
Herpetic gingivostomatitis
Gingivostomatitis is a combination of gingivitis and stomatitis, or an inflammation of the oral mucosa and gingiva. Herpetic gingivostomatitis is often the initial presentation during the first herpes simplex infection. It is of greater severity than herpes labialis which is often the subsequent presentations. Primary herpetic gingivostomatitis is the most common viral infection of the mouth.
Herpes Simplex Virus Infection
An infection caused by the virus HSV.
DNA virus
A DNA virus is a virus that has DNA as its genetic material and replicates using a DNA-dependent DNA polymerase. The nucleic acid is usually double-stranded DNA but may also be single-stranded DNA. DNA viruses belong to either Group I or Group II of the Baltimore classification system for viruses. Single-stranded DNA is usually expanded to double-stranded in infected cells. Although Group VII vi…
What is herpes gingivostomatitis?
Herpes (her-pees) gingivostomatitis (jin-jih-vuh-sto-muh-ti-tis) is a mouth infection. It is also called herpetic (her-peh-tik) stomatitis. This infection is common in young children. Your child may get this infection many times in his lifetime. Herpes gingivostomatitis is different from hand-foot-and-mouth...
How long does herpetic gingivostomatitis last?
Because little ones often put toys in their mouths, the sharing of these playthings should be off limits during any outbreak as well. Most cases of Herpetic Gingivostomatitis go away in about 2 weeks but, unfortunately, once a child develops this infection, they also become more prone to developing recurring mouth sores and ulcers.
How is primary herpetic gingivostomatitis treated?
Primary acute herpetic gingivostomatitis can be managed on an outpatient basis with aggressive oral hydration, analgesia, and topical and systemic antiviral therapy. The main criteria for hospital admission include severe dehydration and pain.
Is herpetic gingivostomatitis an STD?
Is gingivostomatitis an STD? No, but it can be caused by HSV-1, which can occasionally cause genital herpes. Gingivostomatitis is typically passed from person to person from mouth-to-mouth contact, such as kissing or sharing eating utensils.
How is herpetic gingivostomatitis transmitted?
The virus is transmitted by direct contact with infected lesions or from saliva, which may remain infectious for several months. The clinical features include fever, lymphadenopathy, and painful mouth and throat followed by the appearance of multiple vesicles throughout the oral mucosa and lips.
How do you catch gingivostomatitis?
Gingivostomatitis is a contagious mouth infection that causes painful sores, blisters, and swelling. It usually spreads through the saliva of an infected individual or by direct contact with a lesion or sore. Gingivostomatitis is most common in young children, usually under 6 years old, but can also occur in adults.
How do you treat herpetic gingivostomatitis?
Key pointsHSV Gingivostomatitis is usually a self-limiting illness, which resolves without complications.The mainstay of treatment is ensuring adequate hydration and analgesia.Aciclovir should be administered in children who are immunocompromised.
How does gingivostomatitis start?
Gingivostomatitis is common among children. It may occur after infection with the herpes simplex virus type 1 (HSV-1), which also causes cold sores. The condition may also occur after infection with a coxsackie virus. It may occur in people with poor oral hygiene.
How long does herpetic gingivitis last?
The sores and swelling will go away on their own in 1 to 2 weeks. Your child may need to stay home from daycare or school until the sores and swelling are gone. That's because the infection is easily spread to others. Children can spread it through their saliva (drool) to items such as toys or cups.
Is gingivostomatitis serious?
Gingivostomatitis is an infection caused by the herpes virus—the same virus that causes cold sores. Gingivostomatitis is very damaging to the skin, causing ulcers in the mouth and blisters on the lips. It most often occurs in young children.
How did my child get herpetic gingivostomatitis?
Oral HSV1 can commonly affect toddlers and young children and is transmitted through saliva, often from a person with existing cold sores. Your children can get it from sharing utensils, putting toys or things in the mouth and thumb sucking, to name a few. Usually the sores clear up within two weeks.
How can herpetic gingivostomatitis be prevented?
Because herpetic gingivostomatitis can spread easily, the best prevention is avoiding close contact with infected people. Children shouldn't kiss or share food, drinks, or utensils with an infected person.
Can gingivostomatitis be cured?
Gingivostomatitis sores usually disappear within two to three weeks without treatment. Your doctor may prescribe an antibiotic and clean the infected area to promote healing if bacteria or a virus is the cause of gingivostomatitis.
Is herpetic gingivostomatitis recurring?
Herpetic gingivostomatitis infections can present as acute or recurrent. Acute infection refers to the first invasion of the virus, and recurrent is when reactivation of the latent virus occurs. Acute herpetic gingivostomatitis primarily occurs in children, particularly of those under the age of six years old.
What can you eat with gingivostomatitis?
Give your child cool, bland foods and liquids. Applesauce, gelatin, or frozen treats are good choices. Do not give your child salty or acidic foods and drinks, such as orange juice.
Is herpetic stomatitis contagious?
Approximately one quarter of primary infections manifest as gingivostomatitis, typically in the 1-5 year old age range, but can occur in older children. HSV is highly contagious, and is spread by direct contact with infected oral secretions and lesions.
Is herpetic gingivostomatitis recurring?
Herpetic gingivostomatitis infections can present as acute or recurrent. Acute infection refers to the first invasion of the virus, and recurrent is when reactivation of the latent virus occurs. Acute herpetic gingivostomatitis primarily occurs in children, particularly of those under the age of six years old.
What causes gingivostomatitis in adults?
Gingivostomatitis may occur because of: herpes simplex virus type 1 (HSV-1), the virus that causes cold sores. coxsackievirus, a virus often transmitted by touching a surface or an individual's hand contaminated with feces (this virus can also cause flu-like symptoms) certain bacteria (Streptococcus, Actinomyces)
Is viral stomatitis contagious?
Is stomatitis contagious? Yes. It is contagious. It can be spread by close contact with cold sores.
What is gingivostomatitis?
Gingivostomatitis is a combination of gingivitis and stomatitis, or an inflammation of the oral mucosa and gingiva. Herpetic gingivostomatitis is often the initial presentation during the first ("primary") herpes simplex infection. It is of greater severity than herpes labialis (cold sores) which is often the subsequent presentations. Primary herpetic gingivostomatitis is the most common viral infection of the mouth.
What is the pathophysiology of gingivostomatitis?
Herpetic gingivostomatitis originates from a primary infection of HSV-1. The series of events that take place during this infection include replication of the herpes simplex virus, cell lysis and finally, destruction of the mucosal tissue.
What is the HSV infection?
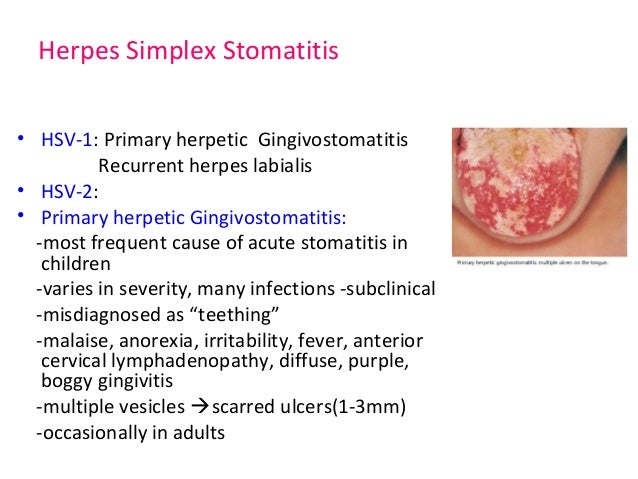
Herpetic gingivostomatitis is an infection caused by the herpes simplex virus (HSV). The HSV is a double-stranded DNA virus categorised into two types; HSV-1 and HSV-2. HSV-1 is predominantly responsible for oral, facial and ocular infections whereas HSV-2 is responsible for most genital and cutaneous lower herpetic lesions. Both HSV-1, and HSV-2 can be the cause of herpetic gingivostomatitis, although HSV-1 is the source of infection in around 90% of cases.
What is the most common viral infection in the mouth?
Primary herpetic gingivostomatitis is the most common viral infection of the mouth. Primary herpetic gingivostomatitis (PHGS) represents the clinically apparent pattern of primary herpes simplex virus (HSV) infection, since the vast majority of other primary infections are symptomless. PHGS is caused predominantly by HSV-1 ...
How long does it take to recover from herpes labialis?
Most individuals who are immunocompetent will fully recover from recurrent herpes labialis in 7 to 14 days. However treatment with antipyretics, oral anaesthetics and analgesics is often needed. In severe cases of herpetic gingivostomatitis, mouth rinses are useful in relieving oral discomfort.
What is the cause of teething in infants?
Teething in infants: A study mentioned that "primary tooth eruption begins at about the time that infants are losing maternal antibody protection against the herpes virus. Also, reports on teething difficulties have recorded symptoms which are remarkably consistent with primary oral herpetic infection such as fever, irritability, sleeplessness, and difficulty with eating." Another study highlighted that "younger infants with higher residual levels of antibodies would experience milder infections and these would be more likely to go unrecognized or be dismissed as teething difficulty."
What is the appearance of a herpetic infection on the mucosa?
The histological appearance of a herpetic infection on the mucosa includes degeneration of stratified squamous epithelial cells, the loss of intercellular connections and inflammatory infiltrate around the capillaries of the dermis layer. An intact herpetic vesicle presents as an intraepithelial blister histologically.
What are the clinical features of herpetic gingivostomatitis?
The clinical features of herpetic gingivostomatitis are sufficiently characteristic to permit accurate diagnosis in most cases. Other conditions with similar oral lesions are limited and include herpangina, aphthous stomatitis, Steven-Johnson syndrome, and other enanthems resulting from infection and drug sensitivities. In herpangina, the lesions are smaller (1 to 3 mm), more often vesicular, and usually localized to the soft palate. The ulcers in aphthous stomatitis are few, relatively deep, and circumscribed. Aphthosis is characterized by periodic recurrence, whereas acute herpetic gingivostomatitis and pharyngitis are limited to a single occurrence. Herpetic pharyngitis, when exudative, must be distinguished from pharyngitis due to Streptococcus pyogenes, adenovirus, Epstein-Barr virus, and diphtheria. The diagnosis of acute herpetic disease of the oropharynx can be confirmed by examination of Giemsa- or Wright-stained smears of scrapings from the base of a fresh lesion (Tzanck test) and by culture of scrapings or swab specimens. Techniques for the rapid detection of viral antigens or DNA are widely available.
What is primary gingivostomatitis?
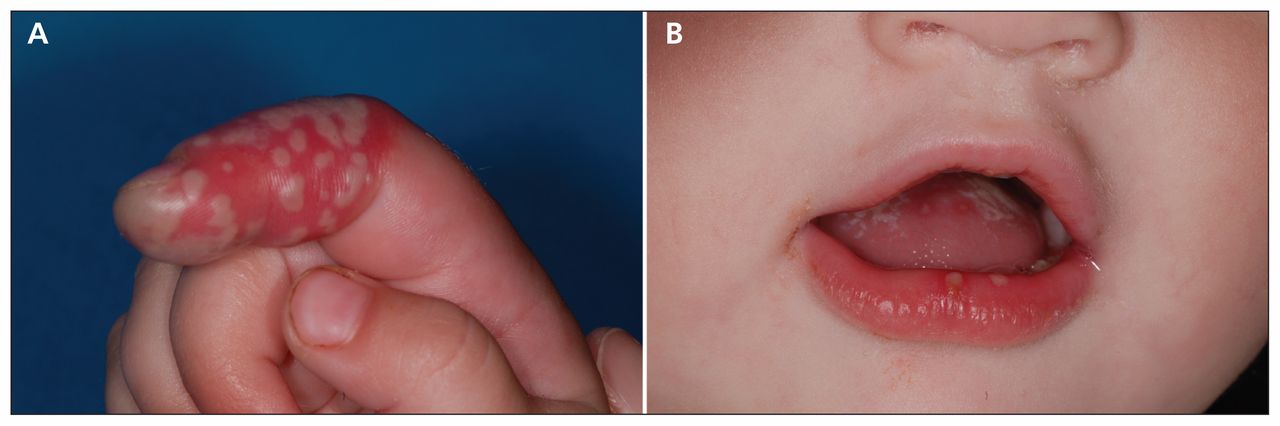
Primary herpetic gingivostomatitis is an infection of the oral cavity caused by the herpes simplex virus type 1 (Figure 11-11). In the primary infection, the virus ascends through sensory and autonomic nerves, where it persists as latent HSV in neuronal ganglia. Secondary manifestations result from various stimuli such as sunlight, trauma, fever, ...
What causes lateral pharyngeal abscess?
Herpetic gingivostomatitis involving pericoronal tissue has also been reported as a cause of the lateral pharyngeal abscess.
How long does it take for gingivostomatitis to resolve?
Acute herpetic gingivostomatitis is a self-limiting condition usually resolving within 3 weeks from the onset of symptoms. Treatment predominantly involves observation and palliative care. This may involve topical anesthetics and over-the-counter pain relief, such as acetaminophen or ibuprofen. Fluids and electrolyte status should be monitored as needed to avoid dehydration.
Why is it difficult to diagnose herpetic laryngotracheitis?
The diagnosis of herpetic laryngotracheitis may be difficult because of the inaccessibility of the lesions. The disease should be suspected in any immunocompromised patient with herpetic lesions of the mouth, upper airway, or skin of the face, especially if endotracheal intubation has been performed. In such patients, bronchoscopic examination is indicated for sampling of suspected areas for cytology and viral culture.
How is HSV-1 spread?
This virus is found worldwide and is spread predominantly via infected saliva or contact with active perioral lesions. In the United States, the estimated HSV-1 seroprevalence is greater than 50% among individuals 14 to 49 years old.
Where does secondary herpetic stomatitis occur?
Secondary herpetic stomatitis can occur on the palate, gingiva, or on the oral mucosa. Primary herpetic gingivostomatitis appears as a diffuse, erythematous, shiny involvement of the gingival and the adjacent oral mucosa, with varying degrees of edema and gingival bleeding. Initial viral presentation appears as spherical clustered vesicles on ...
Overview
Gingivostomatitis is a combination of gingivitis and stomatitis, or an inflammation of the oral mucosa and gingiva. Herpetic gingivostomatitis is often the initial presentation during the first ("primary") herpes simplex infection. It is of greater severity than herpes labialis (cold sores) which is often the subsequent presentations. Primary herpetic gingivostomatitis is the most common viral inf…
Signs and symptoms
The symptoms can be mild or severe and may include:
• Not able to chew or swallow
• Sores on the inside of the cheeks or gums
• Fever
• General discomfort, uneasiness, or ill feeling
Causes
Herpetic gingivostomatitis is an infection caused by the herpes simplex virus (HSV). The HSV is a double-stranded DNA virus categorised into two types; HSV-1 and HSV-2. HSV-1 is predominantly responsible for oral, facial and ocular infections whereas HSV-2 is responsible for most genital and cutaneous lower herpetic lesions. Both HSV-1, and HSV-2 can be the cause of herpetic gingivostomatitis, although HSV-1 is the source of infection in around 90% of cases.
Pathophysiology
Herpetic gingivostomatitis originates from a primary infection of HSV-1. The series of events that take place during this infection include replication of the herpes simplex virus, cell lysis and finally, destruction of the mucosal tissue.
HSV-1 can very easily enter and replicate within epidermal and dermal cells through skin or mucosal surfaces which have abrasions. This results in numerous small vesicles or blisters of up to 1-2m…
Diagnosis
The histological appearance of a herpetic infection on the mucosa includes degeneration of stratified squamous epithelial cells, the loss of intercellular connections and inflammatory infiltrate around the capillaries of the dermis layer. An intact herpetic vesicle presents as an intraepithelial blister histologically. This vesicle is caused by rupture and distension of the virally epithelial cells by intracellular oedema and coalescence of disrupted cells.
Treatment
The aim of treatment is mostly supportive such as pain control, duration of symptoms, viral shedding and in some cases, preventing outbreak. Antibiotics are rarely prescribed to treat bacterial superinfection of oral lesions. Antiviral drugs are used to treat herpetic gingivostomatitis such as aciclovir, valaciclovir, famciclovir, and in resistance cases foscarnet can be used. Treatment does not prevent recurrence. Most individuals who are immunocompetent will fully recover from …
See also
• Acute necrotizing ulcerative gingivitis
External links
• Underlying Causes at wrongdiagnosis.com
• CDC Case Definition: Mercury (Elemental)
What Is It?
- Herpetic Gingivostomatitis (HG) is a contagious mouth infection that generally marks a child’s first exposure to the herpes simplex virus. The risk of contracting (HG) can be increased by poor oral hygiene such as not brushing enough or efficiently. HG is a very uncomfortable infection, especially for little ones, as it causes blisters to occur, ge...
How Will It Affect My Child?
- Herpetic Gingivostomatitis is a painful experience for little ones and can make parents frantic as well. One of the main side effects of the infection is that it makes it very uncomfortable for children to eat and drink. Therefore, those affected become very irritable because they’re hungry and can become dehydrated from lack of fluids as well. You might also notice swelling around t…
How Should It Be Treated?
- There isn’t a cure for Herpetic Gingivostomatitis or a magic potion to make it go away. Mostly, parents can take steps to address the symptoms of the infection and perhaps speed up the recovery a bit. Anti-viral drugs like acyclovir, which has a good record of treating herpes simplex-related viruses, might be prescribed for the child. Oral rinses and analgesics can be offered to h…
Can I Catch Herpetic Gingivostomatitis?
- Herpetic Gingivostomatitis is contagious and it’s easy for children to pass it to one another if they’re prone to doing things like sharing food, drinks, and utensils with each other. Kissing can also prompt spread of the infection. Because little ones often put toys in their mouths, the sharing of these playthings should be off limits during any outbreak as well. Most cases of Herpetic Gin…