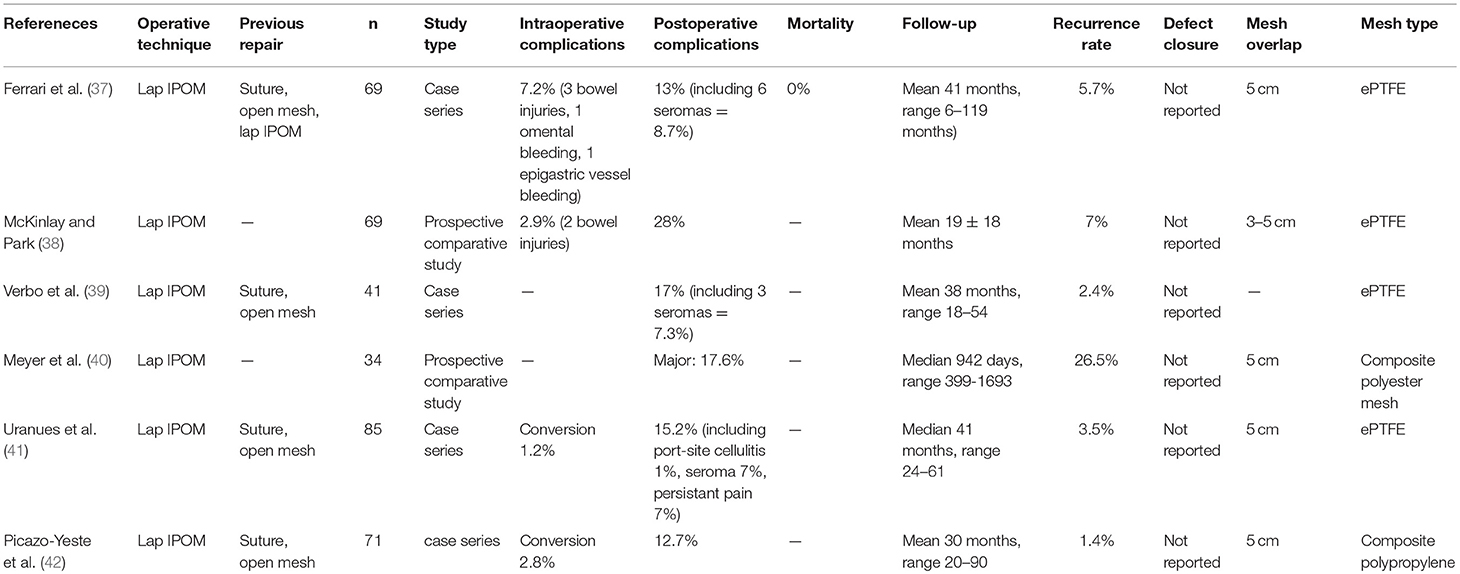
| CPT code | Descriptor | 2017 total RVU |
|---|---|---|
| 49580 | Repair umbilical hernia, younger than age 5 years; reducible | 9.46 |
| 49582 | Repair umbilical hernia, younger than age 5 years; incarcerated or strangulated | 13.34 |
| 49585 | Repair umbilical hernia, age 5 years or older; reducible | 12.85 |
What is CPT code for repair recurrent inguinal hernia?
The soft tissues get bulged out of the abdomen and then these tissues are removed again and again. The CPT code used for recurrent inguinal hernia repair is 49561.
Does CPT 49650 include mesh?
The code 49650 does not state that the mesh is included when performed, unlike the other codes in this catagory...is it understood that the mesh is included or should I be using another code to include mesh? If anyone can help I'm open for suggestions,
Can a hernia come back after surgery?
Yes, a hernia can return after it is repaired and it is called a ‘recurrent’ a hernia. It can happen to every surgeon. Recurrent hernias are formed after the successful surgery of a primary hernia. It can happen at any point in time, maybe within few days or weeks after the first surgery or after many years.
What are the symptoms or signs of an umbilical hernia?
Signs and Symptoms of Umbilical Hernia. Umbilical hernias appear as a bulge or swelling in the belly button area. The swelling may become more noticeable when the baby cries, and may become smaller or disappear when the baby is quiet. If a physician gently pushes on the bulge when a child is lying down and calm, it will usually get smaller or ...
What is the CPT code for open umbilical hernia repair with mesh?
49652 Laparoscopy, surgical, repair, ventral, umbilical, spigelian or epigastric hernia (includes mesh insertion, when performed); reducible.
Is umbilical hernia CPT code?
CPT frequently specifies separate codes to describe laparoscopic repair of reducible and incarcerated/strangulated hernias. For example, 49652 specifies repair of reducible ventral, umbilical, spigelian or epigastric hernias, while 49653 describes repair of incarcerated or strangulated hernias of identical types.
What is the CPT code for hernia repair?
Placement of mesh (49568) is an add-on code for incisional or ventral hernia repairs, performed via an open approach. The range of codes that CPT®code 49568 may be reported with is 11004-11006, 49560—49566. The facility may bill for mesh in other cases, but there is not a separate physician charge.
What is CPT code 49585 used for?
CPT® Code 49585 in section: Repair umbilical hernia, age 5 years or older.
What is the ICD-10 code for umbilical hernia?
ICD-10 code K42. 9 for Umbilical hernia without obstruction or gangrene is a medical classification as listed by WHO under the range - Diseases of the digestive system .
What is the CPT code 44005?
CPT® Code 44005 in section: Incision Procedures on the Intestines (Except Rectum)
What does CPT code 49650 mean?
CPT® 49650 in section: Laparoscopy, surgical.
What is procedure code 49560?
CPT® Code 49560 in section: Repair initial incisional or ventral hernia.
What is procedure code 49561?
CPT® Code 49561 in section: Repair initial incisional or ventral hernia.
When is add on code 49585 used hernia repair?
Answer: Repair of an umbilical hernia via an open approach is coded as 49585. Mesh placement may not be reported separately. Per CPT, mesh placement is only reported separately with repair of open Incisional hernias.
What is procedure code 15734?
CPT® Code 15734 in section: Muscle, myocutaneous, or fasciocutaneous flap.
What is an open umbilical hernia repair?
Open Hernia Surgery – Umbilical Umbilical hernia repairs are almost always best done open. During open surgery, a small incision is made in the crease under the belly button. The belly button is lifted off of the underlying muscle and fat. The hole in the muscle is exposed and a mesh is placed through the hole.
What is procedure code 49560?
CPT® Code 49560 in section: Repair initial incisional or ventral hernia.
What is procedure code 49561?
CPT® Code 49561 in section: Repair initial incisional or ventral hernia.
What is the CPT code 49505?
CPT® Code 49505 in section: Repair initial inguinal hernia, age 5 years or older.
What does CPT code 49650 mean?
CPT® 49650 in section: Laparoscopy, surgical.
What is the root operation for hernia repair?
The two main root operations for hernia repair are Q-Repair, which is assigned when mesh is not used, and U-Supplement, which is assigned when mesh is used. Note that a code using root operation U-Supplement stands by itself as a hernia repair procedure and no additional code is required or assigned to capture the repair or use of mesh.
What is mesh for hernia repair?
For hernia repair without mesh, Z-No Device is used. For hernia repair with mesh, mesh is considered a device. There are three types of mesh: 1) Most mesh is made of synthetic materials such as polypropylene, polyester, and PTFE; 2) Some mesh is bioengineered from donated human tissue, such as from cadavers, and; 3) Some mesh is bioengineered from animal tissue such as bovine and porcine tissue (eg, PermacolTM Surgical Implant). Although there are three types of mesh, there are currently only two options for the device value. Synthetic meshes use J-Synthetic Substitute. Meshes made of either human and animal tissues currently use K-Nonautologous Tissue.5
What is revision 44346?
44346 Revision of colostomy; with repair of paracolostomy hernia (separate procedure)
What are the two main root operations for abdominal wall repair?
3: Root Operation The two main root operations for abdominal wall repair are Q-Repair, which is assigned when mesh is not used, and U-Supplement, which is assigned when mesh is used.
Why is abdominal wall repair not coded separately?
Abdominal wall repair is not coded separately when an associated procedure is performed on an internal organ, because procedural steps necessary to close an operative site are considered integral.
Is abdominal wall repair the same as hernia repair?
In general, abdominal wall repair uses the same coding principles and the same code values as hernia repair. An abdominal wall repair is differentiated from a hernia repair by the ICD-10-CM diagnosis codes, not necessarily by the ICD-10-PCS procedure codes.
Is a hernia repair reported separately?
The hernia repair is separately reportable if it is performed at a site other than the incision and is medically reasonable and necessary. An incidental hernia repair is not medically reasonable and necessary and should not be reported separately.”.
Is CPT 49585 incidental to CPT 43880?
Anthem Central Region bundles C PT 49585 as incidental to CPT 43880 . The performance of an abdominal procedure includes the reimbursement for hernia repair. The CMS National Correct Coding Manual states:
What is the code for a hernia repair?
Voilà, you’re done. If it’s open, you have a bit more work to do, so turn to code range 49491–49611 for open hernia repair.
What determines correct coding of a hernia?
Another factor that determines correct coding is the clinical presentation of the hernia. When the contents of the hernia sac return to their normal location spontaneously or by gentle manipulation, the hernia is considered reducible. While moving the contents may make the hernia appear smaller or disappear, the weakened tissue still needs to be repaired to avoid recurrence of the hernia.
What is the CPT code for mesh?
Add-on code +49568 Implantation of mesh or other prosthesis for open incisional or ventral hernia repair or mesh for closure of debridement for necrotizing soft tissue infection (List separately in addition to code for the incisional or ventral hernia repair) can only be reported separately with codes 49560–49566 for incisional or ventral hernia repair and debridement codes 11040–11006.
What is the code for mesh removal?
Do not use add-on code +11008 Removal of prosthetic material or mesh, abdominal wall for infection (eg, for chronic or recurrent mesh infection or necrotizing soft tissue infection) (List separately in addition to code for primary procedure) to report mesh removal during hernia repair. Although it describes mesh removal, this code can only be used with 10180 Incision and drainage, complex, postoperative wound infection and debridement codes 11004–11006.
Why do surgeons use mesh?
Surgeons will often place a piece of prosthetic mesh to help strengthen the area of the abdominal wall being repaired and provide additional support to the damaged tissue. Hernia mesh is used in 90 percent of hernia surgeries and, when used and placed correctly, reduces the risk of recurrence.
What is abdominal surgery?
Surgery is directed at permanently closing off the orifice through which the abdominal contents protrude, after returning them to the abdominal cavity. Usually, an incision is made over the hernia and the hernia sac is dissected from any surrounding structures.
Why are incarcerated hernias more dangerous than incarcerated hernias?
Incarcerated hernias are more worrisome because they run a greater likelihood of becoming strangulated, which is when the blood supply to an incarcerated hernia is cut off as the vessels pass through the neck of the hernia. This is dangerous, due to the risk of gangrene when tissues die, and can be life-threatening if it isn’t treated.
When was the last update in hernia coding?
The last update in hernia coding was in 2009.
What is abdominal hernia?
An abdominal hernia is a protrusion of part of the intestines through a weakened section of the abdominal cavity; herniations can occur in other parts of the body, such as muscle herniations. This article addresses abdominal hernias. Surgery is directed at permanently closing off the orifice through which the abdominal structures protrude.
What is the CPT code for mesh placement?
If you are new to general surgery coding, read on. Placement of mesh (49568) is an add-on code for incisional or ventral hernia repairs, performed via an open approach. The range of codes that CPT ® code 49568 may be reported with is 49560—49566.
What is CPT code 49659?
CPT ® code 49659, unlisted laparoscopy procedure, hernioplasty, herniorrhaphy, herniotomy is reported when a CPT ® code does not exist for the type of repair performed.
Is a hernia surgically reduced?
Surgery is directed at permanently closing off the orifice through which the abdominal structures protrude. Sometimes, the hernia can be manually reduced, but this is not a permanent intervention. There isn’t a code for medical reduction of a hernia, it is part of an E/M service.
Can you report a ventral hernia repair separately?
If either an incisional or ventral hernia repair is done at the time of another abdominal procedure, through the same incision, do not separately report the hernia repair. It is considered inclusive of the other procedure.
What is the code for mesh incisional hernia repair?
Implantation of mesh or other prosthesis for open incisional or ventral hernia repair or mesh for closure of debridement for necrotizing soft tissue infection (List separately in addition to code for the incisional or ventral hernia repair) (Use 49568 in conjunction with 11004–11006, 49560–49566)
What is the CPT code for an inguinal hernia?
As identified in Table 1 only the codes for open repair of inguinal hernias (49491–49525) or umbilical hernias (49580–49587) have distinct codes based on the age of the patient. Until 1994, separate repair codes were used to report incarcerated hernias and strangulated hernias. These two patient presentations were combined in the 1994 CPT revision. Until 1994, separate codes were used to report different approaches to hernia repair, such as an inguinal approach versus an anterior extraperitoneal approach (Henry) for a femoral hernia repair. Beginning in 1994, all open hernia repair codes were categorized as reducible or incarcerated/strangulated, except for the rare lumbar hernia repair (49540) or rare spigelian hernia repair (49590).
How old is a baby when it has an inguinal hernia?
Repair, initial inguinal hernia, full term infant younger than age 6 months, or preterm infant older than 50 weeks postconception age and younger than age 6 months at the time of surgery, with or without hydrocelectomy; incarcerated or strangulated
How old is a child when they have an inguinal hernia repaired?
Repair, initial inguinal hernia, full term infant younger than age 6 months, or preterm infant older than 50 weeks postconception age and younger than age 6 months at the time of surgery, with or without hydrocelectomy; reducible. 6.20. 10.93. 49496.
What is hernia repair?
Hernia repair includes isolation and dissection of the hernia sac, reduction of intraperitoneal contents, fascial repair, and soft tissue closure. In 1993, the ACS submitted a code change proposal to the American Medical Association CPT Editorial Panel to revise hernia coding in 1994 based on several variables, including the following:
Why is a hernia considered incarcerated?
A hernia should be considered incarcerated if, at the time of the operation, it contains viscera that the surgeon must manually reduce. It should be considered strangulated if the incarcerated contents have evidence of ischemia due to compression of the vascular supply.
What is the code for mesh in a hernia?
Code 49568, Implantation of mesh or other prosthesis for open incisional or ventral hernia repair or mesh for closure of debridement for necrotizing soft tissue infection (List separately in addition to code for the incisional or ventral hernia repair), may be reported only once in addition to the open incisional or ventral hernia repair code (49560–49566), as applicable. Medicare rules do not permit appending modifier 50 to code 49568 for bilateral hernia repair. Code 49568 includes the work of placing the mesh, independent of the size of mesh used. It is the facility’s responsibility to report the type and size of mesh used; the surgeon only reports code 49568 .
What is the correct code for a hernia repair?
RATIONALE: In the CPT® Index, look up Hernia Repair/Inguinal/Initial, Child 5 Years or Older. You are referred to 49491, 49495–49500, and 49505 and 49507. Review the codes to choose the appropriate service. 49505 is the correct code. The repair was through an incision (not by laparoscopy) on an initial inguinal hernia on a patient over five years of age and the hernia was not incarcerated or strangulated. According to CPT® guidelines, “With the exception of the incisional hernia repairs (49560–49566), the use of mesh or other prosthesis is not separately reported.” It would be inappropriate to code the mesh in this scenario.
What are the different types of hernias?
Types of Hernia. • Incarcerated Hernia- hernia that is trapped in the abdominal wall. • Strangulated Hernia- An incarcerated hernia that becomes strangulated cutting the blood flow. Symptoms of this include nausea, high fever, sharp pains and swelling.
What is the National Correct Coding Initiative?
The National Correct Coding Initiative is a collection of bundling edits that are separated into two major categories: Comprehensive/Component Procedure Code edits and Mutual ly Exclusive Procedure Code edits.
Can a physician cancel a surgical procedure?
Used for surgical or radiological procedures in ASC. Due to extenuating circumstances or those that threaten the well‐ being of the patient, the physician may cancel a surgical or diagnostic procedure subsequent to the patient’s surgical preparation (including sedation when provided and being taken to the room where the procedure is to be performed), but prior to the administration of the anesthesia.
Is a hernia recurrent or initial?
Some types of hernias are further categorized as “initial” or “re current” based on whether or not the hernia has required previous repair (s). Additional variables accounted for by some of the codes include patient age and clinical presentation (reducible vs. incarcerated or strangulated). With the exception of the incisional hernia repairs (see ...
Is 49250 a separate procedure?
CPT code 49250 has a 'separate procedure' designation in CPT, so it is always incidental and bundled to another procedure in the same anatomical location and should never be billed in addition. Under NCCI, a modifier cannot be used to override this bundling.
Is a hernia repair reportable?
If a hernia repair is performed at the site of an incision for an open or laparoscopic abdominal procedure, the hernia repair (e.g., CPT codes 49560-49566, 49652-49657) is not separately reportable.
Did Medicare deny 49250?
Our surgeon did a umbilectomy and then a umbilical hernia was noted and was repaired. When billed 49250-umbilectomy and 49585-umbilical hernia repair, Medicare denied the 49250.