
What is the primary hematopoietic organ?
Hematopoietic organs are made up not only of hematopoietic cells but also of supporting tissue, or stroma. It is largely the interaction of the stroma with the stem cells that determines the type of blood cell production in the given organ. Immunologically active cells (lymphocytes and plasma cells) are also formed in the hematopoietic organs, which are the site of important …
How is hematopoiesis maintained in the human body?
Jan 14, 2020 · Hematopoietic Organs. In adult mammals and man, the principal hematopoietic organ is the bone marrow, where the red blood cells (erythrocytes), granular white blood cells (granular leukocytes), blood platelets (thrombocytes), and certain agranular white blood cells (lymphocytes) are formed.
What are hematopoietic stem cells?
May 20, 2021 · The hematopoietic system includes the bone marrow and, at different stages of fetal and postnatal development, the liver, spleen, lymph nodes, and thymus. The extensive use of red blood cell (RBC) or platelet transfusions and of antimicrobials in febrile neutropenic patients reflects the importance of the blood system in the pediatric intensive care unit (PICU) …
How is the hematopoietic system formed during early development?
The hematopoietic system, which comprises all the cellular components of the blood, is one of the earliest organ systems to evolve during embryo development. Hematopoietic stem cells (HSCs), which are rare blood cells residing in the bone marrow of the adult organism, are the founder cells that give rise to the entire hematopoietic system.
What is meant by hematopoietic organ?
Hematopoietic organs provide an environment where undifferentiated blood stem cells are able to self-renew, and at the same time generate offspring that differentiate into different blood cell types.
What is the first hematopoietic organ?
Extraembryonic hematopoiesis: The yolk sac The first hematopoietic emergence, a process named primitive hematopoiesis, starts during the third week of human development, before the establishment of the blood flow, in an extraembryonic tissue—the yolk sac (YS)—which is composed of visceral endoderm and mesoderm [3].Sep 6, 2016
Is liver a hematopoietic organ?
During human development, the liver and marrow both function as hematopoietic organs, but little is known about differences in the production of macrophages and neutrophils by these two organs.Jun 1, 1998
Which is hematopoietic organ in Foetus?
The human placenta is a hematopoietic organ during the embryonic and fetal periods of development.Mar 1, 2009
Is hematopoiesis the same as hematopoiesis?
As nouns the difference between hematopoiesis and hemopoiesis. is that hematopoiesis is (hematology|cytology) the process by which blood cells are produced; hematogenesis while hemopoiesis is (hematology|cytology) formation of new cellular components of the blood in myeloid or lymphatic tissue.
What is fetal hematopoiesis?
During fetal development, hematopoiesis occurs in multiple waves throughout the developing embryo and fetus, including extraembryonic yolk sac (YS), the para-aortic region of the embryo, fetal liver, and placenta before eventually homing to the bone marrow where it occurs just before birth.Feb 17, 2021
Is spleen hematopoietic?
For a few months in utero the normal human spleen is hematopoietic. By the close of the fifth fetal month, the function has moved permanently into the marrow.
Does hematopoiesis occur in the spleen?
Hematopoiesis occurs in the fetal liver and spleen. Hematopoietic stem and progenitor cells in the fetal liver migrate to the bone marrow and the marrow becomes the major hematopoietic site after birth.Mar 23, 2010
What is medullary hematopoiesis?
Extramedullary hematopoiesis (EMH or sometimes EH) refers to hematopoiesis occurring outside of the medulla of the bone (bone marrow). It can be physiologic or pathologic. Physiologic EMH occurs during embryonic and fetal development; during this time the main site of fetal hematopoiesis are liver and the spleen.
What type of tissue is hematopoietic?
The hematopoietic and lymphoid tissues give rise to and house erythrocytes (red blood cells), leukocytes (white blood cells), and platelets. The hematopoietic tissues arise from hematopoietic stem cells (HSCs) (Fig. 19.1), and include bone marrow, peripheral blood, and certain lymphoid tissue.
What is hematopoietic stage pregnancy?
During fetal development, hematopoiesis occurs in different areas of the developing fetus. This process has been divided into three phases: the mesoblastic phase, the hepatic phase, and the medullary phase.Jun 12, 2016
What are the main hematopoietic organs?
The hematopoietic system consists of organs and tissues, primarily the bone marrow, spleen, tonsils, and lymph nodes involved in the production of blood (Mosby Company, 2016). Blood is composed of the liquid component of plasma, and the solid components, which are mainly erythrocytes, leukocytes, and thrombocytes.
What is the term for the production of granulocytes, neutrophils, basophils, monocyte
Hematopoiesis refers to production of RBCs, granulocytes (neutrophils, eosinophils, basophils), monocytes, lymphocytes, platelets, and their stem, progenitor, and precursor cells. During embryogenesis and fetal development, hematopoiesis shifts from the yolk sac (primitive hematopoiesis) to the liver and, after the 20th week of gestation, to the bone marrow (definitive hematopoiesis). Although extramedullary erythropoiesis may persist for several weeks after birth, hematopoiesis takes place almost entirely in the bone marrow in the term infant.
What regulates the steady state of blood counts?
These hematopoietic growth factors are cytokines. Many of the cytokines have overlapping functions. However, gene targeting in the mouse (“knockout mouse”) of cytokines or their cognate receptors has identified the essential nonredundant functions for several hematopoietic growth factors. Mice deficient in erythropoietin (Epo), thrombopoietin (Tpo), and granulocyte colony-stimulating factor (G-CSF) suffer from severe anemia, thrombocytopenia, or neutropenia, respectively.
What are the cells that make up RBCs?
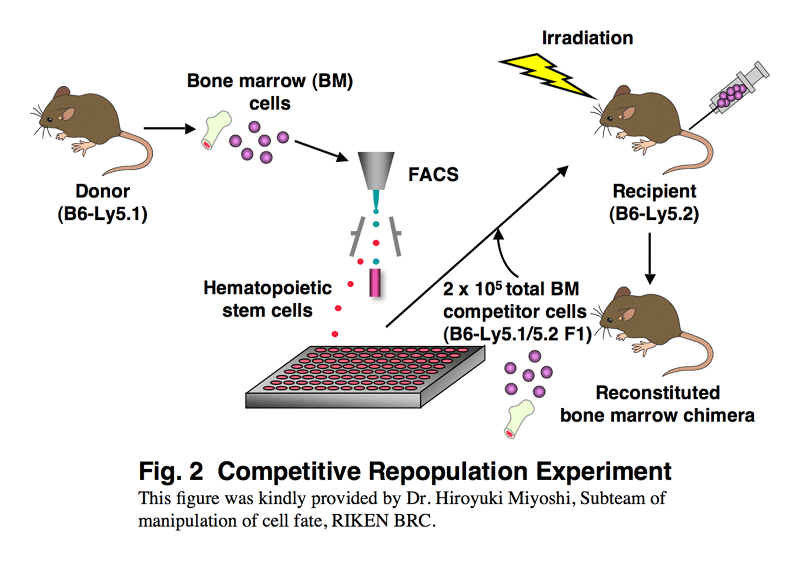
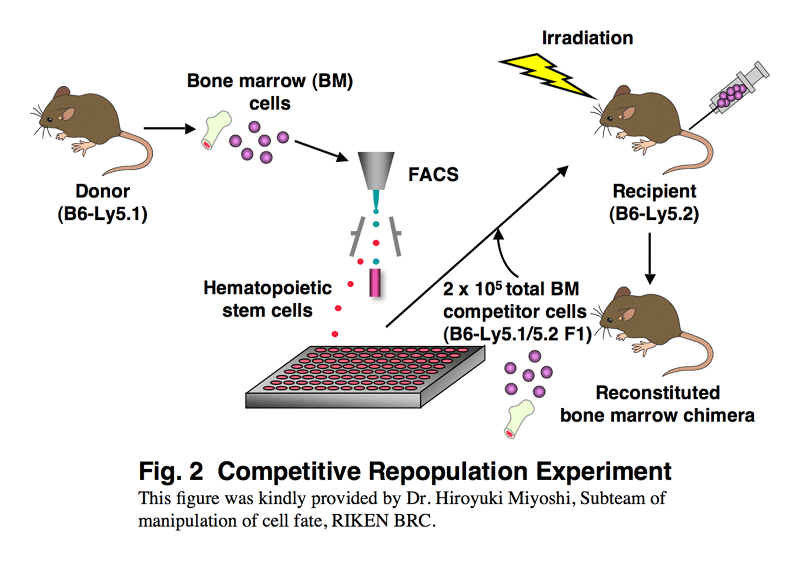
RBCs, granulocytes (neutrophils, eosinophils, basophils), monocytes (and their tissue forms, macrophages), megakaryocytes, and lymphocytes develop from a self-renewing pluripotent hematopoietic stem cell ( Fig. 86.2 ). Stem cells look like small lymphocytes and are not usually distinguishable from them by microscopy. They constitute less than 1% of the nucleated cells in the normal marrow. Immunophenotyping provides rapid identification of cell lineage and stage of development. , Hematopoietic stem cells are defined by the cell surface expression of the CD34 antigen. The “trilineage myeloid” stem cell (erythroid, granulocyte, megakaryocyte) has been designated the colony forming unit-stem (CFU-S; in humans, CD34 + cells) on the basis of murine bone marrow culture assays and experiments in which the spleens of lethally irradiated mice infused with donor marrow cells are found to contain colonies, each consisting of precursors of RBCs, granulocytes, monocytes, and megakaryocytes. Lymphopoiesis appears to depend on a separate progenitor cell, a common lymphoid progenitor cell derived from CD34 + stem cells.
Why is bone marrow absorbed rapidly?
Because the bone marrow circulation connects with the general circulation, fluids and medications injected into the marrow are absorbed as rapidly as when administered intravenously. •.
What is hematopoiesis in biology?
What is hematopoiesis? The hematopoietic system, which comprises all the cellular components of the blood, is one of the earliest organ systems to evolve during embryo development. Hematopoietic stem cells (HSCs), which are rare blood cells residing in the bone marrow of the adult organism, are the founder cells that give rise to ...
Where are the hematopoietic cells formed?
During early development, the various cell types of the hematopoietic system are formed at distinct anatomical niches within the embryo, in a spatially and temporally controlled manner, until this function is completely taken over by the bone marrow and thymus (for T-lymphoid cell generation) just prior to birth.
Which tissue is the primary site of hematopoiesis?
In human and other vertebrate embryos, a homologous region called the aorta-gonad-mesonephros (AGM) as well as the earlier stage precursor tissue, the Para-aortic Splanchnopleura ( P-Sp), were identified as the primary sites for definitive hematopoiesis during early embryogenesis.
What cells are found in the yolk sac?
Upon the separation of yolk sac from the embryo at the 19-day stage, when the blood circulation between the extra- and intra-embryonic compartments is still not established, only erythroid and myeloid cells were identified in the yolk sac.
Where does haematopoiesis occur?
In children, haematopoiesis occurs in the marrow of the long bones such as the femur and tibia. In adults, it occurs mainly in the pelvis, cranium, vertebrae, and sternum.
What are the two models of hematopoiesis?
Two models for hematopoiesis have been proposed: determinism and stochastic theory . For the stem cells and other undifferentiated blood cells in the bone marrow, the determination is generally explained by the determinism theory of haematopoiesis, saying that colony stimulating factors and other factors of the haematopoietic microenvironment determine the cells to follow a certain path of cell differentiation. This is the classical way of describing haematopoiesis. In stochastic theory, undifferentiated blood cells differentiate to specific cell types by randomness. This theory has been supported by experiments showing that within a population of mouse haematopoietic progenitor cells, underlying stochastic variability in the distribution of Sca-1, a stem cell factor, subdivides the population into groups exhibiting variable rates of cellular differentiation. For example, under the influence of erythropoietin (an erythrocyte-differentiation factor), a subpopulation of cells (as defined by the levels of Sca-1) differentiated into erythrocytes at a sevenfold higher rate than the rest of the population. Furthermore, it was shown that if allowed to grow, this subpopulation re-established the original subpopulation of cells, supporting the theory that this is a stochastic, reversible process. Another level at which stochasticity may be important is in the process of apoptosis and self-renewal. In this case, the haematopoietic microenvironment prevails upon some of the cells to survive and some, on the other hand, to perform apoptosis and die. By regulating this balance between different cell types, the bone marrow can alter the quantity of different cells to ultimately be produced.
What organs are enlarged during fetal development?
It may cause these organs to increase in size substantially. During fetal development, since bones and thus the bone marrow develop later, the liver functions as the main haematopoetic organ. Therefore, the liver is enlarged during development. Extramedullary hematopoiesis and myelopoiesis may supply leukocytes in cardiovascular disease and inflammation during adulthood. Splenic macrophages and adhesion molecules may be involved in regulation of extramedullary myeloid cell generation in cardiovascular disease.
What is the name of the process of forming blood cells?
In a healthy adult person, approximately 10 11 –10 12 new blood cells are produced daily in order to maintain steady state levels in the peripheral circulation.
What is the lymphoid lineage?
The lymphoid lineage is composed of T-cells, B-cells and natural killer cells. This is lymphopoiesis. Cells of the myeloid lineage, which include granulocytes, megakaryocytes and macrophages, are derived from common myeloid progenitors, and are involved in such diverse roles as innate immunity and blood clotting.
What are the three types of blood cells?
Cell types. All blood cells are divided into three lineages. Red blood cells, also called erythrocytes, are the oxygen-carrying cells. Erythrocytes are functional and are released into the blood. The number of reticulocytes, immature red blood cells, gives an estimate of the rate of erythropoiesis.
Where does blood formation occur in the body?
As development progresses, blood formation occurs in the spleen, liver and lymph nodes. When bone marrow develops, it eventually assumes the task of forming most of the blood cells for the entire organism. However, maturation, activation, and some proliferation of lymphoid cells occurs in the spleen, thymus, and lymph nodes. In children, haematopoiesis occurs in the marrow of the long bones such as the femur and tibia. In adults, it occurs mainly in the pelvis, cranium, vertebrae, and sternum.
Structure and Function of the Bone Marrow
During embryogenesis and fetal development, hematopoiesis shifts from the yolk sac to the liver and, after the twentieth week of gestation, to the bone marrow. 1 Although hepatic erythropoiesis may persist for several weeks after birth, in the term infant hematopoiesis takes place almost entirely in the bone marrow.
Hematopoiesis
Cells within the hematopoietic island include the RBCs, granulocytes (neutrophils, eosinophils, basophils), monocytes and macrophages, platelets, lymphocytes, and their precursors. The earliest precursors, or stem cells, are thought to look like small lymphocytes and are not usually distinguishable from them by microscopy.
Introduction
As a standard part of this blog, every Wednesday I publish a text concerning medicine and medical achievements. Sometimes I write about the history of medicine, sometimes about the current situation, and sometimes about what awaits us in the future of medicine. I often write about new discoveries by researchers and scientists around the world.
What is haematopoiesis?
Hematopoiesis is one of the most important processes in our body, without which life as we know it would not be possible. It is the shaping of the cellular elements of the blood. There are several types of cells in the blood that perform different functions, but they all have their own lifespan.
How do lungs fit in the story of haematopoiesis?
The lungs are one of the essential organs for maintaining life. The basic and logical role of the lungs is the exchange of gases, ie oxygen (O2) and carbon dioxide (CO2). They are located inside the thoracic cavity and if we look macro-anatomically, they are divided into so-called lobes.
New findings
Two papers from 2017 (links below) describe the hematopoietic potential of the lungs. I will talk more about paper published on March 22, 2017. As for the hematopoietic role of the lungs, it is related to the biosynthesis of platelets. Platelets, or thrombocytes, are fragments of cells called megakaryocytes.
Why is this important?
These findings are much more than another addition to our theoretical understanding of the human body. They have great importance for understanding the role of the lungs in the case of thrombocytopenia. Thrombocytopenia is a condition in which there is a decrease in platelets in the blood, for whatever reason.
Overview
Haematopoiesis is the formation of blood cellular components. All cellular blood components are derived from haematopoietic stem cells. In a healthy adult person, approximately 10 –10 new blood cells are produced daily in order to maintain steady state levels in the peripheral circulation.
Process
Haematopoietic stem cells (HSCs) reside in the medulla of the bone (bone marrow) and have the unique ability to give rise to all of the different mature blood cell types and tissues. HSCs are self-renewing cells: when they differentiate, at least some of their daughter cells remain as HSCs, so the pool of stem cells is not depleted. This phenomenon is called asymmetric division. The other daughters of HSCs (myeloid and lymphoidprogenitor cells) can follow any of the other differentia…
Location
In developing embryos, blood formation occurs in aggregates of blood cells in the yolk sac, called blood islands. As development progresses, blood formation occurs in the spleen, liver and lymph nodes. When bone marrow develops, it eventually assumes the task of forming most of the blood cells for the entire organism. However, maturation, activation, and some proliferation of lymphoid cells occurs in the spleen, thymus, and lymph nodes. In children, haematopoiesis occurs in the m…
Maturation
As a stem cell matures it undergoes changes in gene expression that limit the cell types that it can become and moves it closer to a specific cell type (cellular differentiation). These changes can often be tracked by monitoring the presence of proteins on the surface of the cell. Each successive change moves the cell closer to the final cell type and further limits its potential to become a different cell type.
Other animals
In some vertebrates, haematopoiesis can occur wherever there is a loose stroma of connective tissue and slow blood supply, such as the gut, spleen or kidney.
See also
• Clonal hematopoiesis
• Erythropoiesis-stimulating agents
• Haematon
• Haematopoietic stimulants:
• Leukocyte extravasation
Further reading
• Godin, Isabelle; Cumano, Ana, eds. (2006). Hematopoietic stem cell development. Springer. ISBN 978-0-306-47872-7.
External links
• Hematopoietic cell lineage in KEGG
• Hematopoiesis and bone marrow histology