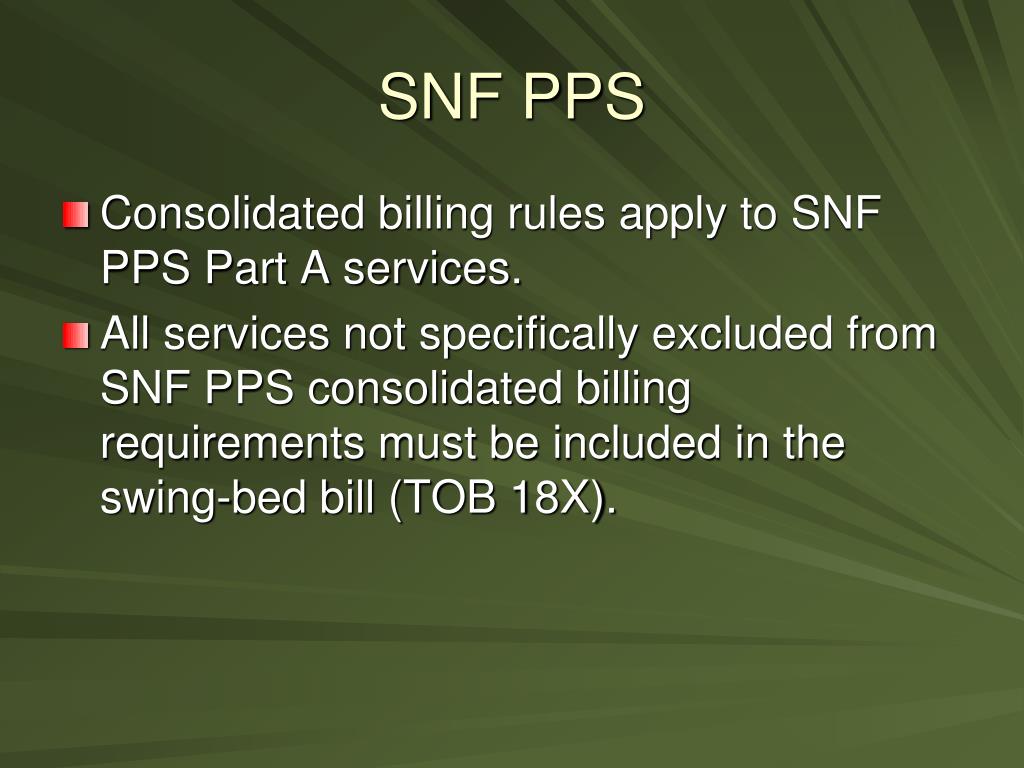
Consolidated billing is a system in which all care services that qualify for payment under the Prospective Payment System (PPS) are lumped together into a single package. This lump sum includes all room and board charges as well as all ancillary services, such as physical therapy, occupational therapy, and speech therapy.
Full Answer
What is consolidated billing?
The consolidated billing requirement confers on the SNF the billing responsibility for the entire package of care that residents receive during a covered Part A SNF stay and physical, occupational, and speech therapy services received during a non-covered stay.
What services are excluded from consolidated billing?
Exception: There are a limited number of services specifically excluded from consolidated billing, and therefore, separately payable. For Medicare beneficiaries in a covered Part A stay, these separately payable services include: certain dialysis-related services, including covered ambulance transportation to obtain the dialysis services;
What is consolidated billing (CB) for SNFS?
Congress then enacted the Balanced Budget Act of 1997 (BBA), Public Law 105-33, Section 4432 (b), and it contains a Consolidated Billing (CB) requirement for SNFs. Under the CB requirement, an SNF itself must submit all Medicare claims for the services that its residents receive (except for specifically excluded services listed below).
What is included in consolidated billing for HHAs?
HHAs must bill for all supplies provided during the 60-day episode including those not related to the plan of care because of the consolidated billing requirements. Items such as urological supplies, ostomy supplies, and surgical dressings are included in Home Health Consolidated billing and cannot be separately billed to the DME MAC.
What does consolidated billing mean?
Consolidated billing covers the entire package of care that a resident would receive during a covered Medicare Part A stay. However, some categories of services have been excluded from consolidated billing because they are costly or require specialization.
What services are included in the consolidated billing of the SNF PPS?
The consolidated billing requirement confers on the SNF the billing responsibility for the entire package of care that residents receive during a covered Part A SNF stay and physical, occupational, and speech therapy services received during a non-covered stay.
Are CT scans excluded from consolidated billing?
*The service must be provided at the place of service listed for the category or it will not be excluded. For example, a CT scan provided at a hospital or CAH is excluded. A CT scan provided anywhere else is not excluded.
What chemo drugs are excluded from consolidated billing?
Chemotherapy is one of the four major categories of services excluded from SNF consolidated billing, but not all chemotherapy drugs are excluded. For example, fluorouracil, interferon, methotrexate, mesnex, leuprolide, and goserelin are included in SNF consolidated billing.
Is dialysis part of consolidated billing?
Consolidated Billing Requirement Medicare provides payment under the ESRD Prospective Payment System (PPS) for all renal dialysis services furnished to ESRD beneficiaries for outpatient maintenance dialysis.
Is dialysis excluded from consolidated billing?
services provided in renal dialysis facilities (RDFs) are also excluded from SNF consolidated billing.
What services are categorically excluded from SNF PPS Part A payment?
These excluded service categories include:Cardiac catheterization;Computerized axial tomography (CT) scans;Magnetic resonance imaging (MRIs);Ambulatory surgery that involves the use of an operating room;Emergency services;Radiation therapy services;Angiography; and.Certain lymphatic and venous procedures.
Is wound care part of consolidated billing?
Medicare payment for wound care services The SNF is required to bill these bundled services in a consolidated bill to the Part A Medicare administrative contractor. The bundled services cannot be billed separately.
Is radiation therapy excluded SNF consolidated billing?
Likewise, radiation therapy performed at a free-standing cancer center would be the SNF's responsibility, even though it's listed as an exclusion. This is because consolidated billing rules state this service only is excluded when performed in an outpatient hospital setting.
Are Medicare Advantage plans subject to consolidated billing?
Security Health Plan Medicare Advantage follows Consolidated Billing rules for members in a Medicare covered skilled nursing facility (SNF) stay.
Does Medicare Part A and B cover chemotherapy?
Medicare covers chemotherapy if you have cancer. Part A covers inpatient hospital stays, care in a skilled nursing facility, hospice care, and some home health care. covers it if you're a hospital inpatient. Part B covers certain doctors' services, outpatient care, medical supplies, and preventive services.
What is not paid by Medicare Part B while the patient is in a SNF?
While in the SNF, the patient will receive rehab services designed to strengthen the patient so that he can return home. Medicare does not pay for custodial care. Conversely, Medicare does pay for skilled nursing care… up to a certain number of days.
How are SNF claims billed?
Billing Requirements. SNFs bill Part A using CMS-1450 (also called UB-04) or its electronic equivalent. Send claims monthly, in order, and when the patient: Drops from skilled care.
How do you bill for hemodialysis?
The appropriate code to bill for any home dialysis modalities is 90966 (for patients 20 years and older) and RPA recommends using wherever the physician rendered the visit as the place of service. Is 90970 unit billable or must it be billed once per date of service?
How much does Medicare reimburse for dialysis?
After you pay the Part B yearly deductible, Medicare pays 80% of the fee and you pay the remaining 20%.
Why do we use modifier GZ?
The GZ modifier indicates that an Advance Beneficiary Notice (ABN) was not issued to the beneficiary and signifies that the provider expects denial due to a lack of medical necessity based on an informed knowledge of Medicare policy.
What is SNF medical term?
SKILLED NURSING FACILITY (SNF) DEFINED. An SNF is an institution or a distinct part of an institution (see §201.1), such as a skilled nursing.
What is the CPT code for skilled nursing?
The Current Procedural Terminology (CPT) code range for Nursing Facility Services 99304-99318 is a medical code set maintained by the American Medical Association.
What does Ltcf?
Long-term Care Facility Component.
Is radiation therapy excluded SNF consolidated billing?
Likewise, radiation therapy performed at a free-standing cancer center would be the SNF's responsibility, even though it's listed as an exclusion. This is because consolidated billing rules state this service only is excluded when performed in an outpatient hospital setting.
Does SNF consolidated billing apply to Medicare Advantage plans?
Consolidated billing is required for Medicare Advantage members who are receiving services in a: Part A covered SNF stay, which includes medical services as well as room and board. Part B non-covered SNF stay, in which the Part A benefits are exhausted, but certain medical services are still covered.
What is not paid by Medicare Part B while the patient is in a SNF?
While in the SNF, the patient will receive rehab services designed to strengthen the patient so that he can return home. Medicare does not pay for custodial care. Conversely, Medicare does pay for skilled nursing care… up to a certain number of days.
How are SNF claims billed?
Billing Requirements. SNFs bill Part A using CMS-1450 (also called UB-04) or its electronic equivalent. Send claims monthly, in order, and when the patient: Drops from skilled care.
What is consolidated billing?
The consolidated billing requirement confers on the SNF the billing responsibility for the entire package of care that residents receive during a covered Part A SNF stay and physical, occupational, and speech therapy services received during a non-covered stay. Exception: There are a limited number of services specifically excluded from consolidated billing, and therefore, separately payable.
What is separately payable for Medicare?
For Medicare beneficiaries in a covered Part A stay, these separately payable services include: physician's professional services;
When did Medicare mandate SNF stay?
In the Balanced Budget Act of 1997 , Congress mandated that payment for the majority of services provided to beneficiaries in a Medicare covered SNF stay be included in a bundled prospective payment made through the Part A Medicare Administrative Contractor (MAC) to the SNF.
Who should contact Part B MAC?
Physicians, non-physician practitioners, and suppliers should contact their Part B MAC or Durable Medical Equipment (DME) MAC with questions about SNF consolidated billing. There is also additional information about SNF consolidated billing on the CMS Medicare Learning Network (MLN) Publications webpage.
Is Medicare covered by SNF?
Medicare beneficiaries can either be in a Part A covered SNF stay which includes medical services as well as room and board, or they can be in a Part B non-covered SNF stay in which the Part A benefits are exhaust ed, but certain medical services are still covered though room and board is not.
What is consolidated billing?
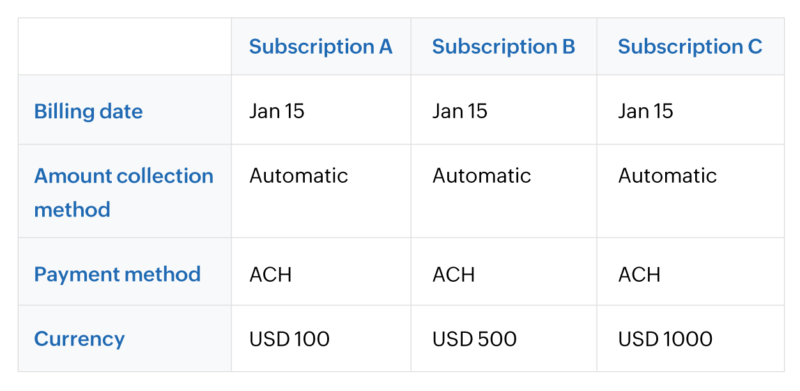
Consolidated billing is the method of combining multiple subscriptions of a customer into a single invoice. Typically, at the end of every subscription cycle, individual invoices are generated to collect payment from the customers. However, to avoid hassles of missed or delayed payments and to reduce the time and effort involved in generating individual invoices, they are grouped together as a consolidated invoice.
What are some factors to be considered before implementing consolidated billing?
There are a few factors to be considered before you decide to implement consolidated billing for your subscription business.
Why is it important to have a billing cycle before sending out consolidated invoices?
Before sending out consolidated invoices, it’s important to determine the billing cycle—especially when you are providing ongoing services and are working on long-term projects. This helps your customer clearly understand when the payments are expected to be made. It is advised to keep the billing cycle shorter, like weekly or monthly billing cycles over quarterly ones, as this is simple and easy to keep track of. Committing to long billing cycles might affect the steady flow of revenue into your business.
How are subscriptions A and C collected?
Here, the payments of subscriptions A and C are collected through credit card , while B and D are collected via ACH. Hence, this results in two consolidated invoices – one for subscriptions A and C and another for subscriptions B and D.
Can a new billing date be set up for all subscriptions to generate a consolidated invoice?
By another method, a new common billing date can be set up for all the subscriptions to generate a consolidated invoice.
Do all subscriptions have to be on the same billing date?
In order to consolidate all these subscriptions and generate a single invoice, they must share the same billing date – which is not the case here. This means, on the billing date of the first subscription which is on the 10th of every month, the consolidated invoice will be generated with the charges of the other three subscriptions prorated accordingly.
Can you group multiple subscriptions?
You can group multiple subscriptions of a customer and send out a single invoice. This simplifies the billing process when it comes to customers with multiple subscriptions. This guide will walk you through what consolidated billing is, how it can benefit your business, and some factors to be kept in mind while implementing consolidated billing.
Consolidated Billing Meaning and How it Differs From Previous Reimbursement Models
In 1997, Congress passed the Balanced Budget Act, which included requirements for consolidated billing, meaning SNFs would have to submit all Medicare claims for the services provided to their residents. As a result, now all Part A and Part B services are consolidated under a single payment, which is paid directly to the SNF.
Consolidated Billing SNF Reimbursements: 6 Tips for External Service Providers
As was noted above, consolidated billing SNF reimbursement changes were meant to prevent the disruption of care coordination, reduce the cases of duplicate billing, and help patients and residents avoid increased fees.
The Answer to What Is Consolidated Billing?
Consolidated billing is a system in which all care services that qualify for payment under the Prospective Payment System (PPS) are lumped together into a single package. This lump sum includes all room and board charges as well as all ancillary services, such as physical therapy, occupational therapy, and speech therapy.
What is consolidated billing?
The consolidated billing requirement confers on the SNF the billing responsibility for the entire package of care that residents receive during a covered Part A SNF stay and physical, occupational, and speech therapy services received during a non-covered stay. Exception: There are a limited number of services specifically excluded from consolidated billing, and therefore, separately payable.
What is separately payable for Medicare?
For Medicare beneficiaries in a covered Part A stay, these separately payable services include: physician's professional services;
What is Guidance for Requirement?
Guidance for requirement confers on the SNF the billing responsibility for the entire package of care that residents receive during a covered Part A SNF stay and physical, occupational, and speech therapy services received during a non-covered stay.
When did Medicare mandate SNF stay?
In the Balanced Budget Act of 1997 , Congress mandated that payment for the majority of services provided to beneficiaries in a Medicare covered SNF stay be included in a bundled prospective payment made through the Part A Medicare Administrative Contractor (MAC) to the SNF.
Who should contact Part B MAC?
Physicians, non-physician practitioners, and suppliers should contact their Part B MAC or Durable Medical Equipment (DME) MAC with questions about SNF consolidated billing. There is also additional information about SNF consolidated billing on the CMS Medicare Learning Network (MLN) Publications webpage.
Is Medicare covered by SNF?
Medicare beneficiaries can either be in a Part A covered SNF stay which includes medical services as well as room and board, or they can be in a Part B non-covered SNF stay in which the Part A benefits are exhaust ed, but certain medical services are still covered though room and board is not.
What is consolidated billing in ESRD?
The ESRD PPS implemented consolidated billing requirements for limited Part B items and services included in the ESRD facility’s bundled payment. Certain laboratory services, drugs and biologicals, equipment, and supplies are subject to consolidated billing and are no longer separately payable when provided to ESRD beneficiaries by providers other than the ESRD facility. Under consolidated billing, ESRD facilities are expected to furnish services, either directly, or under an arrangement with an outside supplier.
When a renal dialysis service is provided to an ESRD beneficiary by other providers, should that provider look?
When a renal dialysis service is provided to an ESRD beneficiary by other providers, that provider should look to the ESRD facility for payment, as opposed to submitting a claim to their Medicare Administrative Contractor (MAC).
Does Medicare pay for renal dialysis?
Medicare provides payment under the ESRD Prospective Payment System (PPS) for all renal dialysis services furnished to ESRD beneficiaries for outpatient maintenance dialysis. Therefore, ESRD facilities are responsible and paid for furnishing all renal dialysis services under the ESRD PPS directly or under arrangement.
Does an ESRD beneficiary have to submit a claim with an AY modifier?
For example, if an ESRD beneficiary also has cancer and has a laboratory test done related to cancer treatment, the laboratory should submit the claim with an AY modifier in order to receive separate payment.
What is consolidated billing?
Consolidated billing includes physical, occupational, therapies and speech-language pathology services received for any patient that resides in a SNF. Therefore the SNF must work with suppliers, physicians and other practitioners.
What services are excluded from consolidated billing?
There are a limited number of services that are excluded from consolidated billing, including services of a physician (except for physical, occupational therapies and speech-language pathology services), physician assistant, nurse practitioner and clinical nurse specialist when they are not an employee of the SNF and when these clinicians are working in collaboration with a physician or under their direct supervision.
How many files are in the Part B update for SNF consolidated billing?
There are four files in the Part B update for SNF consolidated billing:
Does Medicare bill for nursing home?
During the patient screening process, ask whether the patient is a resident of a nursing home. If yes, contact the nursing home and ask if the patient is in a covered Part A stay.
Is SNF a consolidated billing arrangement?
It is a best practice for a SNF to enter into an arrangement with any outside provider/supplier from which the SNF's residents received services subject to SNF consolidated billing. The absence of an agreement does not relieve the SNF of its overall responsibility to furnish directly or under arrangement for all services that are subject to the consolidated billing requirement.
What is a PPS in home health?
Home Health PPS. The Balanced Budget Act of 1997 requires consolidated billing of all home health services while a beneficiary is under a home health plan of care authorized by a physician. Consequently, billing for all such items and services will be made to a single home health agency (HHA) overseeing that plan.
What is medical services?
Medical services provided by an intern or resident-in-training of a hospital, under an approved teaching program of the hospital, in the case of a HHA that is affiliated or under common control with that hospital; and. Care for homebound patients involving equipment too cumbersome to take to the home.
What is the CB requirement for SNF?
Section 4432 (b) of the Balanced Budget Act (BBA) requires CB for the SNF. The CB requirement essentially confers on the SNF the Medicare billing responsibility for the entire package of care that its residents receive, except for a limited number of specifically excluded services.
What is included in the 60 day home health episode?
When a beneficiary is in a 60-day home health episode, these items are included in the PPS episode payment. HHA s must bill for all supplies provided during the 60-day episode including those not related to the plan of care because of the consolidated billing requirements. Items such as urological supplies, ostomy supplies, and surgical dressings are included in Home Health Consolidated billing and cannot be separately billed to the DME MAC.
How to check eligibility for 60 day home health?
Suppliers are encouraged to check eligibility either through NMP or the IVR for these 60-day Home Health episodes. When checking the Home Health Episode History in NMP, the "payer name and ID", provider number, episode start and end date and earliest and latest billing dates will display if an episode exits within the specific date range entered. If a specific date of service is in question, enter those dates or the beneficiary's eligibility will display for the current date.
What modifier is used for hospice?
Services should be coded with the GW modifier ("service not related to the hospice patient's terminal condition").
What is the date of delivery on a DME rental?
For capped rental items of DME where the supplier submits a monthly bill, the date of delivery on the first claim must be the "from" or anniversary date on all subsequent claims for the item.
Does CB apply to incident to services?
While CB excludes the types of services described above and applies to the professional services that the practitioner performs personally, the exclusion does not apply to physician “incident to” services
Can SNFs unbundle Medicare?
SNFs can no longer “unbundle” services that are subject to CB to an outside supplier that can then submit a separate bill directly to the Part B carrier. Instead, the SNF itself must furnish the services, either directly, or under an “arrangement” with an outside supplier in which the SNF itself (rather than the supplier) bills Medicare. The outside supplier must look to the SNF (rather than to Medicare Part B) for payment.