If you have gastroparesis and diabetes, you will need to control your blood glucose levels, especially hyperglycemia. Hyperglycemia may further delay the emptying of food from your stomach. Your doctor will work with you to make sure your blood glucose levels are not too high or too low and don’t keep going up or down. Your doctor may recommend
How does gastroparesis affect my blood sugar?
Signs and symptoms of gastroparesis include:
- Vomiting
- Nausea
- Abdominal bloating
- Abdominal pain
- A feeling of fullness after eating just a few bites
- Vomiting undigested food eaten a few hours earlier
- Acid reflux
- Changes in blood sugar levels
- Lack of appetite
- Weight loss and malnutrition
Does diabetic gastroparesis go away?
There is no cure for gastroparesis, but you can lessen symptoms with the following actions: Keep your blood sugar levels as close to their target range as possible. If playback doesn't begin shortly, try restarting your device. Videos you watch may be added to the TV's watch history and influence TV recommendations.
How to reverse gastroparesis?
- Hydrochloric acid. ...
- Stimulating the Vagus Nerve. ...
- Chewing your food properly . ...
- Mindful eating. ...
- Drinking enough water, at the right times. ...
- Digestive enzymes. ...
- After getting your body to digest with these short term solutions, we need to start implementing some long term solutions. ...
- Detox the Body. ...
- Heal the gut. ...
- Retrain Your Nervous System. ...
Can gastroparesis cause high blood sugar?
Unpredictable blood sugar changes. Although gastroparesis doesn't cause diabetes, frequent changes in the rate and amount of food passing into the small bowel can cause erratic changes in blood sugar levels. These variations in blood sugar make diabetes worse. In turn, poor control of blood sugar levels makes gastroparesis worse.

What are the symptoms of diabetic gastroparesis?
Signs and symptoms of gastroparesis include:Vomiting.Nausea.Abdominal bloating.Abdominal pain.A feeling of fullness after eating just a few bites.Vomiting undigested food eaten a few hours earlier.Acid reflux.Changes in blood sugar levels.More items...•
Is diabetic gastroparesis serious?
More recently, the term diabetic gastroparesis (DGp) has been used to describe a serious complication of diabetes resulting in delayed gastric emptying with associated upper gastrointestinal (GI) symptoms in the absence of any mechanical obstruction [2].
What causes diabetic gastroparesis?
Nausea, heartburn, or bloating can have many causes, but for people with diabetes, these common digestion issues shouldn't be ignored. That's because high blood sugar can lead to gastroparesis, a condition that affects how you digest your food. Diabetes is the most common known cause of gastroparesis.
How long does it take for diabetes to cause gastroparesis?
Most people with gastroparesis have had diabetes for at least 10 years and also have other complications related to the disease.
Does gastroparesis mean your stomach is paralyzed?
Gastroparesis, which means partial paralysis of the stomach, is a disease in which your stomach cannot empty itself of food in a normal way. If you have this condition, damaged nerves and muscles don't function with their normal strength and coordination — slowing the movement of contents through your digestive system.
Do you still poop with gastroparesis?
The delayed stomach emptying and reduced digestive motility associated with gastroparesis can have a significant impact on bowel function. Just as changes in bowel motility can lead to things like diarrhea and constipation, so also changes in stomach motility can cause a number of symptoms: nausea.
How do you fix diabetic gastroparesis?
Treatment for GastroparesisChanging eating habits. ... Controlling blood glucose levels. ... Medicines. ... Oral or nasal tube feeding. ... Jejunostomy tube feeding. ... Parenteral nutrition. ... Venting gastrostomy. ... Gastric electrical stimulation.
How did I get gastroparesis?
Known causes of gastroparesis include: poorly controlled type 1 diabetes or type 2 diabetes. a complication of some types of surgery – such as weight loss (bariatric) surgery or removal of part of the stomach (gastrectomy)
How do they fix gastroparesis?
Medications to treat gastroparesis may include: Medications to stimulate the stomach muscles. These medications include metoclopramide (Reglan) and erythromycin. Metoclopramide has a risk of serious side effects.
How do they test for gastroparesis?
Doctors use lab tests, upper gastrointestinal (GI) endoscopy, imaging tests, and tests to measure how fast your stomach is emptying its contents to diagnose gastroparesis....Tests to Measure Stomach EmptyingGastric emptying scan, also called gastric emptying scintigraphy. ... Gastric emptying breath test.More items...
What is the life expectancy of a person with gastroparesis?
In the reported literature, gastroparesis mortality is highly variable, ranging from 4% in a mixed cohort of inpatients and outpatients followed for 2 years to 37% in diabetic gastroparesis patients requiring nutritional support.
Who is most likely to get gastroparesis?
Affected Populations Gastroparesis demonstrates a gender bias affecting more women than men. Approximately 80% of idiopathic cases are women.
Does gastroparesis affect life expectancy?
For some people, gastroparesis affects the quality of their life, but is not life-threatening.
What is severe diabetic gastroparesis?
Diabetic gastroparesis is a severe complication resulting from uncontrolled diabetes that impairs quality of life and increases comorbid conditions and mortality. This complication is characterized by bloating, nausea, vomiting, weight loss, and early satiety but should be confirmed/diagnosed by scintigraphy.
How do you fix diabetic gastroparesis?
Treatment for GastroparesisChanging eating habits. ... Controlling blood glucose levels. ... Medicines. ... Oral or nasal tube feeding. ... Jejunostomy tube feeding. ... Parenteral nutrition. ... Venting gastrostomy. ... Gastric electrical stimulation.
What is the mortality rate of gastroparesis?
A review of several case series observed that the mortality rates in patients with gastroparesis range from 4% and 38%.
What Is Diabetic Gastroparesis?
Diabetic gastroparesis is a type of nerve damage that slows digestion. High blood sugar levels from diabetes can damage nerves and tissues in your...
What Increases My Risk For Diabetic Gastroparesis?
1. History of type 1 or type 2 diabetes for at least 10 years 2. Eye, nerve, or kidney problems due to diabetes
What Are The Signs and Symptoms of Diabetic Gastroparesis?
Your symptoms may be worse if you drink alcohol or smoke. You may have any of the following: 1. Constipation that may be replaced, at times, by dia...
How Is Diabetic Gastroparesis Diagnosed?
Your healthcare provider will feel your abdomen and ask about your diabetes. You may need any of the following tests: 1. A gastric emptying breath...
How Is Diabetic Gastroparesis Treated?
1. Medicines: 1. Motility medicines help your stomach muscles move food and liquids out of your stomach faster. These medicines also may help you d...
How Can I Manage My Symptoms?
1. Walk after you eat. This may help speed digestion. 2. Follow the meal plan that your healthcare or dietitian gave you. This meal plan can help d...
When Should I Seek Immediate Care?
1. You are vomiting more severely or for a longer period than usual. 2. You urinate less than usual, and your mouth is dry. 3. You feel dizzy and w...
When Should I Contact My Healthcare Provider?
1. Your blood sugar level is higher or lower than healthcare providers have told you it should be. 2. You continue to have pain and bloating in you...
Why does gastroparesis mean stomach paralysis?
Diving into it (double-yuck), we learned that gastroparesis literally means “stomach paralysis” because the stomach has difficulty emptying during digestion. Normally, digestion is aided by the vagus nerve, which helps churn your food into small pieces, before it’s mixed with enzymes and acid in your stomach to break the food down.
How to diagnose gastroparesis?
There are actually many ways to diagnosis gastroparesis, from drinking or eating barium, which allows your stomach to be X-rayed, to using different types of scans to measure the muscular activity of your stomach. (Sometimes they hide the barium in a beefsteak meal — no kidding!)
What is the best medicine for gastroparesis?
More severe cases of gastroparesis might require medication. Two common drugs that help with digestion are Reglan and Erythromycin. Both of them help stimulate muscle contraction in the abdomen. Reglan also helps with the related vomiting and nausea, but it can cause diarrhea (another yuck!).
Why is insulin so difficult to digest?
Because food is absorbed more slowly and unpredictably, dosing insulin can become incredibly difficult.
What happens if you eat too much food in your stomach?
This can worsen your nausea and vomiting and can sometimes even develop into a complete blockage between the stomach and the small intestine, requiring hospitalization. Yikes! There are treatments for bezoars that can break up the mass, but folks who are treated often have to suffer through months of a liquid diet. So trust us: you do not want to sit around and wait if you think you might have gastroparesis!
When is gastroparesis awareness month?
In case you didn’t know, August is officially Gastroparesis Awareness month, so a good time to think about having and keeping a healthy gut — especially given that this condition is a fairly common complication of diabetes.
What is the bill for functional GI and motility disorders?
At the moment they are rallying for support of a Congressional bill called The Functional Gastrointestinal and Motility Disorders Research Enhancement Act (HR 1187) that would fund research of functional GI and motility disorders and ways to improve diagnosis and treatments.
What medications can cause gastroparesis?
These include antidepressants, high blood pressure drugs, and certain diabetes treatments .
What is the best medicine for gastroparesis?
For some people with gastroparesis, medications can help: Dimenhydrinate ( Dramamine ), an over-the-counter antihistamine, helps prevent nausea and vomiting. Domperidone ( Motilium) manages problems in your upper digestive system that are linked to gastroparesis.
What happens if you eat too much food in your stomach?
Food that stays in your stomach too long can spoil and lead to the growth of bacteria. Undigested food can harden and form a lump called a bezoar. It can block your stomach and keep what you eat from moving into the small intestine. Gastroparesis can make it hard to control diabetes.
What happens when your stomach is damaged?
One of those is the vagus nerve, which controls how quickly your stomach empties. When it's damaged, your digestion slows down and food stays in your body longer than it should . This is a condition called gastroparesis.
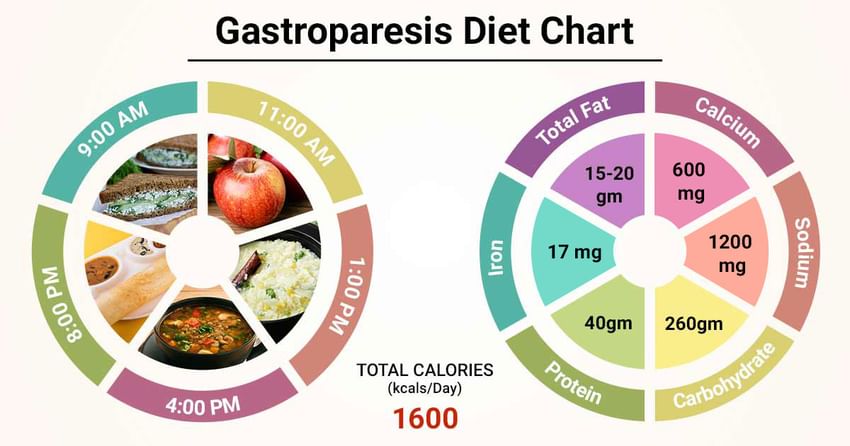
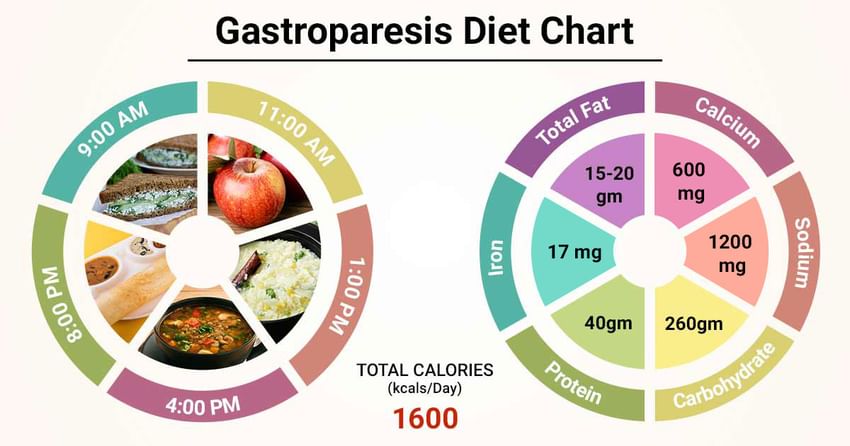
How many meals can you have with gastroparesis?
Instead of three times a day, you can have six small meals.
What is gastric manometry?
Gastric manometry: Your doctor guides a thin tube through your mouth and into your stomach. It measures how quickly you digest food.
How to slow down digestion?
Avoid foods that are high in fat, which can slow down digestion. Watch out for fiber, which takes longer for your body to process.
What causes gastroparesis?
Other conditions can compound your risk of developing the disorder, including previous abdominal surgeries or a history of eating disorders. Diseases and conditions other than diabetes can cause gastroparesis, such as: viral infections. acid reflux disease. smooth muscle disorders.
How does gastroparesis work?
In this procedure, a device is surgically implanted into your abdomen and it delivers electrical pulses to the nerves and smooth muscles of the lower part of your stomach. This may reduce nausea and vomiting. In severe cases, long-term gastroparesis sufferers may use feeding tubes and liquid food for nutrition.
Why is my glucose reading fluctuating?
The disease makes the digestion process hard to track, so glucose readings can fluctuate. If you have erratic glucose readings, share them with your doctor, along with any other symptoms you’re experiencing. Gastroparesis is a chronic condition, and having the disorder can feel overwhelming.
How do you know if you have gastroparesis?
The following are symptoms of gastroparesis: heartburn. nausea. vomiting of undigested food. early fullness after a small meal. weight loss. bloating. loss of appetite. blood glucose levels that are hard to stabilize.
What happens when blood sugar is high?
Extended periods of high glucose in the blood cause nerve damage throughout the body. Chronically high blood sugar levels also damage the blood vessels that supply the body’s nerves and organs with nutrition and oxygen, including the vagus nerve and digestive tract, both of which ultimately lead to gastroparesis.
Why does food stay in the stomach for a long time?
This occurs because the nerves that move food through the digestive tract are damaged, so muscles don’t work properly.
What happens when food isn't digested?
When food isn’t digested normally, it can remain inside the stomach, causing symptoms of fullness and bloating. Undigested food can also form solid masses called bezoars that can contribute to: nausea. vomiting. obstruction of the small intestines.
What are the signs and symptoms of diabetic gastroparesis?
Your symptoms may be worse if you drink alcohol or smoke. You may have any of the following:
How is diabetic gastroparesis diagnosed?
Your healthcare provider will feel your abdomen and ask about your diabetes. Tell him or her about all medicines you currently take. Certain medicines can affect how your digestive system works. Examples include opioids, tricyclic antidepressants, and certain COPD or asthma medicines. Some medicines used to treat type 2 diabetes may also affect your digestive system. Make sure your provider knows about all your current medicines. You may also need any of the following tests:
When should I call my doctor or diabetes care team?
Your blood sugar level is higher or lower than healthcare providers have told you it should be.
What is the name of the nerve damage that slows digestion?
Diabetic gastroparesis is a type of nerve damage that slows digestion. High blood sugar levels from diabetes can damage nerves and tissues in your stomach. The damage prevents your stomach from emptying normally. Gastroparesis is also called delayed gastric emptying.
What is a gastric emptying breath test?
A gastric emptying breath test (GEBT) will show how fast food moves from your stomach to your small intestine. The test measures the amount of carbon in your breath after you eat a meal prepared by healthcare providers. An x-ray or ultrasound may show how your stomach is working.
What are some examples of digestive problems?
Certain medicines can affect how your digestive system works. Examples include opioids, tricyclic antidepressants, and certain COPD or asthma medicines. Some medicines used to treat type 2 diabetes may also affect your digestive system. Make sure your provider knows about all your current medicines.
Why do you need an antibiotic for gastroparesis?
An antibiotic may be given for a short time to help your stomach empty more quickly. A feeding tube may be needed if your stomach cannot process food. You may need the feeding tube for a short time, until your stomach starts working properly. You may instead need a long-term feeding tube if your gastroparesis is severe.
What causes gastroparesis?
Gastroparesis is caused by damage to the vagus nerve, which controls the movement of food through the digestive tract . This nerve damage can happen as a result of long periods of high blood sugar levels. Chronically high blood sugar levels can also damage blood vessels that supply nerves and organs with nutrients and oxygen, ...
How common is gastroparesis?
Gastroparesis is common in people with diabetes. It affects between 27% and 58% of people with type 1 diabetes and 30% of those with type 2 diabetes. Read on to learn about diabetes and digestive problems.
What is the condition where food stays in the stomach longer than it should?
Gastroparesis is a chronic disorder of the digestive tract that causes food to remain in the stomach longer than it should. Gastroparesis is common in people with diabetes. It affects between 27% and 58% of people with type 1 diabetes and 30% of those with type 2 diabetes.
Why do diabetics have bloating?
Many people with diabetes experience digestive problems, such as constipation, bloating or nausea. These symptoms may be due to a condition called gastroparesis (also known as delayed gastric emptying). Gastroparesis is a chronic disorder of the digestive tract that causes food to remain in the stomach longer than it should.
What is delayed gastric emptying?
Gastroparesis, also known as “delayed gastric emptying” or “diabetic stomach” is a disorder of the digestive tract that causes food to remain in the stomach for a period of time that is longer than average.
What nerves are damaged in gastroparesis?
Gastroparesis is caused by damage to the vagus nerve, which controls the movement of food through the digestive tract. This nerve damage can happen as a result of long periods of high blood sugar levels. Chronically high blood sugar levels can also damage blood vessels that supply nerves and organs with nutrients and oxygen, including the vagus nerve and digestive tract, which also contributes to gastroparesis.
What are the treatment options for gastroparesis?
Once the diagnosis of gastroparesis is made, treatment options may include dietary changes, medications and changes to your insulin regimen.
What Is Gastroparesis?
Gastroparesis is a condition that prevents your stomach from properly moving food through the digestive track, causing delayed gastric emptying. Why does this happen? Typically, a damaged vagus nerve, which is responsible for controlling the process.
How Is Gastroparesis Diagnosed?
A gastroparesis diagnosis involves visiting your physician. They will likely need information about your medical history, and blood tests will probably be ordered. Once a gastrointestinal issue has been established, they may use a smart pill, or perform a gastric manometry, an electrogastrography, a barium X-ray or a biopsy to get more information.
What nerve is responsible for controlling blood sugar?
Typically, a damaged vagus nerve, which is responsible for controlling the process. This is particularly common in patients with diabetes because the vagus nerve, like other nerves in the body, can be damaged by diabetic neuropathy. Meaning, if an individual’s blood sugar levels remain uncontrolled for long periods of time and neuropathy develops, ...
Is gastroparesis a type 1 or type 2 diabetes?
Gastroparesis is an uncomfortable, and sometimes painful disorder that is incredibly common amongst people with both type 1 and type 2 diabetes. It’s so common, in fact, that up to 50% of people with diabetes will develop gastroparesis. However, despite its frequency, a lot of people remain in the dark when it comes to what ...
Why does gastroparesis occur?
Causes. It's not always clear what leads to gastroparesis, but in some cases it can be caused by damage to a nerve that controls the stomach muscles (vagus nerve). The vagus nerve helps manage the complex processes in your digestive tract, including signaling the muscles in your stomach to contract and push food into the small intestine.
What are the risk factors for gastroparesis?
Risk factors. Factors that can increase your risk of gastroparesis: Diabetes. Abdominal or esophageal surgery. Infection, usually from a virus. Certain medications that slow the rate of stomach emptying, such as narcotic pain medications. Scleroderma — a connective tissue disease.
Why does my stomach not empty?
But if you have gastroparesis, your stomach's motility is slowed down or doesn't work at all, preventing your stomach from emptying properly. The cause of gastroparesis is usually unknown. Sometimes it's a complication of diabetes, and some people develop gastroparesis after surgery. Certain medications, such as opioid pain relievers, ...
What is the name of the condition where the stomach pulverizes food?
Once your stomach pulverizes the food, strong muscular contractions (peristaltic waves) push the food toward the pyloric valve, which leads to the upper portion of your small intestine (duodenum). Gastroparesis is a condition that affects the normal spontaneous movement of the muscles (motility) in your stomach.
Why does food stay in the stomach longer?
A damaged vagus nerve can't send signals normally to your stomach muscles. This may cause food to remain in your stomach longer, rather than move into your small intestine to be digested. The vagus nerve and its branches can be damaged by diseases, such as diabetes, or by surgery to the stomach or small intestine.
How to tell if you have gastroparesis?
Nausea. Abdominal bloating. Abdominal pain. A feeling of fullness after eating just a few bites. Vomiting undigested food eaten a few hours earlier. Acid reflux. Changes in blood sugar levels.
What does it mean when you have a poor appetite?
Poor appetite can mean you don't take in enough calories, or you may be unable to absorb enough nutrients due to vomiting. Undigested food that hardens and remains in your stomach. Undigested food in your stomach can harden into a solid mass called a bezoar.
How to prevent gastroparesis?
If you have diabetes, you can prevent or delay nerve damage that can cause gastroparesis by keeping your blood glucose levels within the target range that your doctor thinks is best for you. Meal planning, physical activity, and medicines, if needed, can help you keep your blood glucose levels within your target range.
How do doctors treat gastroparesis?
How doctors treat gastroparesis depends on the cause, how severe your symptoms and complications are, and how well you respond to different treatments. Sometimes, treating the cause may stop gastroparesis. If diabetes is causing your gastroparesis, your health care professional will work with you to help control your blood glucose levels. When the cause of your gastroparesis is not known, your doctor will provide treatments to help relieve your symptoms and treat complications.
How does gastric stimulation work?
Gastric electrical stimulation (GES) uses a small, battery-powered device to send mild electrical pulses to the nerves and muscles in the lower stomach. A surgeon puts the device under the skin in your lower abdomen and attaches wires from the device to the muscles in the wall of your stomach. GES can help decrease long-term nausea and vomiting.
What is the National Institute of Diabetes and Digestive and Kidney Diseases?
This content is provided as a service of the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), part of the National Institutes of Health. The NIDDK translates and disseminates research findings to increase knowledge and understanding about health and disease among patients, health professionals, and the public. Content produced by the NIDDK is carefully reviewed by NIDDK scientists and other experts.
What is a venting gastrostomy?
Venting gastrostomy. Your doctor may recommend a venting gastrostomy to relieve pressure inside your stomach. A doctor creates an opening, called a gastrostomy, in your abdominal wall and into your stomach. The doctor then places a tube through the gastrostomy into your stomach.
Can you take IV nutrition for gastroparesis?
Parenteral nutrition. Your doctor may recommend parenteral, or intravenous (IV), nutrition if your gastroparesis is so severe that other treatments are not helping. Parenteral nutrition delivers liquid nutrients directly into your bloodstream. Parenteral nutrition may be short term, until you can eat again.
Does metoclopramide help with nausea?
Metoclopramide may also help relieve nausea and vomiting . Domperidone. This medicine also increases the contraction of the muscles in the wall of your stomach and may improve gastric emptying. However, this medicine is available for use only under a special program.