
Common Causes
Dyspnea is an uncomfortable abnormal awareness of breathing. Dyspnea is the most common cause of respiratory limitation of activity in patients with pulmonary disease. Dyspnea is a subjective symptom reported by patients.
Related Conditions
When you have shortness of breath, you can’t catch your breath or get enough air in your lungs. Your doctor might call it dyspnea. It can be a warning sign of a health problem that needs treatment right away. If you're a healthy adult, you breathe in and out up to 20 times a minute. That's nearly 30,000 breaths a day.
What is dyspnea in pulmonary disease?
If dyspnea occurs suddenly or if symptoms are severe, it may be a sign of a serious medical condition. An episode of dyspnea is not always directly related to an individual’s health. A person can feel short of breath after intense exercise, when traveling to a high altitude, or going through major temperature changes.
What is shortness of breath (dyspnea)?
Some causes of unexplained dyspnea are due to structural abnormalities including blood clots, structural heart disease, valvular heart disease, structural lung disease and abnormalities due to congenital heart and lung disease that could be treated with surgery.
Is dyspnea a sign of a serious medical condition?
What are the causes of unexplained dyspnea?

What is the most common cause of dyspnea?
According to Dr. Steven Wahls, the most common causes of dyspnea are asthma, heart failure, chronic obstructive pulmonary disease (COPD), interstitial lung disease, pneumonia, and psychogenic problems that are usually linked to anxiety. If shortness of breath starts suddenly, it is called an acute case of dyspnea.
What is dyspnea in the respiratory system?
Dyspnea is a sensation of running out of the air and of not being able to breathe fast enough or deeply enough. It results from multiple interactions of signals and receptors in the CNS, peripheral receptors chemoreceptors, and mechanoreceptors in the upper airway, lungs, and chest wall.
What are 3 causes of dyspnea?
The most common causes of short-term dyspnea are:Anxiety disorders.Asthma.A blood clot in your lungs, known as pulmonary embolism.Broken ribs.Excess fluid around your heart.Choking.A collapsed lung.Heart attacks.More items...•
Is dyspnea a serious condition?
Dyspnea can range from mild to severe. If this condition is chronic and persistent, it may seriously limit activity and reduce quality of life. Dyspnea can be a result of lung, heart, vascular, neuromuscular and metabolic disease.
What are the signs of dyspnea?
What are the symptoms of dyspnea?heart palpitations.weight loss.crackling in the lungs.wheezing.night sweats.swollen feet and ankles.labored breathing when lying flat.high fever.More items...
What happens to the body during dyspnea?
Dyspnea can cause you to feel a constriction in the chest. This tightness can make you feel that you can't get a deep breath and can lead to a smothering sensation. This sensation is sometimes described as air hunger. Some people say they feel that they have to work very hard to take a breath.
How is dyspnea diagnosed?
The most useful methods of evaluating dyspnea are the electrocardiogram and chest radiographs. These initial modalities are inexpensive, safe and easily accomplished. They can help confirm or exclude many common diagnoses.
What is the difference between shortness of breath and dyspnea?
Shortness of breath — known medically as dyspnea — is often described as an intense tightening in the chest, air hunger, difficulty breathing, breathlessness or a feeling of suffocation. Very strenuous exercise, extreme temperatures, obesity and higher altitude all can cause shortness of breath in a healthy person.
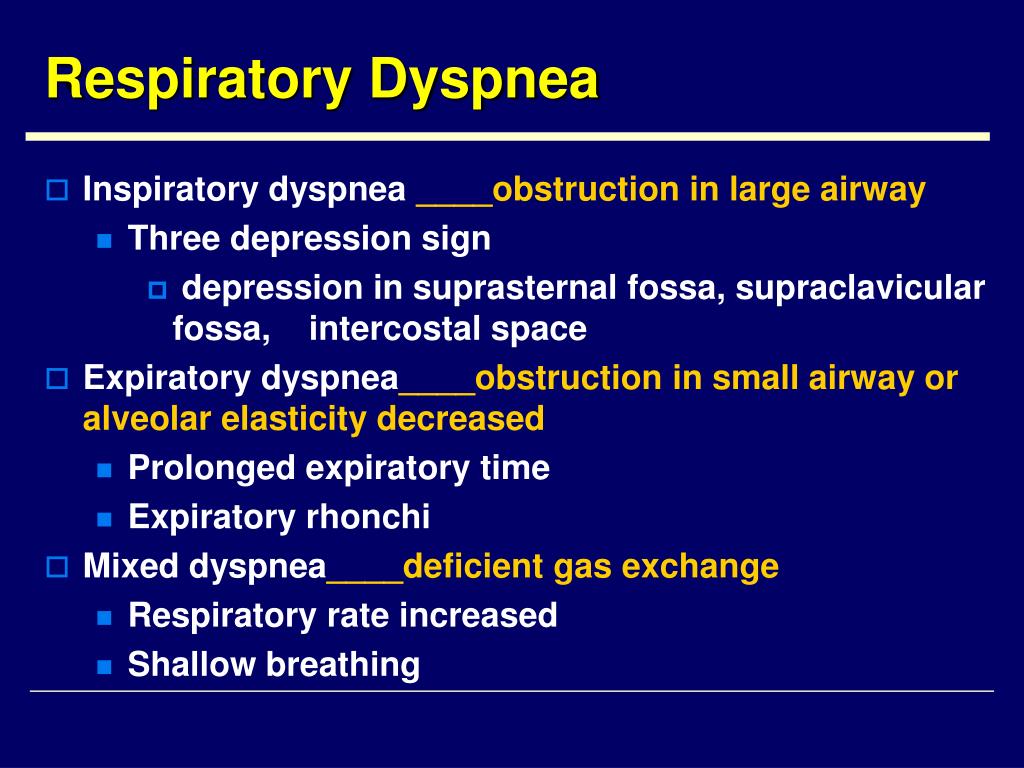
What are the types of dyspnea?
it has arisen from four primary categories: respiratory, cardiac, neuromuscular, psychogenic, systemic illness, or a combination of these.
Is dyspnea a disability?
The SSA will consider your respiratory disorder symptoms, such as whether you suffer from shortness of breath, whether your lungs function normally, whether you suffer from chest pain, or whether you experience bloody sputum when you cough. However, symptoms alone will not result in an approval for disability.
How long does acute dyspnea last?
Feeling breathless may be acute, lasting just a few days or less. Other times, it is chronic, lasting longer than three to six months.
How do hospitals treat shortness of breath?
Standard treatments for respiratory distress include oxygen, albuterol nebulization (with or without ipratropium), nitroglycerin, Lasix, morphine and continuous positive airway pressure (CPAP) or endotracheal (ET) intubation, depending on the presumed cause of distress.
What causes dyspnea?
Steven Wahls, the most common causes of dyspnea are asthma, heart failure, chronic obstructive pulmonary disease (COPD), interstitial lung disease, pneumonia, and psychogenic problems that are usually linked to anxiety.
What are the symptoms of dyspnea?
Emergency medical treatment is needed if an individual has any of these symptoms: sudden onset of severe dys pnea. loss of ability to function due to shortness of breath. chest pain. nausea. Not all cases of dyspnea call for immediate medical treatment, but shortness of breath can indicate serious medical problems.
How do you know if you have dyspnea?
Signs that a person is experiencing dyspnea include: shortness of breath after exertion or due to a medical condition. feeling smothered. Trusted Source. or suffocated as a result of breathing difficulties. labored breathing. tightness in the chest. rapid, shallow breathing.
What is the medical term for shortness of breath?
Dyspnea is the medical term for shortness of breath, sometimes described as “air hunger.”. It is an uncomfortable feeling. Shortness of breath can range from mild and temporary to serious and long-lasting. It is sometimes difficult to diagnose and treat dyspnea because there can be many different causes.
What is the Dyspnea Lab?
The Dyspnea Lab, a research center specializing in shortness of breath, report that people find these programs helpful, even if the root causes of the problem remains. If tests indicate low levels of oxygen in the blood, supplemental oxygen may be supplied.
What causes shortness of breath in infants?
Diseases of the upper respiratory system that cause acute dysnpea are a relatively common pediatric emergency. They are one of the most common causes of shortness of breath in infants. Croup, inhaling a foreign object, and inflammation of the epiglottis are all common causes of dyspnea in infants.
Why is it so hard to breathe with dyspnea?
Environmental pollutants such as chemicals, fumes, dust, and smoke can make it more difficult for people with dyspnea to breathe. People with asthma may find that exposure to allergens such as pollen or mold may trigger episodes of dyspnea.
What Is Dyspnea?
Your doctor might call it dyspnea. It can be a warning sign of a health problem that needs treatment right away.
How to treat shortness of breath from dyspnea?
Breathing and relaxation methods may help. But your dyspnea treatment will depend on what's causing your shortness of breath. For example, if you have asthma, you may get an inhaler to use when you have a flare. If there’s fluid in your lungs, the doctor might need to drain it. If an infection or a blood clot is making you feel short of breath, you could need medication. You also might get oxygen. If you take medications, always take them as your doctor prescribes.
What does a chest X-ray show?
Chest X-ray or a CT scan. They can see if you have pneumonia, a blood clot in your lung, or other lung diseases. A CT scan puts together several X-rays taken from different angles to make a complete picture.
What to do if you have shortness of breath?
If you have new shortness of breath, call 911 . If you have another health condition that makes you more likely to get seriously ill, and you have a fever or cough, call your doctor to ask whether you might have COVID-19, the illness caused by the new coronavirus.
What test is used to determine how much air can be blown in and out of the lungs?
The doctor will examine you and listen carefully to your lungs. You might have a lung function test, called spirometry, to measure how much air you can blow in and out of your lungs and how fast you do it. This can help diagnose asthma and COPD.
What does it mean when you can't breathe?
Hungry for air (you might hear this called air hunger) Unable to breathe deeply. Like you can’t breathe (suffocation ) It can be acute (sudden dyspnea) or chronic (long-lasting dyspnea). Acute dyspnea starts within a few minutes or hours. It can happen with other symptoms like a fever, rash, or cough.
How many times do you breathe in and out a minute?
If you're a healthy adult, you breathe in and out up to 20 times a minute. That's nearly 30,000 breaths a day. A hard workout or the common cold might throw a kink in that pattern from time to time, but you should almost never feel short of breath. If you have new shortness of breath, call 911.
What are the causes of dyspnea/shortness of breath?
Dyspnea can be caused by many conditions, some more serious than others, including:
How to diagnose dyspnea?
In those patients who have unexplained dyspnea, the most accurate way to make a diagnosis is through advanced cardiopulmonary exercise testing. This test uses catheters during exercise (stationary cycling or treadmill) to assess how the body is utilizing oxygen, and to measure heart and lung function.
What are risk factors for dyspnea?
Shortness of breath is a normal symptom during intense exercise or exertion. If it occurs while the patient is at rest—or during unexpected situations—it can be a symptom of a serious medical condition. If you suffer from dyspnea, you may also have any of these health issues:
What medication is used to treat dyspnea/shortness of breath?
Your doctor may prescribe one of the following medications, depending on the underlying cause of the dyspnea:
How can patients manage dyspnea/shortness of breath?
You can help manage shortness of breath with relaxation and breathing exercises. Be sure to talk with your doctor before trying these techniques.
What is the Dyspnea Center?
Dyspnea patients benefit from the Dyspnea Center's clinical team and the wide range of specialists at The Lung Center and Heart & Vascular Center, including pulmonary and critical care medicine, thoracic surgery, cardiovascular medicine, neurology and thoracic and cardiovascular imaging. This collaboration ensures world-class, comprehensive care for dyspnea — as well as its underlying causes.
How to treat dyspnea?
Dyspnea is treated by addressing the underlying disease or condition. For example, if dyspnea is caused by pleural effusion, draining fluid from inside the chest can reduce shortness of breath. Depending upon the cause, dyspnea can sometimes be treated with medication or by surgical intervention.
What is the definition of dyspnea?
Despite its prevalence, the descriptions of dyspnea vary from patient to patient and no single definition encompasses all its qualitative aspects. Typically, it is defined as a feeling of shortness of breath or an inability to take a deep breath.
What causes dyspnea in the lungs?
Diseases such as pulmonary fibrosis affect the alveolar membrane as well as lung compliance, causing dyspnea through impairment of gas exchange and increased work of breathing to expand stiff lung tissue. 2 Chronic obstructive pulmonary disease (COPD) and asthma are examples of diseases that primarily affect conduction of air through the airways, leading to dyspnea through increased work of breathing. 3 These diseases of airflow obstruction also lead to air trapping and hyperinflation of the lungs, altering respiratory mechanics and further increasing the work of breathing. 4 Deconditioning and neuromuscular diseases often involve an overlap of the mechanisms described above. For instance, in amyotrophic lateral sclerosis, the respiratory muscles become weak, which results in impaired ventilation due to failure of the respiratory pump. In obesity, the pump itself may require more energy to move air in and out, and yet still be unable to meet the demands of the body due to general deconditioning. The nervous system can be impaired by many disease states or sometimes by medications, leading to decreased respiratory drive or action, or even central apnea. The central nervous system also detects changes in body pH, which can be a powerful stimulus for a patient's dyspnea, even if the acidemia is not related to a respiratory abnormality. 5
How does lifestyle change affect dyspnea?
Lifestyle modifications can affect dyspnea significantly in some cases, such as weight loss for those with dyspnea related to obesity hypoventilation and sleep apnea, or smoking cessation for those with smoking related disease. Surgical techniques, such as lung volume reduction surgery, are useful in a highly selected subset of patients and should be reserved for those cases where they are recommended by specialists. 19
What are the mechanisms of dyspnea?
The mechanisms and pathophysiology of dyspnea involve interactions between the respiratory system (both the ventilatory function and gas exchange function), the cardiovascular system, neural responses, and oxygen carriers. A broad classification is key to realizing all important causes when faced with a dyspneic patient (Table 1).
How to help with dyspnea?
Despite the availability of devices, the most common initial treatment offered is supplemental oxygen delivery . Increasing the fraction of inspired oxygen may alleviate the sensation of inadequate breathing, resulting in relief of dyspnea. 15 Supplemental oxygen also helps reverse the systemic consequences of hypoxia such as anaerobic metabolism and pulmonary hypertension. Adding helium to the inspired gas mixture can reduce the work of breathing in obstructive lung diseases due to the density and laminar flow properties of helium. 16,17
What organs cause dyspnea?
Diseases in other organs, such as the kidneys and the liver, may cause dyspnea by a combination of the interactions we have discussed. In end stage renal disease, for example, dyspnea can be due to metabolic acidosis, volume overload causing pulmonary edema, and/or pleural effusions impairing lung expansion.
How does respiratory capacity change during pregnancy?
During pregnancy the respiratory system undergoes important and predictable changes. The functional residual capacity of the lungs declines by 18% to 20% as does the residual volume. The tidal volume of resting breaths increases by about 0.2 L, and the volume of air exchanged in each minute increases by about 40%. These factors must be taken into account when assessing a pregnant woman with dyspnea, which is a common but usually mild symptom. Importantly during pregnancy, the respiratory rate typically does not change. 20,21
Why is dyspnea a challenge?
The diagnostic assessment of dyspnea is a challenge in routine practice, particularly because the term “dyspnea”/“shortness of breath” covers a variety of subjective experiences.
What is dyspnea subjective experience?
Dyspnea is an umbrella term for a number of distinguishable subjective experiences including effortful respiration , a feeling of choking or asphyxiation, and hunger for air. The subjectivity of dyspnea is one of the main difficulties confronting the clinician whose task it is to determine the diagnosis and judge the severity of the underlying condition. The pathogenesis of dyspnea is still not fully clear and is now under investigation. Current explanatory hypotheses are based on the concept of a regulatory circuit that consists of afferent information relayed centrally (from chemoreceptors for pH, CO2, and O2 , as well as from mechanoreceptors in the musculature and the lungs [C fibers in the parenchyma, J fibers in the bronchi and pulmonary vessels]) and a corresponding ventilatory response (2).
What are the instruments used to assess dyspnea?
Various instruments are used to assess dyspnea, ranging from simple descriptions of intensity (visual analog scale, Borg scale) to multidimensional questionnaires (e.g., the Multidimensional Dyspnea Profile). These instruments have been validated and are useful for communication. There are other, disease-specific classifications, including the New York Heart Association (NYHA) classification of chronic congestive heart failure (2, 3).
How many patients have shortness of breath?
Dyspnea (shortness of breath) is a common symptom affecting as many as 25% of patients seen in the ambulatory setting.
What is shortness of breath?
Dyspnea (shortness of breath) is a common symptom affecting as many as 25% of patients seen in the ambulatory setting. It can be caused by many different underlying conditions, some of which arise acutely and can be life-threatening (e.g., pulmonary embolism, acute myocardial infarction). Thus, rapid evaluation and targeted diagnostic studies are of central importance. Overlapping clinical presentations and comorbid diseases, e.g., congestive heart failure and chronic obstructive pulmonary disease (copd), can make the diagnostic evaluation of dyspnea a clinical challenge, all the more so as the term “dyspnea” covers a wide variety of subjective experiences. The presence of this symptom is already a predictor of increased mortality.
Is dyspnea a life threatening condition?
Dyspnea is a common symptom affecting as many as 25% of patients seen in the ambulatory setting. It can arise from many different underlying conditions and is sometimes a manifestation of a life-threatening disease.
What is dyspnea?
Patients with dyspnea often describe tightness of the chest and a smothering sensation. These feelings can cause anxiety and psychological distress that makes symptoms worse, creating a vicious cycle.
What causes dyspnea?
Diseases such as amyotrophic lateral sclerosis and myasthenia gravis can cause general bodily weakness that can lead to dyspnea. Another cause is general physical deconditioning, in which the body weakens from inactivity. Deconditioning can result from surgery or serious illness, or it can come from poor lifestyle choices.
What is the medical term for shortness of breath?
Dyspnea is the medical term for shortness of breath. Patients with dyspnea often describe tightness of the chest and a smothering sensation. These feelings can cause anxiety and psychological distress that makes symptoms worse, creating a vicious cycle.
What is it called when you are unaware of breathing?
Dyspnea has been described as an abnormal awareness of breathing. Humans are mostly unaware of the breathing process that keeps them alive. For that reason, being conscious of breathing is an uncomfortable experience that can cause anxiety.
How to improve dyspnea?
Lifestyle changes can improve dyspnea. Losing weight can be especially effective, as obesity increases the risk of asthma and other breathing problems. Being overweight can also cause joint pain and other conditions that make moving difficult, leading to deconditioning.
How to tell if you have dyspnea?
If you seek medical help for dyspnea, your doctor will examine your lungs by listening for breath sounds such as wheezes and crackles. Fingers with widened tips, a condition known as clubbing, can also be a sign of respiratory problems. Tests such as chest X-ray and bronchoscopy can give your doctor more information.
Can dyspnea be caused by low oxygen levels?
In many cases, dyspnea is not caused by low oxygen saturation in the blood. It's possible to have dyspnea with normal blood oxygen levels.
What does it mean when you have dyspnea?
Kathrin Ziegler/Getty Images. Dyspnea on exertion means that a person feels short of breath during exercise. It can cause someone to feel as though they are running out of air and cannot breathe fast or deep enough while exercising or exerting physical effort. Dyspnea on exertion can also cause:
What causes dyspnea when exerting?
Respiratory conditions are a common cause of dyspnea on exertion. Common respiratory causes include:
How to treat dyspnea from smoking?
The treatment for dyspnea on exertion that occurs due to chemical or environmental irritants depends on the specific cause, but common options include: stopping smoking or avoiding exposure to tobacco smoke. wearing protective covering and breathing devices when exposed to chemical fumes.
What is the best treatment for dyspnea?
Common treatment options for respiratory causes include: inhalers, such as antimuscarinics, corticosteroids, and short- or long-acting bronchodilator inhalers. supplemental oxygen therapy.
When to consult a doctor for dyspnea?
It is important to consult a doctor when dyspnea during exertion is unexplained, sudden, severe, or disabling, or if one of the more serious symptoms listed above accompanies it. Last medically reviewed on February 26, 2021. Asthma. Lung Cancer.
Which system plays a role in respiration?
As the cardiovascular system plays a role in respiration, several cardiac conditions are associated with dyspnea on exertion. These include:
Can dyspnea cause tight chest?
Depending on the cause, dyspnea can occur alongside other symptoms, such as a tight chest and anxiety. Read on to learn more about dyspnea on exertion, including the possible causes and when to see a doctor.
Pathophysiology
Uncomfortable sensation or awareness of breathing or needing to breathe.
Signs and Symptoms
Diagnostic Testing
Treatment
- The mechanisms and pathophysiology of dyspnea involve interactions between the respiratory system (both the ventilatory function and gas exchange function), the cardiovascular system, neural responses, and oxygen carriers. A broad classification is key to realizing all important causes when faced with a dyspneic patient (Table 1). The respiratory s...
Considerations in Special Populations
- An exhaustive list of signs and symptoms is beyond the scope of this discussion although these often provide clues to the underlying organ system involved. In many respiratory disorders cough may be a common symptom, alerting to airway inflammation or irritation. Presence of fever may often point towards an infectious disease also contributing to dyspnea. Patients may misinterpr…
Conclusion
- The most commonly employed initial test is the chest roentgenogram. A well performed posteroanterior and lateral view chest roentgenogram can be invaluable in the evaluation of dyspnea. Although primarily targeted at the lungs, it also helps in an evaluation of the cardiovascular system, the chest wall, pleura, mediastinum and upper abdomen. Advanced mod…