What is hepatic ketogenesis? Ketogenesis is the biochemical process through which organisms produce ketone bodies through breakdown of fatty acids and ketogenic amino acids. This process supplies energy under circumstances such as fasting or caloric restriction to certain organs, particularly the brain, heart and skeletal muscle.
What is the role of the liver in the pathogenesis of ketosis?
Activation in the liver inhibits lipogenesis, promotes fatty acid oxidation, switches off acetyl-CoA carboxylase, turns on malonyl-CoA decarboxylase, and consequently induces ketogenesis.
What is the significance of ketogenesis in humans?
Ketogenesis becomes significant under conditions of food (carbohydrate) deprivation. Provision of peripheral tissues, such as skeletal muscle and heart, with ketone bodies as an alternative fuel for energy production results in glucose sparing for organs depending on glucose as an energy source.
What hormones are involved in the regulation of ketogenesis?
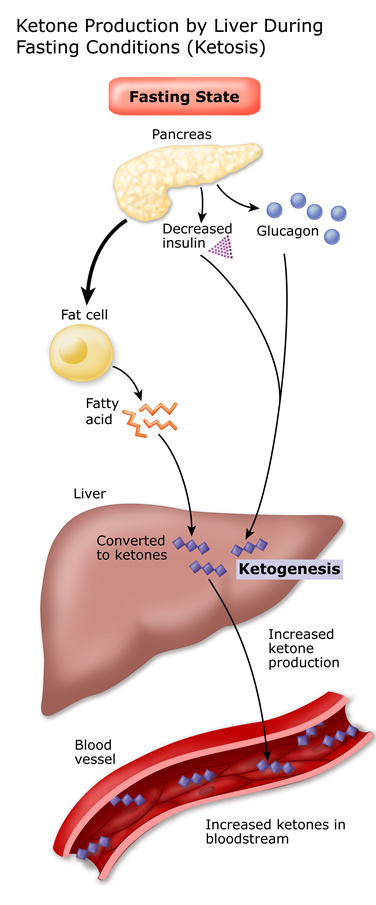
Two hormones are primarily responsible for the regulation of ketogenesis by the liver: glucagon and insulin.
What is the relationship between gluconeogenesis and ketogenesis?
(In rare metabolic diseases, insufficient gluconeogenesis can cause excessive ketogenesis and hypoglycemia, which may lead to the life-threatening condition known as non-diabetic ketoacidosis .)
What hormones are involved in the ketogenic pathway?
Regulation of Ketogenesis. Ketogenesis can be upregulated by hormones such as glucagon, cortisol, thyroid hormones, and catecholamines by causing a more significant breakdown of free fatty acids, thus increasing the amount available to be used in the ketogenic pathway.
Why does the liver not use ketone bodies?
Although it is the primary site that produces ketone bodies, the liver does not use ketone bodies because it lacks the necessary enzyme beta ketoacyl-CoA transferase. Mechanism. Ketogenesis occurs primarily in the mitochondria of liver cells.
What is the name of the pathway that produces ketone bodies?
Biochemistry, Ketogenesis - StatPearls - NCBI Bookshelf. Ketogenesis is a metabolic pathway that produces ketone bodies, which provide an alternative form of energy for the body. The body is constantly producing small amounts of ketone bodies that can make 22 ATP each in normal circumstances, and it is regulated mainly by insulin.
What happens when carbohydrate stores are significantly decreased?
When carbohydrate stores are significantly decreased or fatty acid concentration increases, there is an upregulation of the ketogenic pathway and an increased production of ketone bodies. This can be seen in conditions such as type 1 diabetes, alcoholism, and starvation.
What is the threshold for DKA?
The threshold for DKA is a glucose level of 250. However, it is typically greater than this amount. Once carbohydrate stores become depleted and gluconeogenesis cannot occur anymore, ketogenesis is substantially increased, and greater amounts of ketone bodies are produced.
How is acetoacetate converted to acetone?
Acetoacetate can be converted to either acetone through non-enzymatic decarboxylation or to beta-hydroxybutyrate via beta-hydroxybutyrate dehydrogenase. Acetoacetate and beta-hydroxybutyrate are the two ketone bodies used by the body for energy.
What is the process of producing acetone, acetoacetate, and beta-hydroxybutyrate?
Ketogenesis produces acetone, acetoacetate, and beta-hydroxybutyrate molecules by breaking down fatty acids. These ketones are water-soluble lipid molecules made up of two R-groups attached to a carbonyl group (C = O). Because they are water-soluble, they do not require lipoproteins for transport.
What is the key factor in the regulation of ketogenesis?
A key factor in the regulation of ketogenesis is the availability of nonesterified long-chain fatty acids to the liver, which in turn is controlled by their release from adipose tissue . The enzyme responsible for the initiation of the hydrolysis of stored triacylglycerols to fatty acids is hormone-sensitive lipase. As its name implies, this enzyme is exquisitely sensitive to hormones: adrenaline (in the plasma) and noradrenaline (released from sympathetic nerve endings) are activators, whereas insulin inhibits the activity. In small mammals glucagon is also an activator of the enzyme, but this does not seem to be the case in the human.
What is the first step in the ketogenesis process?
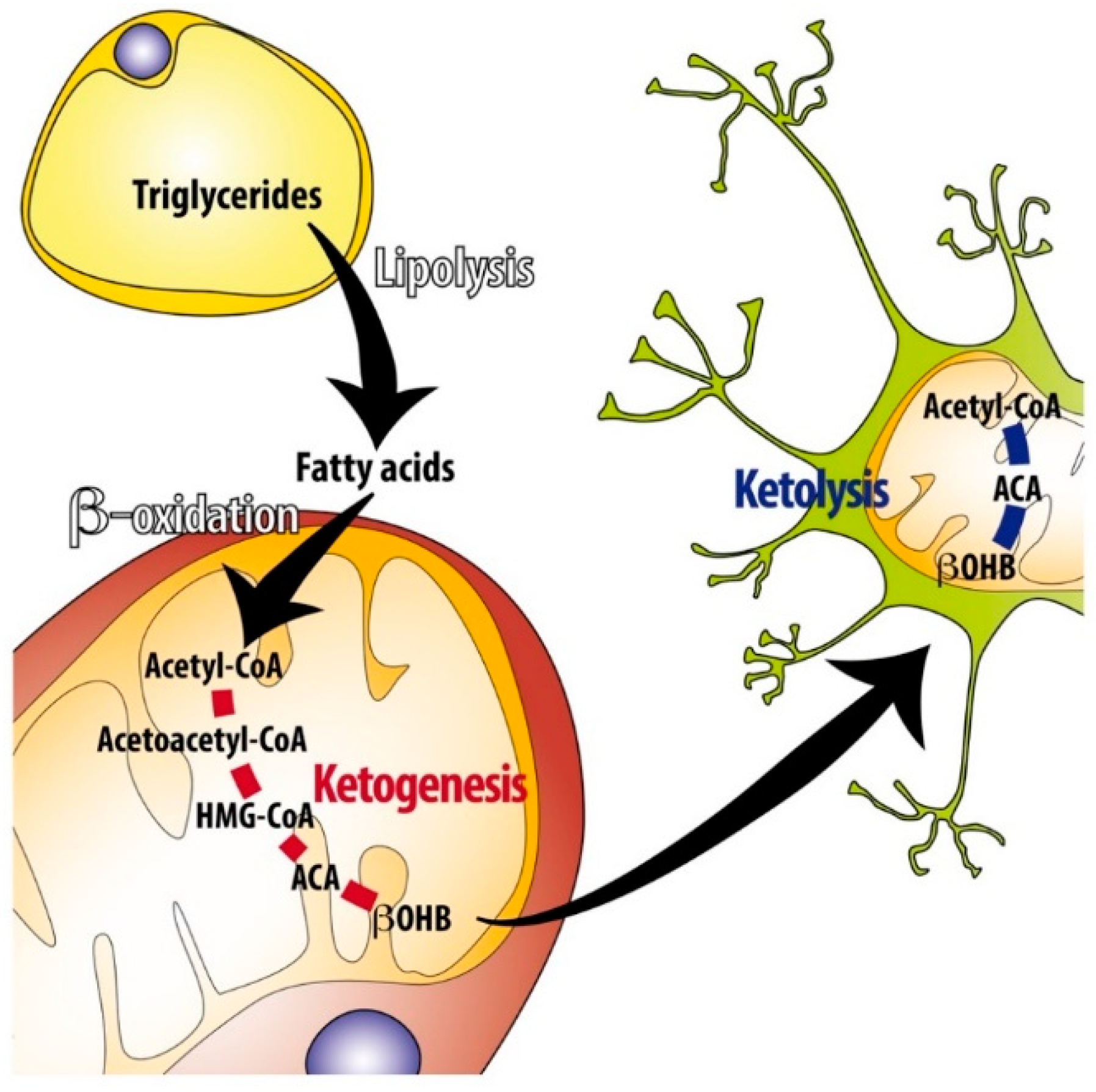
Metabolic process. The first step in ketogenesis is the hydrolysis of triglycerides to yield fatty acids. In the liver, control of ketogenesis is largely due to the blocking of other pathways in the metabolism of the carbon product of fatty acid oxidation, acetyl-CoA (oxidation and fat synthesis).
What is the role of ketone bodies in the body?
Provision of peripheral tissues, such as skeletal muscle and heart, with ketone bodies as an alternative fuel for energy production results in glucose sparing for organs depending on glucose as an energy source. The brain then can use ketones as well as glucose, ...
What are the two substrates of ketogenesis?
From an overall perspective, there are two other substrates to consider: NAD + and ADP (+ inorganic phosphate).
Which isoform of HMG synthase is genetically distinct from the cytosolic one?
The mitochondrial isoform of HMG-CoA synthase is genetically distinct from the cytosolic one, which generates the precursor for cholesterol synthesis. Hydroxymethylglutaryl-CoA lyase (HMG-CoA lyase, EC4.1.3.4) finally generates acetoacetate by cleaving off acetyl-CoA from the HMG-CoA intermediate.
Is acetoacetate a reversible enzyme?
This enzyme is allosterically activated by phosphatidyl choline. The reaction is fully reversible. Net flux depends on substrate concentrations. Acetoacetate and beta-hydroxybutyrate (but not acetone) can become a significant energy fuel for brain after several days of adaptation to starvation conditions.
Does insulin help with ketogenesis?
Insulin plays a central role in arresting ketogenesis; there may be, however, a lag period of a few hours before there is an appreciable decline in the rate of production of ketoacids . This is usually not an urgent aspect of therapy because, based on data from adult subjects with starvation ketosis, the maximum rate of hepatic production of ketoacids is about 1 mmol/min. Hence, the administration of insulin can be delayed if required, as in the case of a patient with DKA and an initial PK of less than 4 mmol/L (see the following discussion). In our view, the only circumstance in which insulin must be administered urgently in a patient with DKA is the presence of ECG changes related to hyperkalemia because of its effect to induce a shift of K + ions into cells. The effects of insulin to treat hyperglycemia are minimal early in therapy. Rather, the P Glucose will fall initially as a result of re-expansion of the ECF volume (dilution) and glucosuria caused by the rise in GFR. Six to eight hours after therapy begins, insulin will lower P Glucose by increasing the rate of oxidation of glucose because competing fat fuels are no longer available, and by promoting the synthesis of glycogen.
How does ketogenesis occur?
Ketogenesis may or may not occur, depending on levels of available carbohydrates in the cell or body. This is closely related to the paths of acetyl-CoA: 1 When the body has ample carbohydrates available as energy source, glucose is completely oxidized to CO 2; acetyl-CoA is formed as an intermediate in this process, first entering the citric acid cycle followed by complete conversion of its chemical energy to ATP in oxidative phosphorylation. 2 When the body has excess carbohydrates available, some glucose is fully metabolized, and some of it is stored in the form of glycogen or, upon citrate excess, as fatty acids (see lipogenesis ). Coenzyme A is recycled at this step. 3 When the body has no free carbohydrates available, fat must be broken down into acetyl-CoA in order to get energy. Under these conditions, acetyl-CoA cannot be metabolized through the citric acid cycle because the citric acid cycle intermediates (mainly oxaloacetate) have been depleted to feed the gluconeogenesis pathway. The resulting accumulation of acetyl-CoA activates ketogenesis.
Which hormones regulate ketogenesis?
Insulin and glucagon are key regulating hormones of ketogenesis, with insulin being the primary regulator. Both hormones regulate hormone-sensitive lipase and acetyl-CoA carboxylase. Hormone-sensitive lipase produces diglycerides from triglycerides, freeing a fatty acid molecule for oxidation. Acetyl-CoA carboxylase catalyzes the production ...
What is acetoacetate converted to?
Acetoacetate, which can be converted by the liver into β-hydroxybutyrate, or spontaneously turn into acetone. Most acetoacetate is reduced to beta-hydroxybutyrate, which serves to additionally ferry reducing electrons to the tissues, especially the brain, where they are stripped back off and used for metabolism.
What is the role of AMPK in ketogenesis?
Ketogenesis in healthy individuals is ultimately under the control of the master regulatory protein AMPK, which is activated during times of metabolic stress, such as carbohydrate insufficiency. Activation in the liver inhibits lipogenesis, promotes fatty acid oxidation, switches off acetyl-CoA carboxylase, turns on malonyl-CoA decarboxylase, ...
Which amino acids are ketogenic?
Deaminated amino acids that are ketogenic, such as leucine, also feed TCA cycle, forming acetoacetate & ACoA and thereby produce ketones. Besides its role in the synthesis of ketone bodies, HMG-CoA is also an intermediate in the synthesis of cholesterol, but the steps are compartmentalised. Ketogenesis occurs in the mitochondria, whereas ...
How is acetone metabolized?
Acetone, which is generated through the decarboxylation of acetoacetate, either spontaneously or through the enzyme acetoacetate decarboxylase. It can then be further metabolized either by CYP2E1 into hydroxyacetone (acetol) and then via propylene glycol to pyruvate, lactate and acetate (usable for energy) and propionaldehyde, ...
Where are ketones produced?
Ketone bodies are produced mainly in the mitochondria of liver cells , and synthesis can occur in response to an unavailability of blood glucose, such as during fasting. Other cells, e.g. human astrocytes, are capable of carrying out ketogenesis, but they are not as effective at doing so. Ketogenesis occurs constantly in a healthy individual.
What is the key factor in the regulation of ketogenesis?
A key factor in the regulation of ketogenesis is the availability of nonesterified long-chain fatty acids to the liver, which in turn is controlled by their release from adipose tissue . The enzyme responsible for the initiation of the hydrolysis of stored triacylglycerols to fatty acids is hormone-sensitive lipase. As its name implies, this enzyme is exquisitely sensitive to hormones: adrenaline (in the plasma) and noradrenaline (released from sympathetic nerve endings) are activators, whereas insulin inhibits the activity. In small mammals glucagon is also an activator of the enzyme, but this does not seem to be the case in the human.
What is the first step in ketogenesis?
The first step in ketogenesis is the hydrolysis of triglycerides to yield fatty acids. In the liver, control of ketogenesis is largely due to the blocking of other pathways in the metabolism of the carbon product of fatty acid oxidation, acetyl-CoA (oxidation and fat synthesis).
What is the parent ketone body?
AcAc, the parent ketone body, can be converted to β-OHB by mitochondrial β-hydroxybutyrate dehydrogenase. Ketone bodies can be used for energy by most tissues. The exceptions are the liver as well as tissues that have no mitochondria, such as red blood cells and the lens of the eye.
What is phase V in metabolic?
Metabolic Phase V (Until Nutrient Depletion Begins) Phase V begins when rates of ketogenesis exceed gluconeogenesis and continues until starvation begins.11 The length of this phase depends on an individual’s body mass index, fat and muscle percentages, physical activity levels, and state of health.
Where do ketone bodies form?
The formation of ketone bodies occurs primarily in the liver via the following enzymatic reactions, all of which are present in the mitochondrial matrix, except for the spontaneous decarboxylation of AcAc to acetone, which occurs in the blood. The reactions of ketone body synthesis are as follows: 1.
What are the two substrates of ketogenesis?
From an overall perspective, there are two other substrates to consider: NAD + and ADP (+ inorganic phosphate).
Which isoform of HMG synthase is genetically distinct from the cytosolic one?
The mitochondrial isoform of HMG-CoA synthase is genetically distinct from the cytosolic one, which generates the precursor for cholesterol synthesis. Hydroxymethylglutaryl-CoA lyase (HMG-CoA lyase, EC4.1.3.4) finally generates acetoacetate by cleaving off acetyl-CoA from the HMG-CoA intermediate.
How does ketosis help you lose weight?
In the short term, you can lose weight quickly, because it reduces the body’s stores of glycogen and water. In the long term, it can suppress your appetite leading to a lower calorie intake. ). Ketosis is quite complex, but this article explains what it is and how it can benefit you.
How much energy does the brain get from ketones?
Trusted Source. ). In fact, after only three days of starvation, the brain gets 25% of its energy from ketones. During long-term starvation, this number rises to around 60% ( 8.
What is the metabolic state of the body?
Ketosis is a metabolic state in which there’s a high concentration of ketones in the blood. This happens when fat provides most of the fuel for the body, and there’s limited access to glucose. Glucose (blood sugar) is the preferred fuel source for many cells in the body. Ketosis is most often associated with ketogenic and very low carb diets.
Is ketosis good for you?
Ketosis may be beneficial for some people, but you should ask your doctor before switching to a very low carb diet, in case it’s not suitable for you. Ketosis is safe for most people. However, some people may experience side effects, including bad breath, headaches, and constipation.
Does ketosis have therapeutic effects?
Some scientists have suggested that ketosis and ketogenic diets may have other therapeutic effects, although it’s worth noting that not all experts agree on this ( 27#N#Trusted Source#N#, 26 ).
Is ketosis the same as ketoacidosis?
Ketosis is not the same as ketoacidosis. People often confuse ketosis and ketoacidosis. While ketosis is part of normal metabolism, ketoacidosis is a dangerous metabolic condition that can be fatal if left untreated.
Does ketosis help the brain?
Ketosis and gluconeogenesis are perfectly capable of fulfilling the brain’s energy needs . Here is more info about ketogenic diets and the brain: How Low-Carb and Ketogenic Diets Boost Brain Health. summary. When the brain isn’t getting enough glucose , it can use ketones for energy.
How does ketogenesis work?
A vital topic for your NEET curriculum, ketogenesis is a metabolic process through which energy is produced for the body. It works by creating ketone bodies. Each ketone body can produce up to 22 ATP under normal circumstances. Ketone body synthesis fastens in the presence of increased fatty acids and lack of carbohydrate.
What happens when the ketogenic pathway overproduces ketone bodies?
In such a case, the ketogenic pathway overproduces ketone bodies. This situation may lead to type 1 diabetes. Furthermore, it can result from starvation and alcoholism as well.
What is the process of producing ketones?
Ans. Ketogenesis is a catabolic pathway of metabolism. In this process, fatty acids and certain ketogenic amino acids are weakened to derive energy by alternative means. Ketone bodies are produced in the ketogenesis process. Our body continuously produces ketone bodies in low amounts but in certain cases like starving, when carbohydrates are present in less amount in diet, ketogenesis is preferred to compensate for the energy requirements. Ketoacidosis is a condition in which an excess amount of ketone bodies gets accumulated in the body. This condition may also be fatal.
Why do ketone bodies increase in blood?
Ketone body synthesis fastens in the presence of increased fatty acids and lack of carbohydrate. A process which is functional almost all the time, ketone bodies can be used as an alternative source of energy. Moreover, during fasting and overnight sleep, ketone bodies increase in blood. However, excessive ketogenesis often results in ketoacidosis, ...
Where does ketone body synthesis take place?
The ketone body synthesis through ketogenesis takes place in mitochondria of liver cells. The steps, which have been illustrated in the image above, are also explained below. Fatty acids are transported into mitochondria via CPT-1. Then through beta-oxidation, acetyl CoA breaks it down.
What is the primary regulator of ketogenesis?
The primary hormonal regulator of ketogenesis is insulin. Therefore, people with diabetes suffer the most from ketoacidosis. Ketoacidosis can be detected initially through some symptoms like bad breath, fatigue, weight loss, frequent urination, excessive thirst, etc.
What is the oxidation process of fatty acids?
Fatty acids undergo 𝛽-oxidation in the liver mitochondria to generate a high amount of energy and form three compounds , that are known as “ketone bodies”. These ketone bodies are water-soluble and do not require lipoproteins for transportation across the membrane. Ketone bodies are lipid molecules having a carbonyl group attached to two -R groups.