Possible complications of chronic apical periodontitis
- Growth formation in the periapical region (periapical granuloma)
- Cyst formation in the apex of the affected tooth (radicular cyst)
- Pus formation and abnormal opening from the mouth to the outer face (sinus)
- Acute worsening of the disease
What conditions does a periodontist treat?
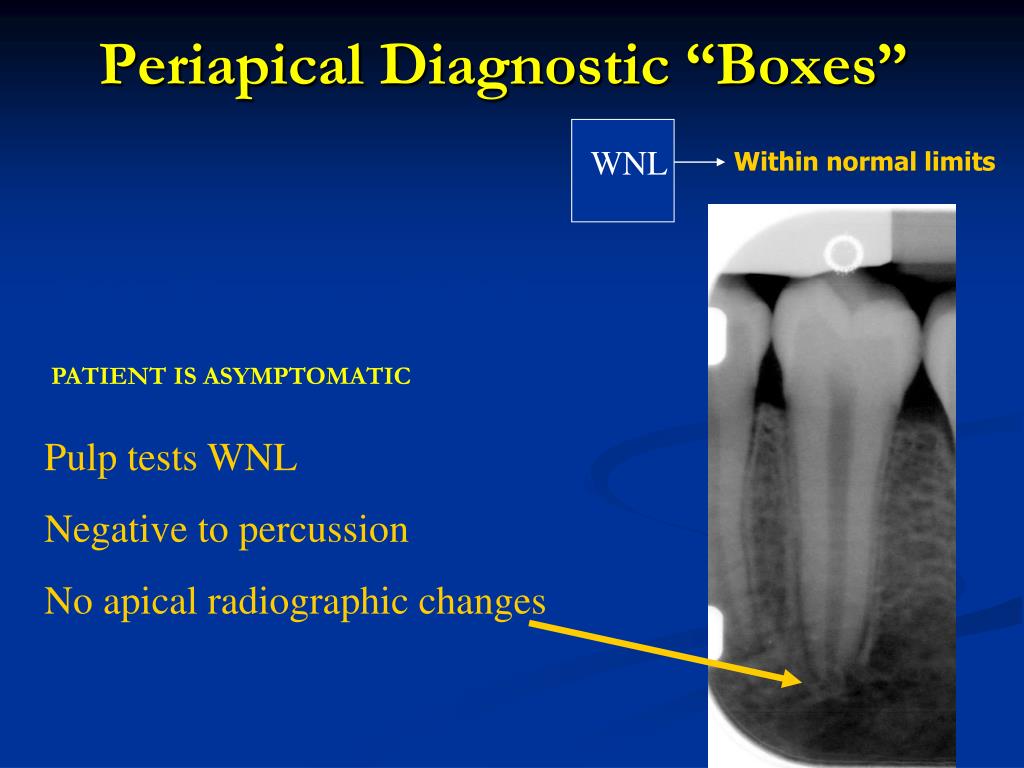
Two types of apical periodontitis exist: Asymptomatic. Asymptomatic apical periodontitis does not produce any clinical signs or symptoms. However, long-term inflammation can eventually destroy the tissue surrounding the teeth. This type usually develops gradually and is ongoing, which is why it once was referred to as chronic periapical periodontitis. Symptomatic.
How do I manage a patient with periodontal abscess?
Chronic periodontitis is a common disease of the oral cavity consisting of chronic inflammation of the periodontal tissues that is caused by the accumulation of profuse amounts of dental …
What is symptomatic apical periodontitis?
Mar 02, 2018 · Chronic apical periodontitis is generally a non-painful condition in which the apical portion (i.e. the part around the tip) of a tooth’s root is chronically inflamed. The term chronic …

What is chronic periapical?
Chronic apical periodontitis is most likely the final stage of periodontitis that a person will experience. It is generally a non-painful condition that is in the apical portion of the apical canal around the tip of the tooth root causing chronic inflammation.
How is periapical periodontitis treated?
What bacteria is involved in periapical periodontitis?
Is apical periodontitis an infection?
Post-treatment apical periodontitis is certainly a microbiological problem, because infection is present in virtually all cases associated with this condition, even in teeth with apparently adequate root canal treatments.Mar 21, 2014
What causes periapical periodontitis?
What is the main cause of periodontal disease?
What is the most commonly encountered microorganism in pulp and periapical infections?
Can pulpitis spread?
How does a root canal get infected?
What does periapical mean in dentistry?
What is periapical image?
A periapical image shows the area completely "around the apex." This is important in that if the pulp tissue inside the tooth is not healthy, it will produce a dark shadow at the apex of the root which can only be seen with this type of radiograph. At right is a periapical film.
What is periapical tissue?
: of, relating to, occurring in, affecting, or being the tissues surrounding the apex of the root of a tooth periapical infection a periapical abscess.
What causes periodontitis to be hard?
Subsequently, question is, what causes periodontitis? It's typically causedby poor brushing and flossing habits that allow plaque—a sticky film of bacteria— to build up on the teeth and harden. In advanced stages, periodontaldisease can lead tosore, bleeding gums; painful chewing problems; and even tooth loss.
What is a periapical radiograph?
Periapical dental radiograph showing chronic periapical periodontitis on the root of the left maxillary second premolar. Periapical periodontitis or apical periodontitis (AP) is an acute or chronic inflammatory lesion around the apex of a tooth root, most commonly caused by bacterial invasion of the pulp of the tooth.
What is the best treatment for periapex infection?
Tooth extraction or apicalresection with curettage of the periapex usually is an adequate treatment. Endodontic treatmentwith a root canal may be used with tooth restoration. Antibiotic therapy is often used for infections.
What is the abscess at the root of a tooth?
A periapical abscess is a collection of pus at the root of a tooth, usually caused by an infection that has spread from a tooth to the surrounding tissues. Pus is the accumulation of these white blood cells, dead tissue, and bacteria.
Why do my gums bleed?
Gum Disease When people don't practice proper dental hygiene, bacteria in the mouth forms plaque on the teeth. These bacteria may cause your gums to become inflamed, which results in red, swollen, or bleeding gums. For many people with gingivitis, this inflammation is not painful.
What is a chronic abscess?
Chronic Apical Abscessis an inffammatory reaction to pulpal infection and necrosis characterized by gradual onset, little or no discomfort and an intermittent discharge of pus through an associated sinus tract. Radiographically, there are typically signs of osseous destruction such as a radiolucency.
What is the term for the accumulation of plaque in the oral cavity?
Chronic periodontitisis a common disease of the oral cavity consisting of chronicinflammation of the periodontaltissues that is caused by the accumulation of profuse amounts of dental plaque. Chronic periodontitisis prevalent in adults and seniors worldwide.
How common is periapical periodontitis?
Periapical periodontitis of some form is a very common condition. The prevalence of periapical periodontitis is generally reported to vary according to age group , e.g. 33% in those aged 20–30, 40% in 30- to 40-year-olds, 48% in 40- to 50-year-olds, 57% in 50- to 60-year-olds and 62% in those over the age of 60. Most epidemiologic data has been generated in European countries, especially Scandinavia. While millions of root canal treatments are carried out in the United States alone each year, total numbers of such cases do not provide reliable indicators of frequency, even for symptomatic periapical periodontitis (given that root canal treatment is not always indicated or complied with, and may also be performed in the absence of periapacial periodontitis).
What is AP in dentistry?
Periapical periodontitis or apical periodontitis ( AP) is an acute or chronic inflammatory lesion around the apex of a tooth root, most commonly caused by bacterial invasion of the pulp of the tooth.
What is the root tip of a tooth called?
Etymologically, the name refers to inflammation ( Latin, -itis) around ( peri- ) the root tip or apex ( -apical) of the tooth ( -odont- ). Periradicular periodontitis is an alternative term.
Do periapical inflammatory lesions show radiographic changes?
The radiographic features of periapical inflammatory lesions vary depending on the time course of the lesion. Because very early lesions may not show any radiographic changes, diagnosis of these lesions relies solely on the clinical symptoms.
What does periradicular mean in dental?
The term periradicular accurately reflects that the problem may have arisen along the root.
What is periradicular root?
The term periradicular accurately reflects that the problem may have arisen along the root. In fact, the problem frequently originates along the root somewhere (periradicular). Thus, the diagnosis is also beginning to be reported using these other descriptive terms.
What is the term for a tooth that is inflamed?
Chronic Apical Periodontitis. Chronic apical periodontitis is generally a non-painful condition in which the apical portion (i.e. the part around the tip) of a tooth’s root is chronically inflamed. The term chronic means the condition has been present for a significant length of time (at least several weeks, and sometimes much longer).
How accurate is periapical radiography?
The accuracy of bitewing and periapical radiography is low for estimating small alveolar bone changes (less than 1 mm) over time (Evidence Grade 3). Thus, performing radiographic examinations at regular intervals for the purpose of assessing changes of the periodontal support over time is not justified.
What does it mean when you bleed after probing your periodontal pocket?
Bleeding following probing of the periodontal pocket is a sign of inflammation in the periodontal tissues (Evidence Grade 2).
What is the best solution for gingivitis?
Mouth-rinsing with a chlorhexidine solution (0.12–0.2 percent) or essential oils as an adjunct to tooth brushing is more effective than tooth brushing alone for reducing gingivitis (Evidence Grade 3).
Does pressure sensitive probe improve periodontal pocket measurements?
The use of electronic pressure-sensitive probes does not improve the reproducibility of periodontal pocket measurements compared to that of manual probing (Evidence Grade 3). Radiographic measurements underestimate alveolar bone loss.
Is bleeding on probing a good predictor of periodontal stability?
The absence of “bleeding on probing” is a good predictor of periodontal stability (Evidence Grade 3).
Is scientific evidence for assessing and designing programs of supportive periodontal therapy insufficient?
Scientific evidence for assessing and designing programs of supportive periodontal therapy is insufficient. Economic Aspects. Scientific evidence is lacking for determining cost-effectiveness and patient-perceived quality with regard to the various methods of prevention, diagnosis and treatment of chronic periodontitis.
Is periodontitis a risk for other diseases?
Chronic Periodontitis as a Risk for Other Diseases. Scientific evidence is contradictory as to whether individuals with chronic periodontitis are at increased risk of developing coronary heart disease or stroke.
What are the different types of periodontitis?
There are three different types of periodontitis, including: 1 Chronic periodontitis, which is the most common and is caused by plaque buildup. 2 Aggressive periodontitis, which is hereditary and causes rapid loss of bone and teeth if untreated. 3 Necrotizing periodontal disease, which is the death of the gums, tooth ligaments, and bones due to lack of blood. It is typically linked to a suppressed immune system from cancer, HIV infections, or malnutrition.
What is the best treatment for periodontitis?
Treating periodontitis requires the support and guidance of your dentist. You’ll likely be prescribed an antiseptic mouthwash or spray you will use at home to combat the bacteria that has accumulated in the pockets of your gums. A deep cleaning, sometimes called scaling, is also a part of periodontitis treatment.
What causes tooth loss?
Chronic periodontitis, which is the most common and is caused by plaque buildup. Aggressive periodontitis, which is hereditary and causes rapid loss of bone and teeth if untreated. Necrotizing periodontal disease, which is the death of the gums, tooth ligaments, and bones due to lack of blood. It is typically linked to a suppressed immune system ...
How to prevent periodontitis?
In most cases, you can eliminate the risk factor through diligent oral hygiene that includes brushing twice a day, flossing, and receiving routine dental checkups is enough to prevent periodontitis.
Can plaque buildup cause periodontitis?
It’s possible to reverse gingivitis with routine dental care. However, if it’s left untreated, it eventually leads to periodontitis. When this happens, pockets form between ...
Can periodontal surgeons save teeth?
Once teeth begin to move within your gums with light finger pressure, have become overly erupted, or have lost gum tissue allowing more than one-third of the tooth root to show, even the best periodontal specialist cannot save your teeth and return them to a state of health.
Does periodontitis cause low birth weight?
Research has also shown that pregnant women with periodontitis tend to give birth prematurely more often and their babies are born with low birth weights.
What is the progression of periodontitis?
Disease progression is intermittent with periods of activity and remission influenced by bacterial profile and risk factors. Individuals in this group will usually have poor levels of plaque control and multiple deposits of calculus, both supra- and subgingival. The role of general and local modifying factors should be considered and both smoking and diabetes (uncontrolled) are positive risk factors for periodontitis. Within this group, bone loss can be characterized as either irregular (vertical) or horizontal. The involved teeth normally give positive responses to pulp testing, indicating vital but not undiseased pulp status. Teeth with extensive attachment loss of periodontal origin have poor prognosis and should be extracted ( Fig. 12.79 ). If such teeth give a negative response to pulp testing, it will not be clear without good insight into the clinical and radiographic history whether pulp necrosis is primary or secondary to periodontal disease. In cases of uncertainty, performance of first stage root-canal treatment followed by review of response will indicate endodontic origin if there is a good response ( Fig. 12.80 ).
How to tell if a tooth is periapical or periapical?
The symptoms of periapical inflammatory lesions can range across a broad spectrum, from being asymptomatic to an occasional toothache to severe pain with or without facial swelling, fever, and lymphadenopathy. A periapical abscess usually manifests with severe pain, mobility, and sometimes elevation of the involved tooth, swelling, and tenderness to percussion. Palpation of the apical region elicits pain. Spontaneous drainage into the oral cavity through a fistula (parulis) may relieve the acute pain. In rare cases, a dental abscess may manifest with systemic symptoms (e.g., fever, facial swelling, lymphadenopathy) along with pain. The acute lesion may evolve into a chronic one (periapical granuloma or cyst), which may be asymptomatic except for intermittent flare-ups of “toothache” pain, which mark the acute exacerbation of the chronic lesion. Patients often give a history of intermittent pain. The associated tooth may be asymptomatic, or it may be mobile or sensitive to percussion. More often, however, the periapical lesion arises in the chronic form de novo; in this case, it may be asymptomatic. The clinical presentation does not necessarily correlate with the histologic or imaging findings.
What is periapical inflammatory lesion?
A periapical inflammatory lesion is defined as a local response of the bone around the apex of a tooth that occurs as a result of necrosis of the pulp or through destruction of the periapical tissues by extensi ve periodontal disease ( Fig. 20-1 ). The pulpal necrosis may occur as a result of pulpal invasion of bacteria through caries or trauma. In Figure 20-1, the periapical inflammatory lesion is characterized by apical periodontitis, an inflammatory process that may histologically represent either a periapical abscess or a periapical granuloma. Toxic metabolites from the necrotic pulp exit the root apex to incite an inflammatory reaction in the periapical periodontal ligament and surrounding bone (apical periodontitis). This reaction is characterized histologically by an inflammatory infiltrate composed predominantly of lymphocytes mixed with polymorphonuclear neutrophils. Depending on the severity of the response, the neutrophils may collect to form pus, resulting in an apical abscess. This result is categorized as acute inflammation. Alternatively, in an attempt to heal from apical periodontitis, the body stimulates the formation of granulation tissue mixed with a chronic inflammatory infiltrate composed predominantly of lymphocytes, plasma cells, and histiocytes, giving rise to periapical granuloma. Entrapped epithelium (the rests of Malassez) may proliferate to form a radicular or apical cyst. Acute exacerbations of the chronic lesions may occur intermittently.
How does periapical abscess affect osteomyelitis?
If the surrounding bone marrow becomes involved with the inflammatory reaction through the spread of pyogenic organisms (bacteria that stimulate an inflammatory response), the localized periapical abscess may transform into osteomyelitis. The exact point at which a periapical inflammatory lesion becomes osteomyelitis is not easily determined or defined. The size of the area of inflammation is not as important as the severity of the reaction. However, considering the size of the lesion, periapical inflammatory lesions usually involve only the local bone adjacent to the apex of the tooth, whereas osteomyelitis involves a larger volume of bone. Periapical lesions occasionally may be large, but the epicenter of the lesion remains in the vicinity of the tooth apex. If the periapical lesion extends farther, so that the lesion no longer is centered on the tooth apex, osteomyelitis may be considered as a possible diagnosis. The distinction between periapical inflammation and osteomyelitis can be made if sequestra are detected in x-ray images. Progression from periapical inflammation to osteomyelitis is relatively rare, and other factors play a role in its development, such as a decrease in the host defenses and an increase in the virulence of pathogenic microorganisms.
How does age affect periodontitis?
Increasing age is correlated with an increased prevalence of periodontal disease, as well as an increase in both the extent and severity of the disease. Approximately 35.7% of adults aged 30 to 39 years experienced greater than 3 mm of attachment loss compared with 89.2% for those individuals aged 80 to 90 years.23 In a study that evaluated the prevalence, severity, and extent of periodontal disease in an employed United States population, loss of attachment greater than 1 mm was found in 99% of the subjects. 22 Approximately 44% of people aged 18 to 64 years exhibited attachment loss at one or more sites, with an average of 3.4 affected sites per person.
Do cytokines cause periodontitis?
Numerous studies have attempted to elucidate the cytokine networks involved in chronic periodontitis, but often with conflicting results ( Seymour and Gemmell, 2001 ). As with antibodies, cause and effect are not clear with most cytokines. With regard to tissue destruction, cytokines including IL-1, IL-6, and IL-18 appear to be important and their regulating cytokines IL-10 and IL-11 are usually concurrently raised. Experiments in animals and observations in humans appear to conflict. In humans TH1 responses appear to correlate with stable lesions, whereas in animals TH-2 responses appear to correlate best with protection. Thus, a number of studies have reported decreased TH-1 responses in periodontal disease and lower levels of IL-2 in the gingival crevicular fluid of periodontitis sites compared with healthy sites ( Pilon et al., 1991 ). Consistent with this is a demonstration that gingival mononuclear cells from adult periodontitis patients produce IL-4 and IL-5 but not IL-2. It is probable that the nature of the response is actually determined by the antigen presenting cell, which determines the nature of the cytokine profile.
Is periapical lesion asymptomatic or asymptomatic?
Patients often give a history of intermittent pain. The associated tooth may be asymptomatic, or it may be mobile or sensitive to percussion. More often, however, the periapical lesion arises in the chronic form de novo; in this case, it may be asymptomatic.
periodontitis
inflammation of the periodontium, usually caused by specific pathologic bacteria that grow in the spaces between the gum and lower part of the tooth crown, and the host response to inflammation. If it continues unchecked the infection will spread to the bone in which the teeth are rooted.
periodontitis
Gum disease, pyorrhea gum disease Dentistry A condition caused by progression of gingivitis, with inflammation and infection of tooth ligaments and bones supporting teeth. See Juvenile periodontitis.
periodontitis
Inflammation of the PERIODONTIUM. This may be centred mainly around the root of the tooth (apical periodontitis) or may be a persistent (chronic) condition affecting the whole periodontium as a complication of severe gum inflammation (gingivitis). Treatment of apical periodontitis is by drilling to drain any pus present and filling.
Periodontitis
A gum disease that destroys the structures supporting the teeth, including bone.
How do you know if you have periodontitis?
Signs and symptoms of periodontitis can include: Swollen or puffy gums. Bright red, dusky red or purplish gums. Gums that feel tender when touched. Gums that bleed easily. Pink-tinged toothbrush after brushing. Spitting out blood when brushing or flossing your teeth. Bad breath. Pus between your teeth and gums.
What is the sticky film that forms when you have periodontitis?
In most cases, the development of periodontitis starts with plaque — a sticky film composed mainly of bacteria. If left untreated, here's how plaque can eventually advance to periodontitis:
How to get rid of plaque on gums?
Brushing your teeth twice a day and flossing once a day removes plaque, but plaque re-forms quickly. Plaque can harden under your gumline into tartar (calculus) if it stays on your teeth. Tartar is more difficult to remove and it's filled with bacteria.
What is the name of the infection that can cause tooth loss?
Open pop-up dialog box. Close. Periodontitis. Periodontitis. Periodontitis is a severe gum infection that can lead to tooth loss and other serious health complications. Periodontitis (per-e-o-don-TIE-tis), also called gum disease, is a serious gum infection that damages the soft tissue and, without treatment, can destroy the bone ...
What causes dry mouth and gums?
Genetics. Certain medications that cause dry mouth or gum changes. Conditions that cause decreased immunity, such as leukemia, HIV / AIDS and cancer treatment. Certain diseases, such as diabetes, rheumatoid arthritis and Crohn's disease.
Can gingivitis be reversed?
Gingivitis can be reversed with professional treatment and good home oral care. Ongoing gum inflammation can cause periodontitis, eventually causing pockets to develop between your gums and teeth that fill with plaque, tartar and bacteria. In time, these pockets become deeper, filling with more bacteria.
Can you lose teeth from a deep infection?
In time, these pockets become deeper, filling with more bacteria. If not treated, these deep infections cause a loss of tissue and bone, and ultimately you may lose one or more teeth. Also, ongoing chronic inflammation can put a strain on your immune system.