Full Answer
What are the 3 mechanisms of hemostasis?
What is Hemostasis | Its Mechanism in 4 Stages
- Vasoconstriction. In these stages, the injured blood vessel’s channel gets narrow so as to minimize the blood flow. ...
- Plug formation by platelets. The sticky platelets adhere to each and release adenosine diphosphate ( ADP ). ...
- Coagulation. In this stage, another layer of the cover is formed on the previous platelet plug formed. ...
- Fibrinolysis. ...
What are the five steps of hemostasis?
What are the five steps of homeostasis?
- First step. Stimulus; a stimulus occurs such as a change in in body temperature.
- Second step. Receptors; the stimulus is acknowledged by the receptors.
- Third step.
- Fourth step.
- Fifth step.
- Final step.
- Negative Feedback.
- Positive Feebback.
What are the steps of hemostasis?
What are the five steps of hemostasis?
- Vessel Spasm.
- Formation of Platelet Plug.
- Blood Coagulation.
- Clot Retraction.
- Clot Dissolution (Lysis)
What are the three steps of hemostasis Quizlet?
- Vessel Spasm.
- Formation of Platelet Plug.
- Blood Coagulation.
- Clot Retraction.
- Clot Dissolution (Lysis)
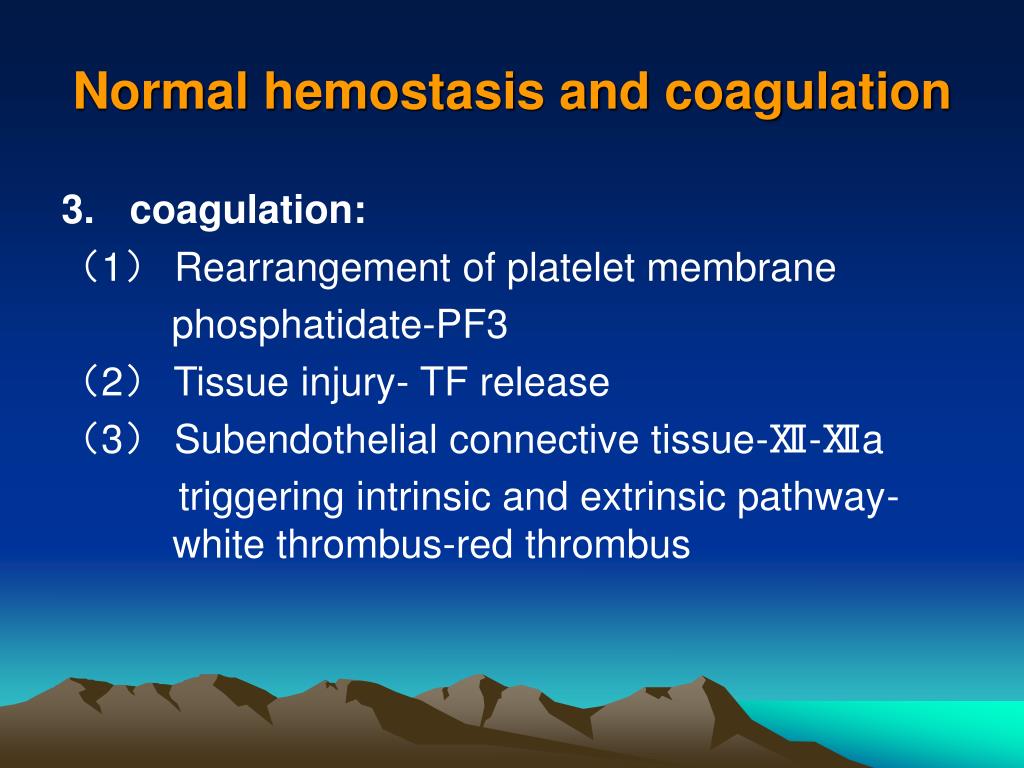
What is coagulation in hemostasis?
Coagulation (or clotting) is the process through which blood changes from a liquid and becomes thicker, like a gel. Coagulation is part of a larger process called hemostasis, which is the way that the body makes bleeding stop when it needs to.
What is the coagulation phase of hemostasis?
The mechanism of hemostasis can divide into four stages. 1) Constriction of the blood vessel. 2) Formation of a temporary “platelet plug." 3) Activation of the coagulation cascade. 4) Formation of “fibrin plug” or the final clot.
What are the coagulation process?
Coagulation is the chemical water treatment process used to remove solids from water, by manipulating electrostatic charges of particles suspended in water. This process introduces small, highly charged molecules into water to destabilize the charges on particles, colloids, or oily materials in suspension.
What is coagulation and what is its function?
Coagulation, also known as clotting, is the process by which blood changes from a liquid to a gel, forming a blood clot. It potentially results in hemostasis, the cessation of blood loss from a damaged vessel, followed by repair.
Why is coagulation important?
Blood clotting, or coagulation, is an important process that prevents excessive bleeding when a blood vessel is injured. Platelets (a type of blood cell) and proteins in your plasma (the liquid part of blood) work together to stop the bleeding by forming a clot over the injury.
What are the factors of blood coagulation?
What Are The Twelve Blood Clotting Factors?Fibrinogen (Factor 1)Prothrombin (Factor 2)Thromboplastin (Factor 3)Calcium (Factor 4)Proaccelerin or Labile Factor (Factor 5)Stable Factor (Factor 6)Antihemophilic Factor (Factor 8)Christmas Factor (Factor 9)More items...
What is an example of coagulation?
Examples of Coagulation Milk proteins coagulate to thicken the mixture that forms yogurt. Blood platelets coagulate blood to seal a wound. Pectin gels (coagulates) a jam. Gravy coagulates as it cools.
What is another word for coagulation?
In this page you can discover 33 synonyms, antonyms, idiomatic expressions, and related words for coagulation, like: clotting, thickening, jellification, curdling, congealing, congelation, condensation, concretion, caseation, blood-clot and gelling.
What are the five phases of coagulation?
Terms in this set (5)phase one- vascular phase. vasoconstriction, vessels respond by trying to reduce blood flow to the area.phase two- platelet phase. ... phase three- coagulation phase. ... phase four- clot retraction. ... phase five- fibrinolysis.
What are the five phases of coagulation?
Terms in this set (5)phase one- vascular phase. vasoconstriction, vessels respond by trying to reduce blood flow to the area.phase two- platelet phase. ... phase three- coagulation phase. ... phase four- clot retraction. ... phase five- fibrinolysis.
What are the 5 stages of hemostasis?
Terms in this set (16)1) Vessel Spasm. ... 2) Formation of Platelet Plug. ... 3) Blood Coagulation. ... 4) Clot Retraction. ... 5) Clot Dissolution (Lysis) ... Collagen. ... vWF. ... ADP.More items...
What does coagulation mean in medical terms?
Definition of coagulation : the process of becoming viscous or thickened into a coherent mass : the forming of clots (as in blood or cream) : the process of coagulating … an incision is made on the skin of the forearm with a spring-loaded device, and the time to coagulation is measured.— Lawrence L. K. Leung.
What are the three types of hemostasis?
Hemostasis can be subdivided into three sequential processes: primary hemostasis, secondary hemostasis, and tertiary hemostasis. In primary hemostasis the interaction of the injured endothelium with von Willebrand factor (VWF), and platelets is crucial for the formation of a platelet plug at the injury site.
What is the difference between hemostasis and coagulation?
The key difference between hemostasis and coagulation is that hemostasis is the overall process which stops bleeding due to a trauma while coagulation is the last step of hemostasis which forms a blood clot to block the hole in vascular tissue.
What is Hemostasis?
Hemostasis is a natural process that occurs to prevent excessive bleeding following an injury. It is the process of natural blood clotting, which acts as the first stage of wound healing. There are several mechanisms involved in hemostasis. They are vasoconstriction, tissue swelling, platelet aggregation and blood coagulation. As a result of vascular, platelet and plasma factors, the bleeding is arrested in the injured blood vessel by hemostasis process. The hemostatic system maintains blood in a liquid state under physiological conditions and also creates blood clots or fibrin clots when there is a vessel injury.
What are the two types of hemostasis?
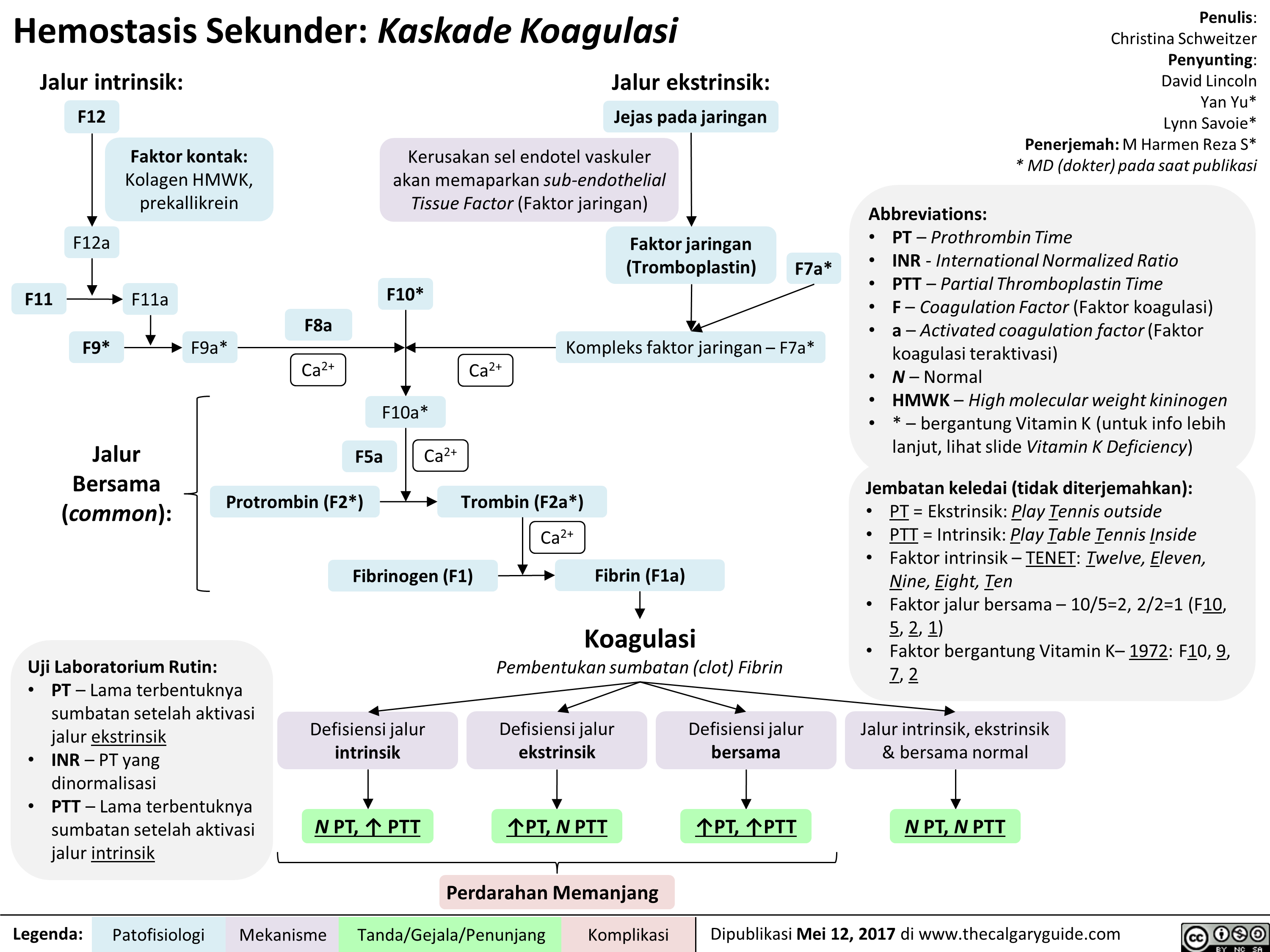
Hemostasis can be categorized into two types named primary hemostasis and secondary hemostasis. Coagulation can be categorized into intrinsic pathway of blood clotting and extrinsic pathway of blood clotting. Disorders. Hemostasis can show abnormalities due to platelet disorders.
What is the final step of hemostasis in which a stable blood clot is formed by platelets?
Coagulation is the final step of hemostasis in which a stable blood clot is formed by platelets and insoluble fibrin network.
How is blood coagulation accomplished?
Blood coagulation is accomplished by making a blood clot. A blood clot consists of a plug of platelets and a network of insoluble fibrin molecules. Blood coagulation is mainly done by the formation of a fibrin clot. Fibrin is an insoluble, fibrous and non-globular protein involved in the clotting of blood. It is the underlying fabric polymer of ...
How does blood coagulation work?
It is done by converting the specific circulating elements in the blood system into insoluble gel-like substances at the injured site. This is known as blood clotting or blood coagulation. Due to this process, continuous blood loss from injured blood vessels, tissues and organs is stopped, and possible complications are prevented as soon as possible. Blood coagulation is accomplished by making a blood clot. A blood clot consists of a plug of platelets and a network of insoluble fibrin molecules.
What is the process of stopping bleeding?
Hemostasis is a natural process which is activated to stop bleeding from the injury site. It occurs via three ways. Blood clotting or blood coagulation is the final step of hemostasis. The hole of the vascular system is blocked by a blot clot formed by platelets and coagulating factors. The key difference between hemostasis and coagulation is ...
What is the process of blood changing from a liquid to a gel?
Coagulation (also known as clotting) is the process by which blood changes from a liquid to a gel. It potentially results in hemostasis, the cessation of blood loss from a damaged vessel, followed by repair.
What is the process of blood exposure to the space under the endothelium?
Exposure of blood to the space under the endothelium initiates two processes: changes in platelets, and the exposure of subendothilial tissue factor to plasma Factor VII, which ultimately lead s to fibrinformation.
What is the term for platelets that form a plug at the site of injury?
Platelets immediately form a plug at the site of injury; this is called primary hemostasis. Secondary hemostasis occurs simultaneously: Additionalcoagulation factors or clotting factors beyond Factor VII (listed below) respond in a complex cascade to form fibrin strands, which strengthen the platelet plug.
Is coagulation a protein?
Coagulation is highly conserved throughout biology; in all mammals, coagulation involves both a cellular ( platelet) and a protein (coagulation factor) component. The system in humans has been the most extensively researched and is the best understood.
What is the process of coagulation?
The process can be divided into the extrinsic and intrinsic pathways. The extrinsic pathway is normally triggered by trauma; the intrinsic pathway is triggered by internal damage to the vessel walls. Both of these pathways merge into a third known as the common pathway. Each of the three pathways depends on the 12 known clotting factors.
What are the steps of hemostasis?
The process includes three main steps: the vascular spasm of the vessel damaged, the formation of a platelet plug, and coagulation.
What happens to the connective tissue during a vascular spasm?
During the vascular spasm, the connective tissues of the vessel constrict and pull away from its surrounding tissues. The formation of a platelet plug occurs as platelets become stuck to the now exposed layers of connective tissues and collagen fibers. As more platelets pass by the damaged area, more platelets become stuck to the growing mass of cells. Coagulation occurs as fibrin threads are networked together and trap blood cells as they pass by the site of injury. The presence of the fibrin threads plus multiple clotting factors form a strong, durable seal to the blood vessel.
How do platelets stick together?
As platelets pass by the area of the damaged vessel, they contact the normally covered layers of connective tissue and collagenous fibers. These layers are now exposed due to the vessel's damage, and the platelets start to stick together as they bind to the exposed collagen and endothelial lining. The clumping together of platelets is further stabilized by von Willebrand factor, a glycoprotein found within the blood plasma. As the clump grows, the platelets release various substances to reinforce the plug including ADP (to help additional platelets stick to the growing plug) and serotonin (to maintain vasoconstriction).
Why is it difficult to clot blood?
Another reason that could impair the blood's ability to clot is the inadequate production of functional amounts of one or more clotting factors. This is the case in the genetic disorder hemophilia. This disorder results in the inability to synthesize sufficient quantities of clotting factor VIII. The genetic roots of hemophilia are found in the X chromosome and are typically passed from a healthy (carrier) mother to her male offspring. Patients with hemophilia bleed from even minor internal and external wounds and leak blood into joint spaces after exercise and into urine and stool. Regular infusions of clotting factors isolated from healthy donors can help prevent bleeding in hemophiliac patients.
What is the process of forming a blood clot?
Coagulation is the process of forming a blood clot. The plasma protein fibrinogen is converted into a non-globular and insoluble protein called fibrin. Fibrin is created in threads, which results in a mesh that traps platelets and erythrocytes that travel through it. The final product is a gelatinous and durable clot.
How long does hemostasis last?
The longitudinal layers pull the vessel away from its surrounding tissues; the circular layers act to constrict the flow of blood in general. This step of hemostasis may last several minutes to several hours.
What is hemostasis?
Hemostasis is your body’s normal reaction to an injury that causes bleeding. This reaction stops bleeding and allows your body to start repairs on the injury. This capability is essential to keep you alive, particularly with significant injuries. However, in uncommon cases, the processes that control hemostasis can malfunction, causing potentially serious — or even dangerous — problems with bleeding or clotting.
How does hemostasis work?
Hemostasis combines the terms “hemo” (meaning “blood”) and “stasis” (meaning “standing still”). In this context, it’s the term for how your body stops bleeding. Rather than being just a single process, hemostasis is actually a collection of several processes. Though they look like separate processes, these all happen at the same time when your body forms a blood clot.
What causes hemostasis?
Without normal hemostasis, even minor injuries could cause dangerous blood loss. An example of this is hemophilia, a condition where hemostasis doesn't work properly and blood can't clot effectively. Any break in your skin is also a risk for germs to enter your body. Clots help reduce that risk by sealing the injury.
How are hemostasis problems diagnosed?
A healthcare provider — such as a hematologist — can diagnose blood clotting problems based on your symptoms and blood tests that analyze the clotting-related components in a sample of your blood.
When should I call a doctor about problems with clotting?
Hypercoagulability can happen with a variety of different symptoms depending on where and when an abnormal clot develops . Examples of this include:
Why do we need a coagulation test?
Coagulation tests are useful in monitoring people who take medications that affect clotting ability. Coagulation tests are also sometimes recommended before surgery.
What are the side effects of a coagulation test?
The side effects of a coagulation test are generally minor. You may have slight soreness or bruises at the site. The risks include lightheadedness, pain, and infection. If you have experience excessive bleeding, the procedure will be carefully monitored. The sample will be sent to a laboratory for testing and analysis.
What does a clotting test do?
Coagulation Tests. Clotting is what prevents excessive bleeding when you cut yourself. But the blood moving through your vessels shouldn’t clot. If such clots form, they can travel through your bloodstream to your heart, lungs, or brain. This can cause a heart attack, stroke, or even death. Coagulation tests measure your blood’s ability ...
What causes a lot of bleeding?
Clotting disorders can cause a dangerous amount of bleeding or clotting. If your doctor suspects you have a clotting disorder, they may recommend one or more coagulation tests. These tests measure various proteins and how they function. Conditions that can cause coagulation problems include: liver disease.
What is fibrinogen level?
Fibrinogen level. Fibrinogen is a protein made by your liver. This test measures how much fibrinogen is in your blood. Abnormal results may be a sign of excessive bleeding or hemorrhage, fibrinolysis, or placental abruption, which is a separation of the placenta from the uterine wall.
What does factor V mean in a blood test?
This test measures Factor V, a substance involved in clotting. An abnormally low level may be indicative of liver disease, primary fibrinolysis (a breakdown of clots), or disseminated intravascular coagulation (DIC).
What does CBC mean in medical terms?
Complete blood count (CBC) Your doctor may order a complete blood count (CBC) as part of your routine physical. The results of the test can alert your doctor if you have anemia or a low platelet count, which can interfere with your ability to clot.
