What is massive necrosis of the liver?
Massive necrosis refers to events in individual acini in which all hepatocytes are dead. abscess resulting from infection of the umbilicus and direct vascular extension to the liver. fibrosis limited to the zones around hepatic venules; a response to congestive heart failure or to intoxication.
What is the clinical course of acute hepatic necrosis?
The clinical course of acute hepatic necrosis resembles an acute, toxic injury to the liver with sudden and precipitous onset, marked elevations in serum aminotransferase levels, and early signs of hepatic (or other organ) dysfunction or failure despite minimal or no jaundice. Rapid recovery after withdrawal of the agent is also typical.
What causes ischemic necrosis of the liver?
Underperfusion of the liver causing ischemic necrosis is postulated in some cases. In others, a history of a procedure under gas anesthesia within the last 24 hours exists.
What is hepatic necrosis in camelids?
Hepatic Necrosis. Hepatic necrosis is an uncommon finding but is an important differential diagnosis for camelids with high hepatocellular liver enzymes.

What causes hepatic necrosis?
Acute hepatic necrosis is typically caused by a direct hepatotoxin and is usually dose dependent and “expected”, rather than idiosyncratic. Latency to Onset. The time to onset of acute hepatic necrosis is typically short, 1 to 14 days.
What happens in liver necrosis?
Necrosis, also referred to as cell death, is a process in which viable cells become nonviable, resulting in dissolution of the cell contents. Under physiological conditions it is a well-regulated process that leads to replacement of individual effete cells.
What type of necrosis occur in liver?
Liver necrosis (whether it appears as ballooning degeneration, apoptotic bodies, or coagulative necrosis) occurs mainly in the centrilobular zones, which leads to dropout and loss of hepatocytes.
Can the liver heal with necrosis?
Introduction. Massive hepatic necrosis (MHN) with consequent fulminant liver failure is a rare but very severe complication of liver disease with various etiology. 1 Although this condition often results in the death of the patients, 10–20% of them can recover spontaneously, without liver transplantation.
What are 4 warning signs of a damaged liver?
Tip-offs to Liver DamageJaundice or yellowing of the eyes or skin.Pain and distention of the abdomen due to the release of fluid from the liver.Swelling of lower legs due to fluid retention.Confusion or forgetfulness. ... Dark-colored urine.Pale-colored stool.Chronic fatigue.Nausea or vomiting.
How quick is death from liver failure?
who are hospitalized for cirrhosis develop ACLF. Of these, 25% died within one month and 40% died within three months.
What is the most common cause of necrosis?
Trauma. Injuries, such as hip dislocation or fracture, can damage nearby blood vessels and reduce blood flow to bones. Steroid use. Use of high-dose corticosteroids, such as prednisone, is a common cause of avascular necrosis.
How does necrosis start?
Necrosis is the death of the cells in your body tissues. Necrosis can occur due to injuries, infections or diseases. Lack of blood flow to your tissues and extreme environmental conditions can also cause necrosis. While dead body tissue can be removed, it can't be brought back to good health.
Is necrosis fatal?
Necrosis is the death of cells in living tissue caused by external factors such as infection, trauma, or toxins. As opposed to apoptosis, which is naturally occurring and often beneficial planned cell death, necrosis is almost always detrimental to the health of the patient and can be fatal.
What is the best drink to flush your liver?
6 Detox Drinks to Cleanse Your LiverCoffee. Coffee is good for the liver, especially because it protects against issues such as fatty liver disease. ... Ginger and lemon drink. ... Oatmeal drink. ... Tumeric drink. ... Green tea. ... Grapefruit drink.
What are signs that your liver is struggling?
SymptomsSkin and eyes that appear yellowish (jaundice)Abdominal pain and swelling.Swelling in the legs and ankles.Itchy skin.Dark urine color.Pale stool color.Chronic fatigue.Nausea or vomiting.More items...•
What are the last days of liver failure like?
The person may be unable to tell night from day. He or she may also display irritability and personality changes, or have memory problems. As brain function continues to decline, he or she will become sleepy and increasingly confused. This state can progress to unresponsiveness and coma.
What is massive liver necrosis?
Massive hepatic necrosis is a key event underlying acute liver failure, a serious clinical syndrome with high mortality. Massive hepatic necrosis in acute liver failure has unique pathophysiological characteristics including extremely rapid parenchymal cell death and removal.
What type of necrosis is fatty liver?
Fatty liver disease involves the accumulation of triglycerides in hepatocytes, necrosis of hepatocytes, inflammation, and often fibrosis with progression to cirrhosis. The two-hit model summarizes the important early metabolic events leading to hepatocellular necrosis in nonalcoholic steatohepatitis (NASH).
How does alcohol damage the liver pathophysiology?
Alcohol contributes to liver injury through a multitude of ways as depicted. Alcohol is metabolized to acetaldehyde; both alcohol and acetaldehyde have toxic effects on hepatocytes. Damaged hepatocytes in turn release DAMPs that recruit innate and adaptive immune cells that perpetuate further liver injury.
How does liver disease cause encephalopathy?
Hepatic encephalopathy is caused when toxins that are normally cleared from the body by the liver accumulate in the blood, eventually traveling to the brain. Many of the symptoms of hepatic encephalopathy are reversible when promptly detected and treated.
What is the effect of liver enzymes on hepatocellular necrosis?
Thus increased blood activity of these enzymes may be indicative of active hepatocellular disease.
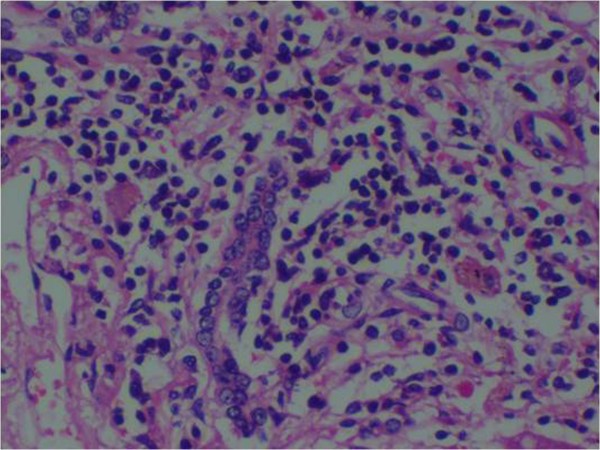
What cells are preserved in hepatocyte necrosis?
In areas of severe hepatocyte necrosis and collapse, the reticulin framework and endothelial cells are often preserved and are mixed with variable numbers of inflammatory cells and hypertrophied Kupffer cells or macrophages that contain a brown ceroid pigment.
What is the most common lesion in hepatitis?
Severe hepatic necrosis with loss of lobular architecture and collapse of the reticulin framework is the commonest lesion seen in either viral infection 59 or an idiosyncratic drug reaction. In viral hepatitis, necrosis tends to be panacinar in distribution, whereas in toxic injury it is zonal. Most acute liver failure is associated with massive confluent necrosis 60,61 and it is difficult to identify any viable hepatocytes. In non-A-E hepatitis or indeterminate hepatitis, there may be lymphoid aggregates around bile ducts with congestion of centrilobular sinusoids. In hepatitis B there is a minimal inflammatory infiltrate, whereas in Epstein-Barr viral hepatitis, centrilobular necrosis with bridging and collapse may be obvious with cholestasis and lymphoid “blast cells.” In most cases, some evidence of regeneration can be found, 61 with proliferation of ductules. The degree and pattern of necrosis do not correlate with the development of encephalopathy or cerebral edema. 60-62
What causes bile stasis?
Hepatic necrosis or hepatocyte swelling may lead to impaired bile flow, resulting in biliary stasis.
What is the second most common cause of death due to iron poisoning?
Acute hepatic necrosis is the second most common cause of death due to iron poisoning. It is characterized by hypertransaminasemia, with enzyme concentrations in the range of several thousands of international units per liter ( Tenenbein, 2001; Robertson and Tenenbein, 2005 ). When this occurs, the prognosis is poor because the site of damage is Zone 1 of the hepatic acinus. Therefore, hepatocytes that possess the capacity for hepatic regeneration are affected; this differs from acetaminophen poisoning, despite similar transaminase concentrations. The prognosis for the latter is less severe because the site of damage is Zone 3 of the hepatic acinus, the daughter cells.
What is necrosis accompanied by destruction of the endothelial cells?
Hepatocellular necrosis accompanied by destruction of the endothelial cells results in central lobular hemorrhage into the zone of necrotic hepatocytes.
Where does submassive necrosis occur?
Liver necrosis (whether it appears as ballooning degeneration, apoptotic bodies, or coagulative necrosis) occurs mainly in the centrilobular zones, which leads to dropout and loss of hepatocytes.
What is colliquative necrosis?
colliquative necrosis liquefactive necrosis. fat necrosis necrosis in which fat is broken down into fatty acids and glycerol, usually occurring in subcutaneous tissue as a result of trauma. liquefactive necrosis necrosis in which the necrotic material becomes softened and liquefied.
What is tubular necrosis?
acute tubular necrosis acute renal failure with mild to severe damage or necrosis of tubule cells, usually secondary to either nephrotoxicity, ischemia after major surgery, trauma (see crush syndrome ), severe hypovolemia, sepsis, or burns. See also lower nephron nephrosis.
What is the process of swelling of the nucleus?
The process involves swelling of the nucleus (pyknosis), fragmentation of the nucleus (karyorrhexis) and complete dissolution of the nuclear chromatin (karyolysis). Necrosis is caused by disease, trauma or interference with blood supply.
What is the term for the death of a cell?
Necrosis. The death of cells, a portion of tissue, or a portion of an organ due to permanent damage of some sort, such as a lack of oxygen supply to the tissues. Mentioned in: Anaerobic Infections, Angiography, Flesh-Eating Disease, Necrotizing Enterocolitis. Gale Encyclopedia of Medicine.
What is the term for the localized death of plant and animal tissue, such as the response of a leaf to?
the localized death of plant and animal tissue, such as the response of a leaf to invasion by a pathogen. An affected area is described as being ‘necrotic’. see DIPHTHERIA.
What are the changes that occur after death of a body tissue?
necrosis. The structural changes, such as those of GANGRENE, that follow death of a body tissue. The most obvious changes are in the cell nuclei which become shrunken and condensed (pyknosis) and no longer take a basic stain. Cell CYTOPLASM becomes more homogeneous and spaces (vacuoles) develop.
What is the term for the death of one or more cells?
ne·cro· sis. , pl. necroses ( nĕ-krō'sis, -sēz) Pathologic death of one or more cells, or of a portion of tissue or organ, resulting from irreversible damage; earliest irreversible changes are mitochondrial, consisting of swelling and granular calcium deposits seen by electron microscopy; most frequent visible alterations are nuclear pyknosis ...
How to treat hepatic failure?
Your doctor may prescribe medications. If only part of your liver is damaged, surgery may be recommended to remove the damaged part. A doctor can also take imaging tests of your liver to look for damage.
What causes liver failure?
Chronic liver failure is usually a result of cirrhosis or alcohol-related liver disease (ARLD). The American Liver Foundation states that alcoholism is the most common cause of cirrhosis in the United States. Usually, your liver breaks down any alcohol that you consume.
How long does it take for liver failure to develop?
Chronic liver failure develops more slowly that acute liver failure. It can take months or even years before you exhibit any symptoms. Chronic liver failure is often the result of cirrhosis, which is usually caused by long-term alcohol use. Cirrhosis occurs when healthy liver tissue is replaced with scar tissue.
What percentage of people with alcohol cirrhosis have it?
The American Liver Foundation says that some form of cirrhosis affects 10 to 20 percent of people who drink heavily.
What is the condition where fat cells are found in the liver?
Alcoholic hepatitis: Alcoholic hepatitis is characterized by fat cells in the liver, inflammation, and scarring. According to the American Liver Foundation, up to 35 percent of people who drink heavily will develop this condition.
Why does my liver fail?
It may happen suddenly, without showing any symptoms. Common causes of acute liver failure include poisoning from mushrooms or drug overdose, which can occur from taking too much acetaminophen (Tylenol).
How to prevent liver failure?
Prevention of hepatic failure. One of the easiest ways to prevent liver failure is to moderate your drinking. The Mayo Clinic recommends that healthy women limit their alcohol consumption to one drink per day. Healthy men over the age of 65 should also limit their alcohol consumption to one drink a day. Men under 65 should consume no more ...
What causes the liver to fail?
Cancer. Cancer that either begins in or spreads to your liver can cause your liver to fail.
What causes a blockage in the veins of the liver?
Diseases of the veins in the liver. Vascular diseases, such as Budd-Chiari syndrome, can cause blockages in the veins of the liver and lead to acute liver failure.
What are the complications of liver failure?
Acute liver failure often causes complications, including: 1 Excessive fluid in the brain (cerebral edema). Too much fluid causes pressure to build up in your brain, which can lead to disorientation, severe mental confusion and seizures. 2 Bleeding and bleeding disorders. A failing liver cannot make enough clotting factors, which help blood to clot. Bleeding in the gastrointestinal tract is common with this condition. It may be difficult to control. 3 Infections. People with acute liver failure are more likely to develop infections, particularly in the blood and in the respiratory and urinary tracts. 4 Kidney failure. Kidney failure often occurs after liver failure, especially if you had an acetaminophen overdose, which damages both your liver and your kidneys.
What is liver failure?
Overview. Acute liver failure is loss of liver function that occurs rapidly — in days or weeks — usually in a person who has no preexisting liver disease. It's most commonly caused by a hepatitis virus or drugs, such as acetaminophen.
How do you know if you have liver failure?
Signs and symptoms of acute liver failure may include: Yellowing of your skin and eyeballs (jaundice) Pain in your upper right abdomen. Abdominal swelling (ascites) Nausea. Vomiting. A general sense of feeling unwell (malaise) Disorientation or confusion. Sleepiness.
How to avoid hepatitis?
Avoid contact with other people's blood and body fluids. Accidental needle sticks or improper cleanup of blood or body fluids can spread hepatitis viruses. Sharing razor blades or toothbrushes also can spread infection.
Which supplements cause liver failure?
Herbal supplements. Herbal drugs and supplements, including kava, ephedra, skullcap and pennyroyal, have been linked to acute liver failure.