The list of Sentinel Events includes, but is not limited to:
- Stage 3, 4, and unstageable pressure ulcer
- Patient fall with serious injury or death
- Unanticipated death with 48 hours of treatment
- Unanticipated death
- Wrong site surgery
Can you identify a sentinel event?
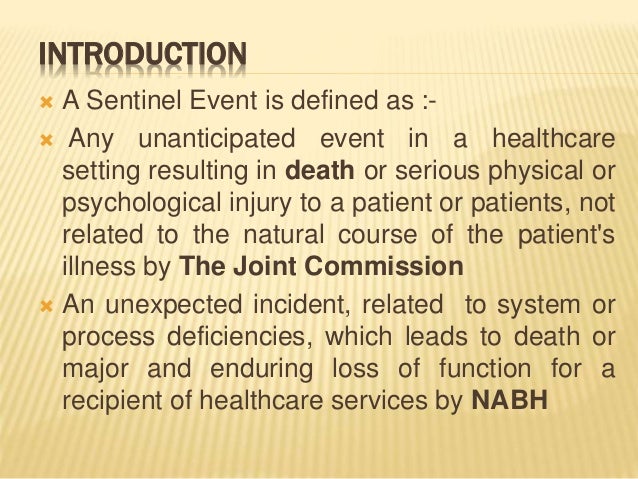
A sentinel event is a Patient Safety Event that reaches a patient and results in any of the following: Death. Permanent harm. Severe temporary harm and intervention required to sustain life An event can also be considered sentinel event even if the outcome was not death, permanent harm, severe temporary harm and intervention required to sustain ...
Is it a real sentinel event?
The Joint Commission defines a sentinel event as an unexpected occurrence involving death, serious physical or psychological injury. The event can result in death, permanent harm, or severe, temporary harm. The term sentinel refers to a system issue that may result in similar events in the future.
What does sentinel event stand for?
The Joint Commission defines a sentinel event as “an unexpected occurrence involving death or serious physical or psychological injury, or the risk thereof” (The Joint Commission, 2012, p. 1). “Risk thereof” refers to incidents for which a recurrence would involve a significant risk of serious adverse outcome.
What is a reviewable sentinel event?
reviewable sentinel events. - the event resulted in an unanticipated death or major permanent loss of function not related to the natural course of the patient's illness or underlying condition.

What are some examples of sentinel events?
The most common sentinel events are wrong-site surgery, foreign body retention, and falls. [3] They are followed by suicide, delay in treatment, and medication errors. The risk of suicide is the highest immediately following hospitalization, during the inpatient stay, or immediately post-discharge.
What are the top 10 sentinel events?
10 most common sentinel eventsPatient suicide: 382.Operative/postoperative complication: 330.Wrong-site surgery: 310.Medication error: 291.Delay in treatment: 172.Patient fall: 114.Patient death or injury in restraints: 113.Assault, rape, or homicide: 89.More items...
What is the difference between an adverse event and a sentinel event?
Purpose of Policy An Adverse Event is a serious, undesirable and usually unanticipated patient safety event that resulted in harm to the patient but does not rise to the level of being sentinel. A No Harm event is a patient safety event that reaches the patient but does not cause harm.
What is one of the top 3 root causes of sentinel events?
According to the Joint Commission, the most common cause of sentinel events in healthcare includes unintended retention of a foreign object, fall-related events, and performing procedures on the wrong patient.
Is a fall with fracture a sentinel event?
Specifically, only those falls that meet the Joint Commission definition would qualify as sentinel events. Most importantly, falls with injury are a significant patient safety problem. Falls with serious injury are consistently among the top ten sentinel event reports to TJC.
Is elopement a sentinel event?
Elopement can be a sentinel event as defined by the Joint Commission when the elopement results in temporally related death such as suicide, accidental death or homicide or results in a major permanent loss of function.
Do all sentinel events have to be reported?
Self-reporting a sentinel event is not required and there is no difference in the expected response, time frames, or review procedures whether the hospital voluntarily reports the event or The Joint Commission becomes aware of the event by some other means.
What are the 3 common factors of an adverse event?
The most common contributing factors were (i) lack of competence, (ii) incomplete or lack of documentation, (iii) teamwork failure and (iv) inadequate communication. Conclusions: The contributing factors frequently interacted yet they varied between different groups of serious adverse events.
Is a near miss considered an adverse event?
A near miss is defined as "any event that could have had adverse consequences but did not and was indistinguishable from fully fledged adverse events in all but outcome." (Some studies use the related terms "potential adverse event" and "close call.") In a near miss, an error was committed, but the patient did not ...
What happens after a sentinel event?
Handling a sentinel event If the event involves medical equipment, that item must immediately be taken out of service, bagged, and labeled for investigation. Next, the event must be communicated up the chain of leadership, and an occurrence report (or other report) must be submitted as required by the facility.
How long do you have to report a sentinel event?
Submit its comprehensive systematic analysis and corrective action plan to The Joint Commission, or otherwise provide its response to the sentinel event using an approved methodology within 45 business days of the known occurrence of the event for Joint Commission evaluation.
What is considered a patient safety event?
A patient safety event is defined as any process, act of omission, or commission that results in hazardous healthcare conditions and/or unintended harm to the patient [ 1 ]. Reporting patient safety events is a useful approach for improving patient safety [ 2 ].
What is the most common sentinel event reported to Joint Commission?
Unintended Retention of Foreign Object (URFO) is one of the most frequently reported sentinel events to The Joint Commission.
Which example qualifies as a sentinel event quizlet?
Patient suicide is a sentinel event. Which of the following is the best definition of "sentinel event"? A sentinel event is an unexpected incident that involves death or serious injury. Incident reports ensure that incidents are recorded and tracked, so that future incidents can be prevented.
What is reviewable sentinel event?
# Rape, as a reviewable sentinel event, is defined as unconsented sexual contact involving a resident and. another resident, staff member, or other perpetrator while being treated or on the premises of the. health care organization, including oral, vaginal, or anal penetration or fondling of the resident's sex.
Which of the following is the best example of an adverse event?
Which of the following is the best example of an adverse event? A patient receives an overdose of medication. Which of the following is the best definition of "adverse event"? An event where patient safety has been or might be affected.
What is sentinel event?
The Joint Commission defines a sentinel event as an unexpected occurrence involving death, serious physical or psychological injury. The event can result in death, permanent harm, or severe, temporary harm. The term sentinel means a system issue that may result in similar events in the future.
What is a serious reportable event?
The National Quality Forum defined the term serious reportable events as “preventable, serious, and unambiguous adverse events that should never occur.”. These events are also termed as never events. Previously, sentinel events included events that occurred only to patients.
What is sentinel event?
The Joint Commission defines a sentinel event as an unexpected occurrence involving death, serious physical or psychological injury.[1] The event can result in death, permanent harm, or severe, temporary harm. The term sentinel refers to a system issue that may result in similar events in the future. The National Quality Forum defined the term serious reportable events as “preventable, serious, and unambiguous adverse events that should never occur.” These events are also termed as never events. Previously, sentinel events included events that occurred only to patients. In 2013, the concept was expanded to include “harm events” to the staff, visitors, and vendors on the organization’s premises.
When did the sentinel event policy start?
All healthcare organizations should have a policy for responding to a sentinel event. In 1996 , the Joint Commission instituted a formal sentinel event policy. It partners with the hospitals that have experienced a sentinel event in the investigation, analysis, and development of corrective action plans.[7] The policy has the following goals:
What is a semos?
SEMOS is a quantifiable measure to evaluate if the action plan was effective and sustained. It has a numerator and denominator. The organization follows up on the data via chart audit and observation to measure compliance. Every organization should have a clear framework for reporting and responding to a sentinel event that is non-punitive, fosters teamwork, and promotes a just culture.
Is reporting sentinel events voluntary?
Reporting a sentinel event to the Joint Commission is voluntary. [8] The advantages of reporting the sentinel event include:[2]
What is sentinel event?
A sentinel event is "any unanticipated event in a healthcare setting that results in death or serious physical or psychological injury to a patient, not related to the natural course of the patient's illness". Sentinel events can be caused by major mistakes and negligence on the part of a healthcare provider, ...
What are the advantages of reporting sentinel events to the Joint Commission?
Advantages of reporting sentinel events to The Joint Commission are: Adding to the database with dissemination to other health care facilities, preventing other adverse events.
How long do you have to notify the FDA of a sentinel event?
In addition, healthcare organizations are required to notify the Food and Drug Administration (FDA) and device manufacturers within 10 days of a sentinel event caused by a medical device, according to the Safe Medical Device Act of 1990. Statistics of sentinel events are recorded and published by the FDA's MedWatch program.
Do you report sentinel incidents to the Joint Commission?
Each accredited organization is encouraged, but not required, to report any sentinel event to The Joint Commission. However, the organization is expected to prepare a root cause analysis and action plan within 45 calendar days of the event.
What is Sentinel Events?
The Sentinel Events team publishes a quarterly newsletter that focuses on key patient safety issues identified by covered facilities in the state , as well as those issues that have been identified nationally. The newsletters include information and links to tools that are available to facilities as a means of assisting in the promotion of their patient safety programs.
How to contact the Sentinel?
If you have determined that a Sentinel Event has occurred, you must fill out and submit the Sentinel Event Notification and Near Miss Reporting Form (Word), or contact the Sentinel Events team at one of the following numbers: Sentinel Event Hotline - (207) 287-5813. Sentinel Event Fax - (207) 287-3251.
What is the phone number for the Sentinel?
Sentinel Event Fax - (207) 287-3251. Main Office Phone - (207) 287-9300. This notification to the Division of Licensing & Certification must occur one business day after the Sentinel Event occurred or was discovered.
When do you have to submit a Sentinel 2021?
Healthcare providers who are required to report Sentinel Events must submit the Sentinel Events 2021 Annual Attestation (Word) form by January 30th each year. This attestation affirms that the healthcare provider reported all of the Sentinel Events in their facilities for the prior year.

Overview
A sentinel event is "any unanticipated event in a healthcare setting that results in death or serious physical or psychological injury to a patient, not related to the natural course of the patient's illness". Sentinel events can be caused by major mistakes and negligence on the part of a healthcare provider, and are closely investigated by healthcare regulatory authorities. Sentinel events are identified under The Joint Commission (TJC) accreditation policies to help aid in root c…
Specific events requiring review
Sentinel events include "unexpected occurrences involving death or serious physical or psychological injury, or the risk thereof". They also include the following, even if death or major loss of function did not occur:
• Infant abduction
• Release of an infant to an incorrect family
Actions and reporting
Participation is necessary by the leadership of TJC accredited healthcare organizations and by the persons closely involved in the systems under review. Causal factors are analyzed, focusing on systems and processes, not individual performance. Potential improvements, called an "action plan", are identified and implemented to decrease the likelihood of such events in the future. Each accredited organization is encouraged, but not required, to report any sentinel event to The Join…
Joint Commission actions
After review of the accredited facility's report on the sentinel event, The Joint Commission issues an Official Accreditation Decision Report that may modify the organization's current accreditation status, assign an appropriate "measure of success", or a require follow-up survey within six months. A healthcare facility that fails to complete a root cause analysis of the sentinel event and action plan within the time frame can be placed on "Accreditation Watch" by the Joint Commissi…
External links
• TJC Sentinel Events Policy and Procedure