origin regarding the latency, duration, and direction of nystagmus. Patients with paroxysmal CPN commonly show several different types of nystagmus classified according to the provoking positioning. The persistent form of CPN mostly appears as downbeat nystagmus while prone or supine, or apogeotropic or geotropic horizontal nystagmus when the head is turned to either side while supine. CPN may be ascribed to erroneous neural processing within the velocity-storage circuit that functions in estimating angular head velocity, gravity direction, and inertia. Paroxysmal CPN appears to be post-rotatory rebound nystagmus due to lesions involving the cerebellar nodulus and uvula. In contrast, persistent CPN may arise from erroneous gravity estimation. The overlap of lesion location responsible for both paroxysmal and persistent CPN may account for the frequent coexistence of both forms of nystagmus in a single patient.
What is the relationship between the direction of paroxysmal CPN and the canals stimulated during each positioning?
With these analyses, it was disclosed that the rotational vector of paroxysmal CPN is mostly aligned with the rotational axes of the semicircular canals inhibited during the positioning . For instance, during right Dix-Hallpike maneuver, right posterior (excitation) and left anterior semicircular (inhibition) canals are mainly stimulated, but the ipsilateral (excitation) and contralateral (inhibition) horizontal canals are also stimulated in part. Accordingly, the rotational axis of paroxysmal CPN triggered during right Dix-Hallpike maneuver is aligned with the vector sum of the rotational axes of left anterior and left horizontal canals that are normally inhibited during this positioning. Given that canalolithiasis of the anterior canal can also generate paroxysmal torsional downbeat nystagmus during Dix-Hallpike or straight-head hanging maneuvers ( Bertholon et al., 2002 ), differentiation of paroxysmal CPN from BPPV may be challenging when only based on the direction of nystagmus.
What is the direction of spontaneous nystagmus?
Peripheral or central spontaneous nystagmus (i.e., nystagmus already present while looking in the straight-ahead (center) gaze position with the head stationary in the upright and neutral position (not turned or tilted) is frequently modulated by head position, and such modulation should not be mistaken for CPN [ 1, 17 ]. Specifically, horizontal spontaneous nystagmus is predominantly modulated along the interaural plane in the supine position. Patients with acute peripheral vestibular neuritis show direction-fixed horizontal spontaneous nystagmus, which is more intense when they lie on their affected ear (i.e., the slow phase side), and occasionally direction-changing apogeotropic nystagmus (i.e., reverses direction when they lie on the fast phase side). In contrast, patients with acute stroke or a multiple sclerosis relapse, apart from the above-mentioned patterns, might also show direction-fixed spontaneous nystagmus which is stronger when turning the head to the fast phase side or direction-changing geotropic nystagmus (i.e., reverses direction when lying on the slow phase side). A mismatch between the intended/estimated and the real level of neuronal discharge in the vestibular nuclei has been proposed to explain positional findings in acute vestibular syndrome. Over time, nystagmus reverses its direction in one or more positions following acute vestibular syndrome, giving rise to any combination of direction-fixed or direction-changing nystagmus in supine positions in both groups. This was believed to reflect vestibular compensation, possibly indicating adaptive hyperactivity or hypoactivity of the vestibular nuclei [ 17 ]. Vertical spontaneous nystagmus on the other hand is predominantly modulated along the naso-occipital plane. For example, upbeat nystagmus in the upright position often improves or reverses to downbeat nystagmus in the prone position. While not contradicting the existence of a primary otolithic dysfunction in the genesis of upbeat nystagmus change to downbeat nystagmus with head position, there is recent evidence for additional positional modulation vertical SCC using head impulse test analysis in different head positions [ 55 ]. Lastly, both positional modulation of spontaneous and CPN may co-exist in the same individual and its frequency is probably underestimated [ 17, 56 ].
What is central positional vertigo?
Clinically, central positional nystagmus (CPN) is often suspected when atypical forms of its peripheral counterpart , i.e., benign paroxysmal positional vertigo (BPPV), are observed , namely a linear horizontal nystagmus as in horizontal canal BPPV or a downwardly and torsionally beating nystagmus as in anterior canal BPPV. Pathophysiologically, CPN is caused by cerebellar and/or brainstem dysfunction. Recent work has provided further insights into the different clinical phenotypes and the underlying pathomechanisms. We performed a PubMed review focused on the findings on CPN using the key words “Central Positional Nystagmus”, “Central Positional Vertigo”, “Positional Nystagmus” OR “Positioning Nystagmus” OR “Positional Vertigo” OR “Positioning Vertigo” AND “Central” from January 2015 to August 2021. CPN may account for up to 12% of patients with positional nystagmus. Clinical data on CPN are mostly based on case reports or small retrospective case series. CPN is frequently associated with cerebellar and/or brainstem structural lesions, namely stroke, tumours or demyelination, or diffuse involvement of these structures due to degenerative or autoimmune/paraneoplastic diseases; it is also found in patients with vestibular migraine. CPN can be paroxysmal or persistent. The direction of the nystagmus is often downward in head-hanging or apogeotropic in lateral supine positions; combinations of both forms also occur. Clinically it is important to note that CPN is often associated with other central, often cerebellar ocular motor or other neurological signs; typically, it is not improved by the therapeutic liberatory manoeuvres for BPPV. These additional features are also important for the diagnosis, in particular if no structural lesions are found. Pathophysiologically, CPN is believed to reflect an abnormal integration of semicircular canal-related signals by the cerebellar nodulus, uvula and/or tonsil, ultimately providing an erroneous estimation of the head tilt and/or eye position coordinates. The natural course of CPN remains, so far, largely unknown. Symptomatic treatment of CPN consists of pharmacotherapy, e.g., with 4-aminopyridine, and causative treatment of the underlying disease if known. CPN is an important differential diagnosis to BPPV and a clinically relevant entity with heterogenous clinical presentations and various pathomechanisms and etiologies. In particular, studies on the natural course and treatment of CPN are needed.
What is the pathophysiology of CPN?
Among those patients with etiologies without evident structural lesions, CPN pathophysiology remains largely unknown. Between VM attacks, hypersensitized nodulus and uvula may suppress the vestibular nuclei as an adaptive/compensatory response to aberrant vestibular nuclei activation. During attacks, brainstem regions associated with migraine (e.g., locus coeruleus; dorsal raphe nucleus) are believed to excite the vestibular nuclei to the extent that nodulus and uvula suppression is no longer adequate to maintain stability, particularly when nodulus and uvula activity is being modulated (i.e., when changing head position), resulting in positional nystagmus and vertigo [ 48 ]. An alternative mechanism for VM-related CPN relates to the existence of cortical spreading depression in the occipital lobes (i.e., a depolarizing propagating wave that causes neural hyper excitability followed by long lasting neural suppression, leading to changes in perfusion and metabolism of the cortical brain tissue), as a potential generator of vertigo in migraine. Supporting this theory, a recent study showed an association between elevated lactate peaks in the occipital lobes on MR spectroscopy and the presence of CPN in VM patients [ 36 ].
What are the CPN assessment maneuvers?
CPN assessment should include the following positional maneuvers: head-hanging from sitting position on each side (Dix-Hallpike maneuver) and return to the upright position, straight head-hanging from sitting and return to the upright position, and lying down from sitting and assuming the ear-down position on each side while supine (Pagnini-McClure maneuver) (Fig. 1) [ 5, 8, 21 ]. Each maneuver should be performed as rapidly as possible, since slow movements might not be sufficient to provoke CPN [ 22 ]. Ideally, patients should also be examined by video-oculography in the dark with ocular fixation removed, as sensitivity for CPN detection increases and additional analysis of nystagmus waveform might be useful [ 5 ]. A full ocular motor exam, including the assessment of spontaneous nystagmus, pursuit, saccades, gaze-evoked nystagmus (GEN), post-head shaking nystagmus (HSN), ocular tilt reaction (OTR), subjective visual vertical (SVV), head impulse test, and hearing as well as a full neurological exam are mandatory to discard the presence of associated signs in CPN patients [ 5, 6, 8] (for differential diagnosis see below).
How to determine head rotation?
CPN model. Head rotations are sensed by the SCC in the inner ear. Here, the relative endolymph motion is detected by the cupula, which when deflected, creates a neural signal indicating the head rotation. The angular velocity estimate of the head is then centrally reconstructed by a velocity storage integrator in the brainstem, which considers the inherent deficiencies in the dynamics of the SCC. A negative feedback loop is added to the integrator to prevent noise accumulation in the integrator’s output. Head translation in space and tilt relative to gravity are sensed by the otolith organs in the inner ear. Here, a neural signal based on gravito-inertial acceleration is obtained, which does not distinguish between tilt and translation. Additional sensory clues about head orientation relative to gravity, provided by the SCC, help to solve the gravito-inertial ambiguity, by conveying a signal to a gravity direction (i.e., head tilt) estimator in the cerebellum, which integrates head rotation velocity over time. The gravity direction estimator delivers an estimate of the gravity vector, which can then be subtracted from the gravito-inertial acceleration to calculate inertia and estimate head linear acceleration (i.e., head translation). A somatogravic feedback loop is added to the gravity direction estimator to prevent error accumulation due to the integration of a noisy signal and bring the gravity estimate towards the gravito-inertial acceleration. Finally, a rotational feedback loop conveying a virtual angular velocity signal (i.e., the cross-vector product of the estimated gravity direction and the gravito-inertial acceleration) is additionally added to the velocity storage integrator to prevent inaccuracies in angular velocity estimation, which in turn would promote an incorrect estimation of gravity direction. The nodulus and uvula seem to be responsible for the estimation of gravity direction and feeding this signal into the rotational feedback loop. In persistent apogeotropic CPN, a lesion (cross) involving the vestibulo-cerebellar pathway that relays the estimated gravity to rotational feedback creates a bias of the estimated gravity direction toward the nose along the naso-occipital axis of the head while in ear-down positions. The persistent mismatch between the actual and estimated gravities forces the rotational feedback loop to bring the estimate of gravity direction toward the actual one, thus generating apogeotropic nystagmus. In persistent geotropic CPN, the mechanism is similar and only the direction of bias reverses (i.e., away from the nose). In paroxysmal (downwardly beating and apogeotropic) CPN, dysfunction of the nodulus and uvula generates a prominent post-rotatory response by the SCC, which causes an erroneous estimation of angular and gravity direction estimation (circles line). SCC semicircular canal, CPN central positional nystagmus
Why is CPN not aligned with head motion?
One additional mechanism which might be important in CPN, particularly in cases in which CPN direction is not aligned with that of the head motion during the positioning, is the presence of a mismatch between eye position estimated by the burst generator and the neural integrator, hypothetically due to altered otolith input to one of these systems [ 11 ].
Is nystagmus a multiplanar or uniplanar plane?
In terms of the direction of the nystagmus, CPN can be further classified into multiplanar (i.e., occurrence of various types of nystagmus along different planes; e.g., vertical and horizontal CPN in the same individual) and uniplanar [ 5, 8 ]. Lastly, the nystagmus plane in CPN may be aligned or not with the vector sum of the rotational axes of the semicircular canals (SCC) that are normally involved during the positioning (e.g., downwardly beating nystagmus during straight head-hanging vs. upwardly beating nystagmus during ear-down position) [ 5, 24 ]. In this review, the direction of jerk nystagmus is always described in a head-referenced frame (e.g., nystagmus beating toward the forehead is upwardly beating, regardless of head position), except for horizontal jerk nystagmus in Pagnini-McClure positions, which is described in an earth-referenced frame (i.e., nystagmus that beats toward the earth in ear-down positions is called geotropic while that which beats away from the earth is called apogeotropic).
What are the characteristics of nystagmus?
The characteristics of nystagmus upon positional testing were extracted from each patient. This description was divided into the classical features of PN, i.e., the direction of nystagmus, provoking position, duration of nystagmus, latency of onset, fatigability, and the presence of concurrent symptoms such as subjective vertigo, nausea, and/or vomiting.
Which ear is the nystagmus in?
For HC-BPPV, the nystagmus that occurs when the left ear or right ear is in the down position can be directed to the undermost (geotropic) or uppermost (apogeotropic) ear ( 1 ). Thus, this feature (geotropic or apogeotropic) cannot be used to differentiate a peripheral or central origin.
How many patients have spontaneous nystagmus?
It is noteworthy that only 2 (2.4%) patients within the data set reported the presence of spontaneous nystagmus ( 12, 25 ). This minimized the potential influence of the well-known phenomenon that a discrete spontaneous downbeat nystagmus, which may not be visible under Frenzel glasses, becomes only evident by positioning the patient.
Where is the loss of visual suppression of nystagmus with optic fixation?
The loss of visual suppression of nystagmus with optic fixation indicates a lesion at the flocculonodular lobe of the cerebellum ( 38, 39 ). The effect of visual fixation upon nystagmus was only documented in two patients of the papers reviewed here, with patients with posterior fossa lesions demonstrating a failure of fixation suppression ( 16 ).
What are the Associated neurological signs or symptoms?
This information referred to any central symptom such as gait disturbances, abnormal oculomotor function, and atypical symptoms such as unexplained weight loss, as well as reference to normal or abnormal observations upon clinical examination and testing.
Is nystagmus downbeating or upbeating?
The purely vertical nystagmus upon D–H was pure downbeating in 17 (42.5%) ( 7, 14, 16, 27, 30 ), pure upbeating in 1 (2.5%) ( 19 ), and upbeating followed by downbeating in 1 (2.5%) ( 7 ). Due to a lack of consensus in terminology, it was impossible to interpret the direction of torsional nystagmus unless specified, but nystagmus beating away from the lowermost ear (apogeotropic) was reported by Choi et al. ( 4) in all nine of the patients who were presented with torsional nystagmus upon D–H testing ( 4 ).
Is central positional vertigo a controlled study?
The study selection process of this review did not identify any controlled studies relevant to the diagnosis of central positional vertigo/nystagmus. For this reason, this review included case studies and case series for consideration of their evidence. The authors recognize that such study designs, which are retrospective in nature, are inherently susceptible to the risk of bias. The case series did not typically recruit consecutive series of individuals from multiple centers, and this introduced a risk of selection bias. The studies were also at risk of detection of reporting/observer bias in which the clinical presentation of the CPN reported was not standardized. Furthermore, none of these case studies or case series that were considered relevant to the current review referred to results in a comparison group.
What is central positional nystagmus?
Two types of central positional nystagmus have been identified: central positional nystagmus without vertigo (CPN) and central positional nystagmus with vertigo (CPV). 1, 2 Central positional nystagmus without vertigo is characterized by nystagmus that persists as long as the head is held in the provoking position. 1 The nystagmus is typically in one direction (vertical, horizontal, or torsional), unlike the mixed vertical torsional nystagmus seen in posterior and anterior semicircular canal BPPV. Central positional nystagmus may be seen in elderly patients when they are in supine. The elicited nystagmus is typically vertical. In the absence of other findings on the examination, the CPN is thought to be benign. In other individuals, the CPN may be seen in conjunction with either upbeating or downbeating spontaneous nystagmus while the patient is seated. The CPN in these cases is typically greater than the spontaneous nystagmus observed in sitting.
What are the causes of nystagmus and CPN?
The upbeating spontaneous nystagmus and CPN have been associated with central disorders such as tumor, stroke, and multiple sclerosis affecting brachium conjunctivum or the ventral tegmental tract. 4 Many of these patients also had findings of abnormal smooth pursuit.
What causes upbeating nystagmus?
The upbeating nystagmus is caused by a higher level of neural activity in the central posterior semicircular canal pathways relative to the central anterior semicircular canal pathways. + +. Given the lack of symptoms of vertigo with the positional tests, the unidirectionality of the positional nystagmus, and the other oculomotor findings, ...
What is positional vertigo?
Although benign paroxysmal positioning vertigo (BPPV) is a common finding that is relatively easy to diagnose and treat, there are causes of positional nystagmus and positional vertigo that are a result of either abnormalities within the central nervous system or other peripheral vestibular conditions. These conditions will not respond to the conservative measures described for the treatment of BPPV. The goal of this appendix is to help the clinician identify the signs and symptoms of positional nystagmus and positional vertigo that are not consistent with BPPV and are suggestive of other disorders.
What is nystagmus in the eye?
Nystagmus: Symptoms, Causes, Diagnosis, Treatment. Nystagmus is a condition where you can’t control your eye movement. It may affect your vision. WebMD explains what it is and which treatments might help ease symptoms. Skip to main content .
What Causes Nystagmus?
It may be a sign of another eye problem or medical condition. You may be born with it, or you might develop it later in life. Nystagmus is caused by many different things, including:
What does it mean when your eyes move?
You may feel like your eyes have a mind of their own. They move up and down, side to side, or in a circle. This is called nystagmus or "dancing eyes ." It's a condition where you can't control your eye movements.
How to fix nystagmus?
Wear the right contacts or glasses to improve vision. It won't cure nystagmus, but it can help with other eye problems that can make it worse. Eye muscle surgery may be an option. The goal is to help with the head tilt that often comes with nystagmus. Sometimes surgery improves vision, too.
What is the best treatment for nystagmus?
Eye muscle surgery may be an option. The goal is to help with the head tilt that often comes with nystagmus. Sometimes surgery improves vision, too.
How to tell if a child has nystagmus?
If you think you or your child may have symptoms of nystagmus, see your eye doctor. They’ll look at the insides of your eyes and test your vision. They’ll also look for other eye problems.
Why do my eyes move?
The movement might be in one eye, but it's usually in both eyes. You may notice that you nod your head or keep it in strange positions. You do that because it helps you focus when you can't hold your gaze steady.
What is central vertigo?
Central vertigo is a clinical condition in which an individual experiences the sensation of motion despite remaining still. It results from a dysfunction in the central vestibular aspects of the nervous system. This activity explains when central vertigo should be considered on differential diagnosis and reviews the proper evaluation and management of this condition.
What is the meaning of "central vertigo"?
Central vertigo is a clinical condition in which an individual experiences hallucinations of motion of their surroundings, or a sensation of spinning, while remaining still , as a result of dysfunction of the vestibular structures in the central nervous system (CNS) .[1] The patient complains typically of dizziness with hallucination or sense of spinning. This is different from the light-headed "dizziness" which is more commonly secondary to global impairment of cerebral perfusion.
What is the result of a lesion in the vestibular nucleus?
Any lesion affecting the vestibular nuclei or their projections especially those to and from the cerebellum will result in symptoms of vertigo and associated signs of nystagmus.
What is the most important clinical scenario?
The most important clinical scenario is one a patient presented to the emergency department or urgent care with acute vertigo. Most patients suffering from vertigo have a peripheral cause including benign paroxysmal positional vertigo, acute vestibular neuritis (or labyrinthitis), Meniere disease or even perilymphatic fistula or superior semicircular canal dehiscence. However, identification of central vertigo clinically is of utmost importance due to the serious underlying cause of brainstem ischemia or infarction.
What test is used to diagnose vertigo?
As described above in the history and physical, tests for causes of peripheral vertigo such as Dix-Hallpike test and simple screening test for hearing are important. A detailed neurological exam including assessment of extremity and truncal ataxia, gait, and HINTS test should all be performed.
When is a neurologic consultation necessary?
Finally, a neurologic consultation is warranted for a patient complaining of vertigo, and a neurosurgical consultation is necessary if an underlying hemorrhage, edema, or brainstem compression is discovered, as surgical decompression (e.g., ventriculostomy or craniectomy) may be required .
Is central vertigo more common than peripheral vertigo?
1. Central vertigo is much less common compared with peripheral vertigo yet its recognition is extremely important to improve the outcome of the patient.
