Failure to capture means that the ventricles fail to response to the pacemaker impulse. On an EKG tracing, the pacemaker spike will appear but it will not be followed by a QRS complex. Failure to pace occurs when the pacemaker does not generate an electrical impulse. On an EKG tracing, pacemaker spikes will be missing.
What causes a pacemaker to fail to capture?
Capture failure occurs when the generated pacing stimulus does not initiate myocardial depolarization. The main causes of this failure are lead dislodgment, low output, lead maturation, and lead or pacer failure (fibrosis, fracture, low pacing voltage, or elevated myocardial pacing thresholds).
What is failure to sense in a pacemaker?
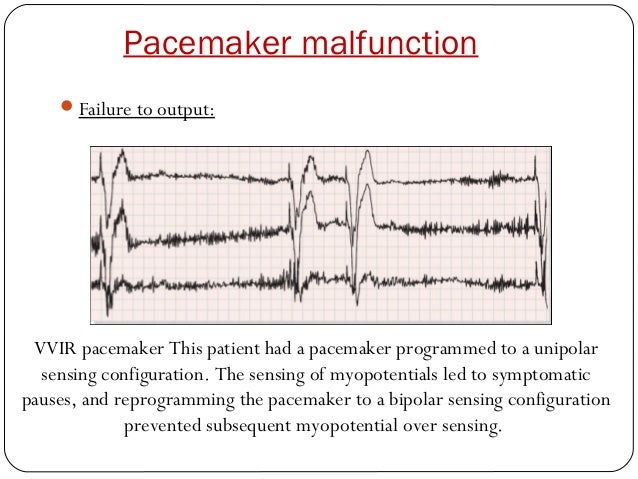
Failure to sense occurs when the pacemaker does not detect the patient's myocardial depolarization. This can often be seen on an EKG tracing as a spike following a QRS complex too early. This can often be seen on an EKG tracing as a spike following a QRS complex too early.
How often do pacemakers fail?
Pacemakers very rarely fail. So no worries there. The problem area is the leads. They do have a life of around 25 to 35 years if you are lucky. They dont suddenly fail but give indications of degradation giving plenty of time to find a resoultion to any problem. Dont worry.
Is it possible to have malfunctioning pacemaker?
You can tell if your pacemaker is malfunctioning if you are starting to experience symptoms of arrhythmia. You might have chest pain, difficulty breathing, dizziness, or lightheadedness. There are several reasons why your pacemaker might stop working. These include the following: Your condition has changed and it needs to be reprogrammed.
What does it mean when a pacemaker fails to capture?
Failure to capture (FTC), which means that the pacemaker stimulations do not result in myocardial activation. Failure to pace (FTP), which means that the pacemaker does not stimulate as expected. Oversensing, which means that the pacemaker senses signals that are not true P-waves or R-waves.
How do I know if my pacemaker is not capturing?
You can tell if your pacemaker is malfunctioning if you are starting to experience symptoms of arrhythmia. You might have chest pain, difficulty breathing, dizziness, or lightheadedness. There are several reasons why your pacemaker might stop working.
What causes failure to capture?
Failure to capture can result from several causes, including battery depletion, circuit failure, lead dislodgement or maturation, elevated capture thresholds due to progressive cardiac disease, metabolic abnormalities and or drugs.
How do you troubleshoot failure to catch a pacemaker?
Failure to capture• If the patient's condition has changed, notify the health care provider (HCP) and ask for new settings. If pacemaker settings have been altered by the patient or someone else, return them to their correct positions. If the pacemaker generator has a plastic face cover, make sure it's in place.
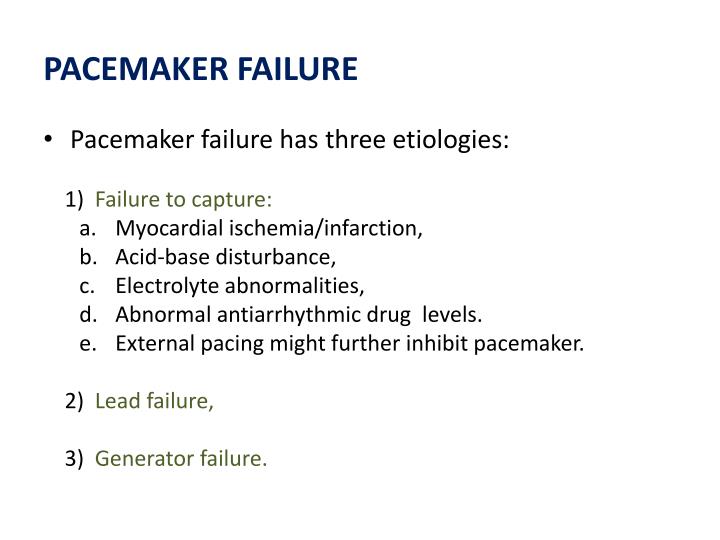
What are the 3 primary problems that can occur with a pacemaker?
Pacemaker failure has three causes: (1) failure of capture, (2) lead failure, and (3) generator failure. Failure of capture owing to a defect at the level of the myocardium (i.e., the generator continues to fire but no myocardial depolarization takes place) remains the most difficult problem to treat.
What are the 4 common issues with pacemakers?
Problems with the pacemaker the lead gets pulled out of position. the battery of the pulse generator fails. the circuits that control the pacemaker are damaged after being exposed to strong magnetic fields. the pacemaker has not been properly programmed.
What is the most common pacemaker malfunction?
Most common are the rate-related pseudomalfunctions. Rate changes in the presence of normal pacemaker function can occur because of magnet operation, timing variations (A-A vs V-V), upper-rate behavior (Wenckebach or 2:1 block), pacemaker-mediated tachycardia (PMT), or rate response.
How often does a pacemaker malfunction?
Maisel reported a pacemaker generator failure rate of 0.46% based on US Food and Drug Administration reports, as well as 1.3 malfunctions per 1000 person-years based on device registries.
What is capture in cardiac pacing?
Electrical capture is assessed by inspection of the ECG tracing on the pacing unit monitor. Successful capture is usually characterized by a widened QRS complex, followed by a distinct ST segment and broad T wave (Figure 2).
What will the nurse do first if the patient's pacemaker fails to capture?
Failure to capture: Pacemaker fires but does not depolarize the ventricle. The nurse should turn patient to left side (to bring lead in better contact with endocardium), check all connections, and increase the energy delivered.
How can you tell if a pacemaker is working?
A pacemaker check is typically performed every six weeks after the device is implanted. The checkup will help your doctor determine if the pacemaker is working properly. A magnet will be placed over your pacemaker to change its rate of function. An external computer will analyze the rate of change.
What does failure to capture look like on EKG?
Capture Failure. Capture failure occurs when the generated pacing stimulus does not initiate myocardial depolarization. On the surface ECG, pacing spikes are present, but they are not followed by a QRS complex in the event of ventricular noncapture or by the lack of P waves in the event of atrial noncapture (Fig.
How easy is it to dislodge pacemaker leads?
Abstract. The rate of dislodgement of atrial pacing leads is ∼3%. To solve this problem, reoperation and repositioning of these leads is one of the solutions.
How do you know you have capture with pacing?
Electrical capture is assessed by inspection of the ECG tracing on the pacing unit monitor. Successful capture is usually characterized by a widened QRS complex, followed by a distinct ST segment and broad T wave (Figure 2).
What causes a pacing threshold to increase?
Hyperpolarization of the myocardial cell membrane can occur with alkalosis or hypocarbia leading to an increase in the pacing threshold, as will hypokalemia, which may result from hyperventilation. Hyperglycemia will also raise the threshold, as will hypothermia, and may cause failure of the pacemaker to capture. C.
How to test a pacemaker for failure to pace?
Standard ring magnets are typically used for this procedure. Some pacemakers may require specific magnets. Place the magnet directly on the chest wall over the pacemaker. This closes the reed switch and converts the pacemaker to an asynchronous or fixed‐rate pacing mode. Expect the pacemaker to pace at the programmed rate (60–80 beats/min). If this occurs, then the problem was oversensing and the pacemaker was inappropriately inhibited. Causes of oversensing include atrial depolarizations, muscle activity, and external electrical interference. Component failure should be suspected if there are no spikes on magnet application. Battery depletion is indicated by the presence of a pacemaker rate less than the program med rate. All of these conditions require further evaluation by cardiology. The magnet should be left in place if it corrects the underlying bradydysrhythmia.
What are polymorphic VTs?
Polymorphic VTs are related to electrical instability caused by an initial prolongation and then slow adaptation of repolarization caused by changes in the heart rate and activation sequence. Most polymorphic VTs, VF, and torsades de pointes that have been reported seem to be consistent with a pause or bradycardia-dependent mechanism. Anomalous dynamics of the paced QT intervals have been observed until the second day after AV junction ablation in patients with rapid refractory AF, resulting in prolongation of the QT interval when the heart rate is less than 75 beats/min. This finding may explain the ventricular arrhythmias occurring after AV junction ablation and may also explain the beneficial effects of temporary relatively rapid pacing. On the other hand, bradycardia may not be the sole factor. Sympathetic tone augmentation following AV junction ablation has been described in patients paced at 60 beats/min, thus causing prolongation of action potential duration and RV refractoriness, whereas sympathetic tone was reduced in patients paced at 90 beats/min. Such an increase in sympathetic activity and prolongation in action potential duration may favor early afterdepolarization and triggered activity, which may mediate torsades de pointes and polymorphic VT. To reduce the risk of these arrhythmias, routine pacing at 80 beats/min has been recommended following AV junction ablation. Patients with high-risk factors for arrhythmias, such as congestive heart failure or impaired LV function, may require pacing at higher rates (e.g., at 90 beats/min for 1 to 3 months) as well as in-hospital monitoring for at least 48 hours. Adjustment of the pacing rate, although rarely to less than 70 beats/min, is usually undertaken after 1 week in most patients, preferably after an ECG evaluation for repolarization abnormalities at the lower rate.
How fast does an escape rhythm develop after RF ablation?
Most patients who undergo RF ablation of the AV junction are pacemaker dependent after the procedure, as defined by lack of an escape rhythm that is faster than 40 beats/min. Following AV junction ablation, an escape rhythm develops in 70% to 100% of cases, and the absence of escape rhythm immediately after ablation seems to be the only predictor for long-term pacemaker dependency. Although the appearance of an escape rhythm does not obviate the need for pacing, it may provide reassurance in case of pacemaker failure.
How does a Zener diode protect the pacing output circuitry?
Current devices incorporate elements (Zener diodes, thyristors) that protect the pacing output circuitry and sensing amplifiers by shunting excess energy away from the device. The Zener diode behaves as a short circuit as soon as the voltage exceeds a certain value, such as 10 to 15 V, that is substantially above the output voltage of the pulse generator. Other, less common circuit designs can also limit the current flowing up the lead, but at the expense of inhibition of pacing output during the reception of large voltages. 22 For example, in the Telectronics (St. Jude Medical, Sylmar, Calif.) Meta DDDR 1254 pacemaker, the output circuit switches open to protect the generator if RF current is applied at the same time as the pacing pulse. No pacing output is emitted until the RF energy delivery ceases, although the event markers indicate normal pulse delivery. This behavior results in asystole during RF catheter ablation 23 or application of electrosurgery despite the use of a magnet or reprogramming to the VOO mode. 24
What causes a pacemaker to fail?
Pacemaker failure has three causes: (1) failure of capture, (2) lead failure, and (3) generator failure. Failure of capture owing to a defect at the level of the myocardium (i.e., the generator continues to fire but no myocardial depolarization takes place) remains the most difficult problem to treat. Myocardial changes that result in noncapture include myocardial ischemia/infarction, acid-base disturbance, electrolyte abnormalities, or abnormal levels of antiarrhythmic drug (s). Temporary pacing (transvenous, transcutaneous, transthoracic, or transesophageal) might inhibit pacemaker output at voltages that will not produce myocardial capture. Sympathomimetic drugs generally lower pacing threshold. Outright generator or lead failure is rare.
Why are cardiac pacemakers implanted under the skin?
Patients with implantable cardiac pacemakers and cardioverter-defibrillators are at much lower risk from stray current leaks than patients with central lines or external wires in place, because these devices are implanted under the skin, which leaves the normal protective mechanism of the skin intact.
What does PVARP mean?
Recall from the previous discussion that PVARP, mode switch and upper pacing limit are means for preventing these tachyarrhythmias. PVARP means that the atrial lead is refractory for a certain time period after each ventricular stimulation. Mode switch means that the pacemaker inactivates the trigger function during supraventricular tachyarrhythmias. Also note that tachyarrhythmias mediated by the pacemaker can not exceed the upper pacing limit of the pacemaker, which is usually set to 160 beats/min.
Why does my pacemaker undersensing occur?
Undersensing occurs when the pacemaker fails to detect cardiac activity. This may be due to lead dislodgement, lead fracture or inadequate myocardial contact. It may also be due to the low amplitude (voltage) of the potentials generated by activated myocardium.
What are the different types of pacemakers?
Conventional surface ECG can reveal the following types of pacemaker dysfunction: 1 Failure to capture (FTC), which means that the pacemaker stimulations do not result in myocardial activation. 2 Failure to pace (FTP), which means that the pacemaker does not stimulate as expected. 3 Oversensing, which means that the pacemaker senses signals that are not true P-waves or R-waves. Sensing of such signals normally inhibits the pacemaker. Oversensing may lead to underpacing. 4 Failure to sense (undersensing), which means that it fails to sense true P-waves or R-waves. Undersensing may lead to overpacing. 5 Failure to rate adjust, which means that the pacemaker fails to adjust its rate according to haemodynamic needs. This is only relevant in rate responsive pacemakers.
What does it mean when a pacemaker is undersensing?
Oversensing may lead to underpacing. Failure to sense (undersensing), which means that it fails to sense true P-waves or R-waves. Undersensing may lead to overpacing. Failure to rate adjust, which means that the pacemaker fails to adjust its rate according to haemodynamic needs.
Why does undersensing lead to overpacing?
Undersensing can lead to overpacing, because the pacemaker does not sense ongoing activity. Signs of overpacing should always lead to suspicion of undersensing.
Why is myocardial excitability not activated?
A stimulus delivered during the refractory period should not result in activation because the myocardium is refractory. The most common cause of failure to capture is insufficient stimulus energy. Modern pacemakers have built-in functions to calibrate the stimulus amplitude and width according to myocardial excitability.
What is the term for oversensing a pacemaker?
This type of oversensing is referred to as pacemaker crosstalk.
What does a spike on a pacemaker mean?
Y Clinical Tip: A pacemaker spike — a mark on the ECG projecting upward or downward from the baseline — indicates that the pacemaker has fired.
Why does my pacemaker fire?
The pacemaker fires because it fails to detect the heart's intrinsic beats, resulting in abnormal complexes. The cause may be a dead battery, decrease of P wave or QRS voltage, or damage to a pacing lead wire.
