Common peroneal nerve dysfunction is a type of peripheral neuropathy (damage to nerves outside the brain or spinal cord). This condition can affect people of any age. Dysfunction of a single nerve, such as the common peroneal nerve, is called a mononeuropathy. Mononeuropathy means the nerve damage occurred in one area.
What causes peroneal nerve pain and how is it treated?
Peroneal tendonitis is inflammation in one or both of the tendons that connect your lower leg to your foot. It’s usually due to overusing the tendons, but it can also be the result of a sudden injury such as an ankle sprain. Pain and swelling in your peroneal tendons usually go away after several weeks of conservative treatments.
Does peripheral neuropathy ever get better?
Usually a peripheral neuropathy can’t be cured, but you can do a lot of things to prevent it from getting worse. If an underlying condition like diabetes is at fault, your healthcare provider will treat that first and then treat the pain and other symptoms of neuropathy. In some cases, over-the-counter pain relievers can help.
What causes peroneal nerve damage?
The peroneal nerve can be injured by trauma and nerve compression, including:
- Knee dislocation
- Knee or leg fracture
- Knee or hip replacement surgery
- Compression of the peroneal nerve in the leg
- Compression of the peroneal nerve by a nerve sheath tumor or nerve cyst
What are symptoms of peroneal nerve damage?
What You Need to Know
- Mild peroneal nerve injuries can cause numbness, tingling, pain and weakness.
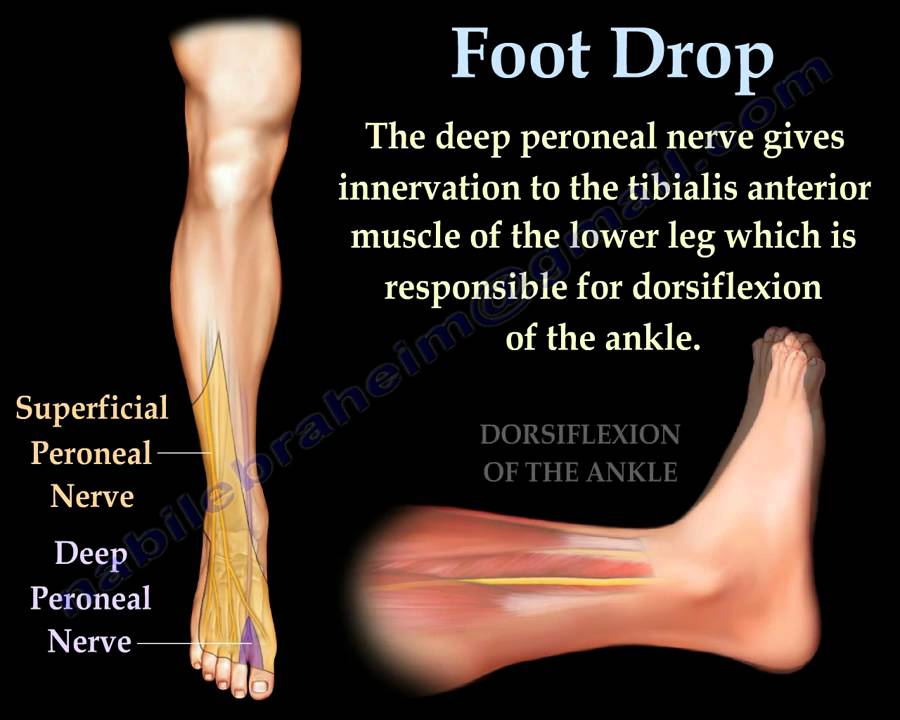
- More severe injuries can be characterized by a foot drop, a distinctive way of walking that results from being unable to bend or flex the foot upward at the ankle.
- Other neurological conditions, for example a herniated disc, can also cause foot drop.

How do you treat a deep peroneal nerve?
Nonsurgical treatments, including orthotics, braces or foot splints that fit inside the person's shoe, can bring relief. Physical therapy and gait retraining can help the person improve their mobility. Some injuries may require peripheral nerve surgery, including one or more of these procedures: Decompression surgery.
What are the symptoms of peroneal neuropathy?
SymptomsDecreased sensation, numbness, or tingling in the top of the foot or the outer part of the upper or lower leg.Foot that drops (unable to hold the foot up)"Slapping" gait (walking pattern in which each step makes a slapping noise)Toes drag while walking.Walking problems.Weakness of the ankles or feet.More items...
What causes deep peroneal nerve damage?
There are numerous traumatic and non-traumatic causes of peroneal nerve injuries, including knee dislocation, direct impact or cut on the fibular neck, fracture of the proximal fibula, compression by use of a tight plaster cast, or compression wrapping, prolonged bed rest, and regular crossing of the legs.
What does the deep peroneal nerve do?
It runs through the interosseous membrane and descends down the leg, between the extensor muscles of the foot, for which it provides supply. The nerve terminates around the ankle joint by dividing into lateral and medial terminal branches which innervate the muscles and skin of the foot.
Is peroneal neuropathy a disability?
Neuropathy is considered a disability by the SSA. The SSA refers to a medical guide called the Blue Book when evaluating eligibility for Social Security disability benefits.
Can peroneal nerve damage be cured?
Aim: Common peroneal nerve (CPN) injuries represent the most common nerve lesions of the lower limb and can be due to several causative mechanisms. Although in most cases they recover spontaneously, an irreversible damage of the nerve is also likely to occur.
What doctor treats peroneal nerve damage?
By taking a multidisciplinary approach to treatment, your surgeon will have access to other specialists—from intensivists and hospitalists, to endocrinologists and physical therapists—that will work closely together to diagnose and treat your condition.
Can peroneal nerve damage be permanent?
This condition is not normally life-threatening, but the pain can be uncomfortable. Decompression of the peroneal nerve may not fully resolve the pain associated with this condition. In some cases, if the injury to the nerve is severe, the disability may be permanent.
Can peroneal neuropathy reversed?
Peripheral neuropathy cannot be reversed.
How long does it take for a peroneal nerve to heal?
What is the recovery time after a common peroneal nerve decompression? The recovery time after a common peroneal nerve decompression at the knee is usually 3-4 months.
What muscles are supplied by the deep peroneal nerve?
The deep peroneal nerve supplies the following muscles:Tibialis anterior.Extensor digitorum longus.Peroneus tertius.Extensor hallucis longus (propius)Extensor digitorum brevis.Extensor hallucis brevis.
Where is the deep peroneal nerve located?
The deep peroneal nerve, also called the deep fibular nerve, is a peripheral nerve of the calf. It's a terminal branch of the common peroneal nerve, which is a branch of the sciatic nerve.
Where is peroneal nerve pain felt?
Injury to the common peroneal nerve results in a foot drop described as slapping or tripping [20]. Pain may occur at the site of compression as well as distally into the lateral leg. At times there may be a radiation of pain into the thigh [15].
How do you test the peroneal nerve?
0:131:45Common Peroneal Nerve Test - Supine - YouTubeYouTubeStart of suggested clipEnd of suggested clipAnd then invert the ankle. That's position you want to hold an ankle in throughout the entire text.MoreAnd then invert the ankle. That's position you want to hold an ankle in throughout the entire text. Now we're going to flex the hip while keeping the knee in extension.
How do you diagnose peroneal nerve damage?
Peroneal nerve dysfunction is typically diagnosed by a physical examination of the legs and feet. An MRI or CT scan may be used to confirm the compression of the nerve. Electrodiagnostic tests such as EMGs and NCVs may also be used to confirm the diagnosis.
How long does it take for the peroneal nerve to heal?
8. What is the recovery time after a common peroneal nerve decompression? The recovery time after a common peroneal nerve decompression at the knee is usually 3-4 months.
What is the deep peroneal nerve?
Rehabilitation. The deep peroneal nerve, also called the deep fibular nerve, is a peripheral nerve of the calf. It's a terminal branch of the common peroneal nerve, which is a branch of the sciatic nerve. The deep peroneal nerve contains both motor and sensory fibers.
Why do my feet drop?
Foot drop can also be caused by problems unrelated to the deep peroneal nerve, including a bone overgrowth in the spinal canal, or a tumor or cyst compressing the nerve along the sciatic or common peroneal nerves.
Which nerve is responsible for pulling the foot back?
By innervating the tibialis anterior, extensor hallucis longus, extensor digitorum longus, and fibularis tertius, the deep peroneal nerve is responsible for pulling the foot back—the opposite motion of pointing the toes. This motion, which is called dorsiflexion, is important for walking. Dorsiflexion is required both when your heel strikes ...
Which branch of the deep peroneal nerve connects to the extensor hallucis brevis?
The medial branch, which is a cutaneous (of the skin) nerve. The lateral and medial are the terminal branches of the deep peroneal nerve.
Which nerve sends off motor branches to several muscles in the calf?
The deep peroneal nerve sends off motor branches to several muscles in the calf, including: 1 . It also sends a branch to the ankle joint, then puts off two branches into the foot: The lateral branch, which connects to the extensor digitorum brevis and extensor hallucis brevis muscles.
Which nerve provides motor function to muscles?
The upper portion of the deep peroneal nerve provides motor function to muscles, while the lower portion provides both motor and sensory function to portions of the foot. 1
What test measures how fast electrical signals move through the nerves?
Nerve conduction tests , which measure how fast electrical signals move through the nerves
What is Peroneal Neuropathy?
Peroneal neuropathy occurs when the common peroneal nerve in the leg is injured. It may be damaged if the area around the knee is wounded or if there's been trauma in the hip. A problem with the common peroneal nerve often results in foot drop, which is the inability to lift the ankle, extend the toes, or to turn the foot outward.
How is Peroneal Neuropathy treated?
Splinting and bracing can be helpful in treating the foot drop while waiting for the peroneal nerve to recover.
Why does my foot drop?
A problem with the common peroneal nerve often results in foot drop, which is the inability to lift the ankle, extend the toes, or to turn the foot outward.
What is the rehabilitation of a peroneal neuropathy patient?
Rehabilitation of the patient with peroneal neuropathy at the fibular head (Table 42.11) should encompass the general principles of therapy outlined earlier. The initial rehabilitation encounter emphasizes obtaining a thorough history and identifying the patient's capabilities and limitations, and how these affect daily function. Assuming the peroneal nerve has not been completely transected, key aspects of rehabilitative care are to reduce inflammation, prevent further injury, and control pain while the nerve recovers.
What is the most common disorder mistaken for FNFH?
While the most common disorder mistaken for FNFH is L5 radiculopathy, clinical and neurologic involvement of non-fibular L5 innervated muscles such as the tibialis posterior, gluteus medius, tensor fasciae latae, and L5 multifidus muscles can help make this distinction. Other localizations which are less common are lumbosacral plexopathy and sciatic mononeuropathy (in the latter condition, the fibular division being more often and more severely involved than the tibial in many cases). Once the localization of common fibular neuropathy is established, the differential diagnosis includes trauma (as from blunt force trauma, fibula fracture, adduction injury with knee dislocation, and arthroscopic surgery), external compression (associated with bed rest, prolonged surgeries under general anesthesia, casting or bracing of the lower limb, leg crossing, prolonged positioning of the lower limbs in squatting, kneeling, or sitting cross-legged), acute ankle injury, mass lesions (such as ganglion cyst, Baker cyst, tumor, callus, or hematoma), entrapment in the fibular tunnel or in association with anterior compartment syndrome), vascular (popliteal aneurysm or vasculitis), involvement in diseases with multiple mononeuropathies (DM, multifocal motor neuropathy, hereditary neuropathy with liability to pressure palsies, or Hansen disease), profound weight loss, and idiopathic ( Stewart, 2010 ).
What is the most common cause of mononeuropathy in the lower limb?
Fibular (peroneal) neuropathy at the fibular head (FNFH) is the most common cause of mononeuropathy in the lower limb. The usual presentation is acute to subacute painless foot drop, with physical examination showing not only weakness of ankle dorsiflexion but also of toe extension and ankle eversion. Sensory deficits are typically limited to the foot dorsum and sometimes only foot dorsum skin immediately adjacent to the first interspace.
What is the most common manifestation of MMN?
Multifocal motor neuropathy (MMN) often presents symmetrically with weakness of the intrinsic hand muscles or wrist drop. Foot drop due to peroneal neuropathy is also a common manifestation of MMN, although it usually follows the involvement of the upper limbs. However, among lower limb mononeuropathies, peroneal neuropathy is the most common and is often manifested by conduction block due to segmental demyelination.
What nerve is involved in sciatica?
Partial sciatic nerve lesions usually affect the lateral division (peroneal nerve) more than the adjacent medial division (tibial nerve) due to greater vulnerability of the peroneal division of the sciatic nerve to physical injury. This often presents a diagnostic challenge since they imitate a distal selective peroneal nerve injury due to compression at the fibular head. Although the neurological history is useful (such as following a gluteal injection or gunshot wound), the examiner should search for signs of tibial nerve involvement. Common manifestations of sciatic nerve involvement that are inconsistent with a peroneal neuropathy at the fibular head include severe foot pain, absent or depressed ankle jerk, weak ankle inversion, and sensory loss in the sole.
How to treat peroneal neuropathy at the fibular neck?
In patients with a peroneal neuropathy at the fibular neck, measures that reduce pressure, such as extra cushioning while sleeping and avoidance of crossing the legs during the day, are usually sufficient to alleviate the symptoms. An ankle-foot orthosis splint to keep the foot dorsiflexed should be used until active movement has recovered. Physical therapy consisting of active and passive range-of-motion exercises, as well as walking, is an important conservative measure. Surgical decompression can be considered for patients who do not recover on their own with the aforementioned measures.
What is the name of the neuropathy that causes sensory disturbances in the dorsal foot and the anterior and?
Peroneal neuropathy gives rise to sensory disturbances over the dorsal foot and to the anterior and lateral lower leg.
What nerves are involved in ankle eversion?
The superficial peroneal nerve travels between the peroneus longus and brevis, the primary ankle evertors, and innervates both muscles. The peroneus tertius and extensor digitorum longus also contribute to ankle eversion. Segmental innervation is the same as for the deep peroneal nerve. Near to the midpoint of the lateral lower leg, the nerve becomes subcutaneous. It supplies sensation to the skin of the lateral leg and the dorsum of the foot and toes, sparing the small area between the first two toes and a variable lateral part of the foot [1]. Fifteen to twenty-eight percent of patients have an accessory peroneal nerve that branches off the superficial peroneal to supply the extensor digitorum brevis (usually innervated by the deep peroneal) [2–4].
What nerve is in the foot?
In the foot, the deep peroneal nerv e remains in close proximity to the interosseus membrane with the anterior tibial artery. The nerve supplies the short toe extensors, the extensor digitorum brevis, and extensor hallucis brevis. Also, it provides innervation to the intertarsal joints. Then, it terminates in a cutaneous branch. This branch innervates the web space between the first and second toes [1].
What causes a peroneal nerve to compromise?
Peroneal nerve compromise has been reported due to numerous traumatic and insidious causes. Traumatic causes of nerve injury occur in association with musculoskeletal injury or with isolated nerve traction, compression, or laceration. Insidious causes include mass lesions and metabolic syndromes.
How long does it take to diagnose a peroneal nerve injury?
If there has been an injury to the peroneal nerve at the knee during lateral ankle sprain, this could be detected within 2 weeks after injury on electromyographic examination. A series of 66 patients with ankle sprain underwent this evaluation. Eighty-six percent of patients with grade III sprains and seventeen percent of patients with grade II sprains had electrodiagnostic evidence of peroneal nerve injury on needle examination. Nerve conduction studies were normal in most patients with ankle sprain. Three of the patients (10%) with grade II injury had abnormal sensory studies, and one of the patients with grade III ankle sprain had abnormal motor studies [11].
Which nerve innervates the anterior muscles of the leg?
The deep peroneal nerve innervates the anterior muscles of the leg by traveling deep to the peroneus longus. This nerve supplies the tibialis anterior, extensor digitorum longus, peroneus tertius, and extensor hallucis longus. These muscles control foot dorsiflexion and toe extension.
What is the largest nerve in the sacral plexus?
The sacral plexus is formed from the L4–S4 ventral rami. The largest nerve in the sacral plexus and in the human body is the sciatic nerve. It receives contributions from the L4–S3 ventral rami and exits the sacral plexus by passing through the greater sciatic foramen and traveling inferior to the piriformis muscle.
Where does the peroneal nerve travel?
The common peroneal nerve then travels across the lateral head of the gastrocnemius muscle. This nerve provides cutaneous innervation to the lateral aspect of the leg below the knee via the lateral cutaneous nerve of the calf. Just distal to the head of the fibula, the nerve becomes subcutaneous. It continues between the peroneus longus muscle and the fibula. At this point, it divides into two main branches, the deep peroneal and superficial peroneal nerves.
What causes peroneal nerve injury?
The peroneal nerve can be injured by trauma and nerve compression, including:
What nerves are involved in the front of the feet?
The common peroneal nerve branches from the sciatic nerve and provides sensation to the front and sides of the legs and to the top of the feet. This nerve also controls the muscles in the leg that lift the ankle and toes upward. Injuries to the peroneal nerve can cause numbness, tingling, pain, weakness and a gait problem called foot drop.
What is the name of the disease that causes numbness in the shin?
Amyotrophic lateral sclerosis (also known as ALS or Lou Gehrig’s disease) Multiple sclerosis. Parkinson’s disease. Herniated lumbar disk. Peroneal Nerve Injury Symptoms. Inability to point the toes upward or lift the ankle up (dorsiflexion) Pain, weakness or numbness affecting the shin or the top of the foot. Loss of ability to move the foot.
What is the name of the gait where the knee is raised higher than normal to clear the foot from the ground?
A distinctive gait where the knee is raised higher than normal to clear the foot from the ground when the leg swings forward (also called steppage or foot drop gait)
What can help with mobility?
Nonsurgical treatments, including orthotics, braces or foot splints that fit inside the person’s shoe, can bring relief. Physical therapy and gait retraining can help the person improve their mobility. Some injuries may require peripheral nerve surgery, including one or more of these procedures: Decompression surgery.
What is nerve conduction?
Nerve conduction study, which measures the amount and speed of conduction of an electrical impulse through a nerve.
Which nerve innervates the muscles in the legs that lift the ankle and toes upward?
The branches of the common peroneal nerve innervate and control the muscles in the legs that lift the ankle and toes upward (dorsi flexion).
What nerve is entrapped in scar at the fibular head?from drrobertlaprademd.com
When the physical exam and/or studies document that the common peroneal nerve is entrapped in scar at the fibular head, a common peroneal nerv e neurolysis may be performed. This involves making an incision over the anterior compartment of the leg and upper portion of the biceps femoris, developing a skin flap down to the region ...
How successful is peroneal nerve decompression?from drrobertlaprademd.com
Treatment of common peroneal nerve entrapment can include rest and observation, but when this is not successful a common peroneal nerve decompression can be performed. As is true for most nerve decompression surgeries, the success rate is approximately 70% to 75% . The most common reasons for continued symptoms after surgery are ...
What happens if your knee opens up on the outside?from drrobertlaprademd.com
In addition, with posterolateral corner knee injuries, if the knee opens up significantly on the outside because of the posterolateral corner injury, the common peroneal nerve can become stretched as part of this injury and become irritated or damaged.
How many people have a peroneal nerve injury?from drrobertlaprademd.com
In our series, about 15% of people will have a common peroneal nerve injury when they do have a complete posterolateral corner injury. In these cases, about 50% of the time the common peroneal nerve function will be restored. Therefore, it is important to have the patient wear an ankle foot orthosis and to work daily on stretching exercises so the heel cord does not become significantly tight if they have had a foot drop develop after a posterolateral corner injury.
What is the best treatment for peroneal nerve palsy?from drrobertlaprademd.com
If a peroneal nerve palsy occurs due to a trauma, such as a sporting instrument hitting the outside of the leg, or after surgery where retraction or stretching the nerve may have inadvertently occurred, the use of oral corticosteroids may help to stabilize the nerve and help it to recover sooner.
How long does it take to recover from a peroneal nerve decompression?from drrobertlaprademd.com
The recovery time after a common peroneal nerve decompression at the knee is usually 3-4 months. For the first 6 weeks, we do not want to encourage the knee to form a lot of scar tissue around the area of the decompression, so we have patients on crutches.
What does tapping on the nerve in the foot mean?from drrobertlaprademd.com
Tapping on the nerve at this location, called a Tinel’s sign, may cause some zingers to go down the leg or cause numbness or weakness of the foot. Localized common peroneal nerve entrapment usually has these types of symptoms right at the location where the common peroneal nerve crosses the lateral aspect of the fibula.
What is class III evidence?
An evidence-based review conducted by the American Association of Neuromus-cular and Electrodiagnostic Medicine concluded that there was class III evidencesupporting the use of nerve conduction studies for the diagnosis of fibular neurop-athy, specifically motor nerve conductions of the fibular nerve recording from thetibialis anterior and extensor digitorum brevis muscles (including conductionthrough the leg and across the fibular head), and orthodromic and antidromic super-ficial fibular sensory nerve conduction studies.65 In addition, class III and IVevidence was found for its usefulness in providing information with regard torecovery of function, whereas evidence was limited to class IV for the role of needleelectromyography.65
What nerves are involved in motor innervation?
The deep fibular (peroneal) nerve supplies motor innervation to all anterior compartmentmuscles (the tibialis anterior, the extensor digitorum longus, and extensor hallucis lon-gus) and the fibularis tertius, also known as the peroneus tertius. The anterior tibialis isthe strongest foot dorsiflexor, although the extensor digitorum longus and the fibularistertius assist with this movement. The deep fibular nerve travels distally in the calf and atthe level of the ankle joint, fascia overlying the talus and the navicular bind the deepfibular nerve dorsally. Ventrally, the extensor hallucis longus muscle fibers and tendonand the inferior extensor retinaculum overlay the nerve. The inferior extensor retinac-ulum is a Y-shaped band anterior to the ankle; the anterior tarsal tunnel is consideredthe space located between the inferior extensor retinaculum and the fascia overlyingthe talus and navicular. Just rostral or under the inferior extensor retinaculum, thedeep fibular nerve branches into medial and lateral branches. The lateral branch ofthe deep fibular nerve travels under the extensor retinaculum, as well as the extensordigitorum and hallucis brevis muscles to innervate these muscles and nearby joints.The medial branch travels under the extensor hallucis brevis tendon to supply sensationto the skin between the first and second toes.
What muscle is most likely to be abnormal on a needle electromyographic examination?
Needle electromyographic examination should include the tibialis anterior muscle .This muscle is the most likely muscle to demonstrate abnormalities on the needleexamination.16The examination should also include at least one muscle innervatedby the superficial fibular nerve, the short head of the biceps femoris, and at leastone tibial innervated muscle distal to the knee. The short head of the biceps femoris,the only fibular-innervated muscle above the knee, is abnormal with a more proximalmononeuropathy involving the fibular division of the sciatic. Sciatic nerve lesions maymimic fibular neuropathies because of the fascicular arrangement of the nerve in thethigh.63,64The fibular nerve fibers in the thigh seem to be more susceptible to injurycompared with those of the tibia, and clinically only fibular nerve involvement maybe suspected. This susceptibility is thought to arise from several factors, includingthe fibular nerve’s more lateral location, the larger funiculi, or its tethering and coursearound the fibular head. Electrophysiologically, a sciatic neuropathy can be distin-guished by assessing tibial motor and sensory conduction, as well as evaluating foraxonal loss in tibial nerve innervated muscles, including those in the thigh. If a distaltibial innervated muscle is abnormal or if the short head of the biceps femoris isabnormal, then the examination should be extended to include more proximal sciaticinnervated muscles to exclude a sciatic neuropathy as well as an evaluation of glutealmuscles (abnormal in a lumbosacral plexopathy), and a lumbosacral paraspinal exam-ination to exclude a radiculopathy or polyradiculopathy. Deep fibular abnormalitiesmay be severe with common fibular neuropathy, with normal superficial sensoryresponses.
What is the most common neuropathy in the lower limb?
Fibular or peroneal neuropathy is the most frequent mononeuropathy encountered inthe lower limb and the third most common focal neuropathy encountered overall, aftermedian and ulnar neuropathies.1,2Following revised anatomic terminology publishedin 1998, the peroneal nerve is also now known as the fibular nerve, to prevent confu-sion of this nerve with those regions with similar names.3Perone is another term for thefibula and, thus, this revised terminology for this nerve, its branches, and relatedmusculature is based on language describing the location.3While both fibular andperoneal are considered acceptable terms, “fibular” and it related terminology ispreferred and therefore will be used throughout this article.
Can fibular neuropathy cause foot drop?
Patients with fibular neuropathy often present with complaints of “foot drop” orcatching their toe with ambulation, which may develop acutely or subacutely depend-ing on the precipitating cause. There may also be complaints of sensory loss over thefoot dorsum.
