
What is fi02 on a ventilator?
What is FiO2 ventilator? FiO2 is the amount of oxygen invested in the ventilator itself to pump your patient’s lungs up with air. Normal FiO2 is between 35% to 50%. However, in the events that your patient is not compensating and is not receiving the desired amount of oxygen, the FiO2 can be increased to 75% and as much as 100%.
What is the normal range of FiO2?
What is the normal range for PaO2 FiO2?
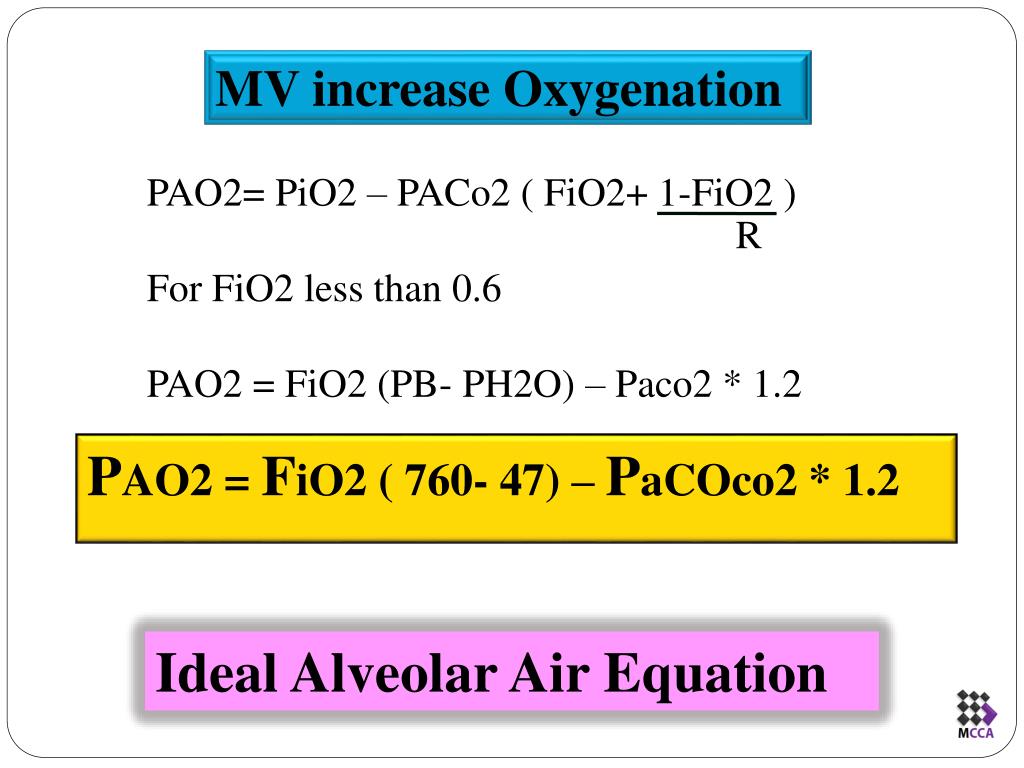
- The PaO2 rises with increasing FiO2. Inadequate or decreased oxygen exchange decreases the ratio.
- Normal PaO2/FiO2 is >400 mmHg.
- Approximate PaO2 by multiplying FiO2 by 5 (eg, FiO2 = 21%, then PaO2 = 100 mmHg)
What does FiO2 stand for?
What Does FiO2 Stand For? What Does FiO2 Stand For? FiO2 stands for Fraction of Inspired Oxygen; it is a fraction of the amount of oxygen a patient is inhaling produced by an oxygen device such as a nasal cannula or mask. Different devices deliver different amounts of oxygen to the patient.
What is FiO2 in mechanical ventilation?
What is FiO2 in mechanical ventilation? FiO2 : Percentage of oxygen in the air mixture that is delivered to the patient. Flow: Speed in liters per minute at which the ventilator delivers breaths.
What is a good FiO2 level?
FIO2 is typically maintained below 0.5 even with mechanical ventilation, to avoid oxygen toxicity, but there are applications when up to 100% is routinely used. Often used in medicine, the FIO2 is used to represent the percentage of oxygen participating in gas-exchange.
What is the meaning of FiO2?
fraction of inspired oxygenThe fraction of inspired oxygen (FiO2) is the concentration of oxygen in the gas mixture. The gas mixture at room air has a fraction of inspired oxygen of 21%, meaning that the concentration of oxygen at room air is 21%.
What is PEEP and FiO2?
Positive end-expiratory pressure (PEEP) and inspired oxygen fraction (FIO2) are the primary means of improving PaO2 during mechanical ventilation. Patients with acute respiratory distress syndrome (ARDS) typically present with a large intrapulmonary shunt, which makes even high FIO2 ineffective in improving PaO2.
What is the lowest FiO2 on ventilator?
The lowest FiO2 possible (50% or less) should be used to achieve the desired PaO2 to avoid oxygen toxicity.
What does FiO2 of 100 mean?
The flow meter is connected to either a bottle of oxygen or a medical wall supply of oxygen. This oxygen is PURE, it is 100% oxygen! Therefore, anything that comes out of that flow meter has an FiO2 of 100%.
What is the FiO2 of room air?
21 percent oxygenAs mentioned, room air is 21 percent oxygen, so you are breathing a FiO2 of 21 percent without supplemental oxygen. When you use a flow rate of 1 liter per minute, your FiO2 increases to 24 percent. Every liter beyond that increases the FiO2 by about 4 percent.
What is normal PEEP range?
This, in normal conditions, is ~0.5, while in ARDS it can range between 0.2 and 0.8. This underlines the need for measuring the transpulmonary pressure for a safer application of mechanical ventilation.
What does PEEP 5 mean?
A low level of PEEP (∼5 cm H2O) is usually applied to offset the reduction in functional residual capacity (FRC) with supine positioning in mechanically ventilated patients, whereas higher levels may be applied to improve oxygenation in patients with hypoxemic respiratory failure.
Does PEEP increase FIO2?
PEEP levels can also be recommended based on the inspired oxygen fraction (FIO2), with a higher FIO2 requirement calling for higher PEEP. PEEP/FIO2 tables have been created to guide clinicians17, with two variants available (Table 1)4,18.
What is PEEP value?
Positive end-expiratory pressure (PEEP) is a value that can be set up in patients receiving invasive or non-invasive mechanical ventilation.
What level should the FiO2 and PEEP be set at?
The relationship between the clinician-set baseline PEEP and FiO2 levels is shown in Figure 2. Most clinicians selected PEEPs of 5, 8 or 10 cm H2O. When FiO2 was 50% or less, most clinicians selected either 5 or 8 cm H2O.
What is the highest PEEP level?
PEEP of 29 appears to be the highest tolerated PEEP in our patient. We noted an initial rise in blood flow across all cardiac valves followed by a gradual decline. Studies are needed to investigate the immediate effect and long-term impact of PEEP on cardiopulmonary parameters and clinical outcomes.
How do you calculate FiO2?
FiO2 = 20% + (4 x oxygen liter flow) Breathe Rate – how slow or fast the person is breathing.
What is FiO2 of 2l nasal cannula?
Published estimates of the FiO2 at 2 L/min have varied from 0.24 to 0.33 and at 4 L/min from 0.27–0.50. 7-9 Is it important to know how much variability there is around the FiO2 delivered from nasal cannulae?
What is a normal PaO2 FiO2 ratio?
PaO2/FiO2 ratio subdivided using the threshold of 100–200–300 according to the Berlin criteria of ARDS. PaO2 < 60 and >100 mmHG (out of normal range) versus PaO2 60–100 (in range).
How do you calculate desired FiO2?
“F” represents the FIO2 – the fraction (percent) of inspired oxygen that the patient is receiving expressed as a decimal (40% oxygen = FIO2 of 0.40). P divided by F = P/F ratio. Example: PaO2 = 90 on 40% oxygen (FIO2 = 0.40): 90 / 0.40 = P/F ratio = 225.
What is the respiration mode on a ventilator?
This mode requires a frequency of respirations per minute to be set. Patients who are attached to the ventilator then can trigger additional breaths that are greater than the set respirations per minute. If these patients cannot meet the trigger criteria, then the machine takes over and triggers all of the breaths.
When using assist control modes, should the respiratory rate be set at least high enough?
When using assist control modes, the respiratory rate should be set at least high enough so as to achieve a minute ventilation that is predicted for the patient. The respiratory rate can be set even higher if the patient has a known acid base imbalance during the time of intubation.
What happens if a ventilator does not initiate inspiration?
If the patient does not initiate inspiration, the ventilator automatically delivers the preset rate and tidal volume. This is to ensure minimum minute ventilation is achieved. Some ventilator settings are common between conventional modes of ventilation.
What is pressure controlled ventilation?
Pressure controlled ventilation is when a patient has a pressure setting on the ventilator and when the ventilator cycles a breath the pressure will continue to rise on the ventilator until the pre-set pressure limit is reached then the ventilator will cycle off and the patient will then exhale.
What is the normal tidal volume?
Tidal volume setting is dependent of the lung status. Normal tidal volume is 12 mL/kg ideal body weight; in patients with COPD, the tidal volume is 10 mL/kg ideal body weight and in patients with ARDS it is set to 6-8 mL/kg ideal body weight
Why is FRC reduced?
A reduction of FRC is because of the collapse of the unstable alveoli. Applying PEEP increases alveolar pressure and alveolar volume. Trigger sensitivity is a criteria used by the mechanical ventilator to determine if the patient is making an effort. There are two triggers; the flow trigger and pressure trigger.
Overview of Modes of Mechanical Ventilation
The modes of mechanical ventilation are important for clinicians who work with these patients to understand. An iron lung is an example of negative pressure ventilation. Most modern mechanical ventilators are positive pressure ventilation.
Modes of Mechanical Ventilation
Below is a brief overview of the different modes of mechanical ventilation. There are many different modes of ventilation that vary minimally between each other. We will focus on the common modes of mechanical ventilation and their clinical use.
Controlled Mechanical Ventilation (CMV)
One mode of mechanical ventilation is controlled mechanical ventilation (CMV). In controlled mechanical ventilation, the ventilator provides a mechanical breath on a preset timing. Patient respiratory efforts are ignored.
Assist Control
Another mode of mechanical ventilation is assist control. In assist control, the operator can set either a controlled volume or controlled pressure. A minimum number of preset mandatory breaths are delivered by the ventilator. The patient may trigger additional machine assisted breaths above the set rate.
Synchronized Intermittent Mechanical Ventilation (SIMV)
Synchronized intermittent mechanical ventilation (SIMV) is another mode of mechanical ventilation where the operator can set either a controlled pressure or controlled volume. Each mandatory breath in SIMV will deliver the identical set parameters (set pressure or volume) every specified number of seconds.
Pressure Support Ventilation (PSV)
In pressure support ventilation, a fixed amount of pressure (set by the clinician) augments each breath during the inspiratory phase of ventilation. The tidal volume is variable and depends on the patient’s effort and lung elasticity.
Volume Support Ventilation (VS)
In volume support ventilation the ventilator delivers a supported breath to help the patient reach a set tidal volume. This mode is dependent on the patient’s effort. The ventilator varies the inspiratory pressure level with each breath to achieve the target volume.
What is the function of oxygenation in a ventilated patient?
In a mechanically ventilated patient, this can be achieved by increasing the fraction of inspired oxygen (FiO 2%) or the positive end-expiratory pressure (PEEP).
What is invasive mechanical ventilation?
Invasive mechanical ventilation is an intervention that is frequently used in acutely ill patients requiring either respiratory support or airway protection. The ventilator allows gas exchange to be maintained while other treatments are given to improve the clinical condition. This activity reviews the indications, contraindications, ...
How many breaths does a ventilator give?
In assist control, if the rate is set at 12 and the patient breathes at 18, the ventilator will assistwith the 18 breaths, but if the rate drops to 8, the ventilator will take over controlof the respiratory rate and deliver 12 breaths in a minute.
How much pressure is required for mechanical ventilation?
Proper management of mechanical ventilation also requires an understanding of lung pressures and lung compliance. Normal lung compliance is around 100 ml/cmH20. This means that in a normal lung the administration of 500 ml of air via positive pressure ventilation will increase the alveolar pressure by 5 cm H2O. Conversely, the administration of positive pressure of 5 cm H2O will generate an increase in lung volume of 500 mL. When working with abnormal lungs, compliance may be much higher or much lower. Any disease that destroys lung parenchyma like emphysema will increase compliance, any disease that generates stiffer lungs (ARDS, pneumonia, pulmonary edema, pulmonary fibrosis) will decrease lung compliance.
How does mechanical ventilation affect the lungs?
Normal respiratory physiology works as a negative pressure system. When the diaphragm pushes down during inspiration , negative pressure in the pleural cavity is generated, this , in turn, creates negative pressure in the airways that suck air into the lungs.
What is the effect of ventilation?
Its most important effect is the removal of carbon dioxide (CO2) from the body, not on increasing blood oxygen content. Ventilation is measured as minute ventilation in the clinical setting, and it is calculated as respiratory rate (RR) times tidal volume (Vt). In a mechanically ventilated patient, the CO2 content of the blood can be modified by changing the tidal volume or the respiratory rate.
What is the positive pressure that will remain in the airways at the end of the respiratory cycle?
PEEP: The positive pressure that will remain in the airways at the end of the respiratory cycle (end of exhalation) is greater than the atmospheric pressure in mechanically ventilated patients. For a full description of the use of PEEP, please review the article titled “Positive End-Expiratory Pressure (PEEP).”
What does flow mean in PC-CMV?
Flow (v̇) = Tidal Volume / Inspiratory time. Hence, in PC-CMV, when Inspiratory time is fixed and if tidal volumes are increased, that means flow rate is increased.
What is respiratory failure?
Respiratory failure is caused by failure to oxygenate (Type I respiratory failure), with resultant decreae in PO2 or failure to ventilate (Type II respiratory failure), with a resultant increase in PCO2.
How to understand the equation of motion in volume control mode?
A set tidal volume/flow is delivered into the lungs. When air flows through the airways against the inherent resitance, it generates some pressure which is equal to flow x resistance. After air flows though the airways, it tries to open the alveoli against the elastic recoil thereby generating some pressure which is equal to the volume/ compliance. Then, finally you add the PEEP to these two pressures, it would give you the peak pressure.
How many variables can a ventilator control?
Ventilator can control only one variable at a time.
What is the work of breath?
Work of breath = Volume x Pressure. It is the work required to overcome the mechanical impedance to respiration. In other words, it is the work needed to overcome both elastic and airflow resistance. The time constant is a measure of the time needed for alveolar pressure to reach 63% of the change in airway pressure.
Why is PEEP not used in ventilation?
Such patients illustrate why PEEP should not automatically be applied as treatment for hypoxemic respiratory failure. Respiratory system compliance is much higher in relatively normal areas of lung than in areas of consolidation or collapse. As a result, application of PEEP may preferentially expand these more normal areas and not produce the desired effect in the involved lung. Distention of normal lung tissue stretches and narrows pulmonary vessels, which can raise pulmonary vascular resistance sufficiently to divert blood to the abnormal areas. Accordingly, applying PEEP can worsen rather than improve arterial oxygenation in such instances.
What is the meaning of FIO2?
FiO2 is the fraction of inspired oxygen. Essentially, it’s how much oxygen we’re giving to the patient. Recall that atmospheric oxygen is 21%, so your FiO2 will always be above that. The key with FiO2 is that we want to give the minimum amount the patient needs to maintain an adequate oxygen level in the blood.
What is the mode of a ventilator?
In addition to rate, FiO2 and PEEP, the MD or respiratory therapist will adjust how the ventilator delivers oxygen to the patient. We call this the “ventilator mode.” Modes can be broadly categorized as pressure controlled and volume controlled.
How does a respiratory therapist determine the correct respiratory rate?
The respiratory therapist or MD will determine the correct respiratory rate for the patient based off their unique physiologic needs. For example, if the patient is acidotic because they’re retaining their CO2, we can try increasing the respiratory rate to help the patient “blow off” their CO2. Some ventilator modes will allow a patient to initiate breaths, so it’s always possible that a patient could breathe above the rate set by the therapist. If that occurs, and we really need the patient to breathe at the prescribed rate, we usually sedate them in order to achieve this.
How does negative pressure ventilation work?
Negative pressure ventilation: Under normal circumstances, humans breathe utilizing negative pressure ventilation. When the diaphragm drops and the intercostal muscles pull the ribs outward, pleural pressure decreases below atmospheric pressure. This negative pressure draws air into the lungs. As the diaphragm moves up, pleural pressure increases which pushes air out of the lungs. The air comes IN during that period of negative pressure.
What is the process of adding oxygen to the body?
Oxygenation: The process of adding oxygen into the body. Think of this as the chemistry component.
Do ventilators have sound?
You’ll soon learn that ventilators (and everything else in the critical care setting) come with a lot of sound effects. There are two alarms I want you to be hypervigilent about…the high-pressure alarm and the low-pressure alarm.
