
Does hypoglycemia cause coma?
Severe hypoglycemia and coma. Severe hypoglycemia (very low blood glucose levels) can lead to loss of consciousness and coma if not treated. In most cases the body will restore blood sugar levels to normal by releasing glucagon to raise blood sugar levels.
Can hyperglycemia cause a diabetic coma?
It's important to treat hyperglycemia, because if left untreated, hyperglycemia can become severe and lead to serious complications requiring emergency care, such as a diabetic coma. In the long term, persistent hyperglycemia, even if not severe, can lead to complications affecting your eyes, kidneys, nerves and heart.
What does hyperglycemic hyperosmolar nonketotic coma mean?
What is hyperosmolar hyperglycemic nonketotic coma? Hyperosmolar Hyperglycemic Nonketotic Syndrome (HHNS), also known as Hyperosmolar Hyperglycaemic State (HHS) is a dangerous condition resulting from very high blood glucose levels. HHNS can affect both types of diabetics, yet it usually occurs amongst people with type 2 diabetes.
What is a hyperosmolar nonketotic hyperglycemic coma?
Hyperglycemic hyperosmolar nonketotic syndrome (HHNS) is a potentially deadly condition that can develop as a result of infection or illness in people with uncontrolled type 2 diabetes or when diabetes medications aren't taken as directed. Some also refer to this as a "diabetic coma."
What happens during a hypoglycemic coma?
If you have diabetes, dangerously high blood sugar (hyperglycemia) or dangerously low blood sugar (hypoglycemia) can lead to a diabetic coma. If you lapse into a diabetic coma, you're alive — but you can't awaken or respond purposefully to sights, sounds or other types of stimulation.
What is the difference between hypoglycemic coma and diabetic coma?
You're most likely to get hypoglycemia if you skip a meal after injecting insulin or if you take too much insulin. Diabetic comas happen when you don't take steps to fix blood sugar that's too high or too low.
How is hypoglycemia coma treated?
Intravenous fluids to restore water to your tissues. Potassium, sodium or phosphate supplements to help your cells function correctly. Insulin to help your tissues absorb the glucose in your blood.
What causes hyperglycemic coma?
A diabetic hyperosmolar coma is caused by severe dehydration and very high blood glucose levels (hyperglycaemia). Events that can lead to high blood glucose levels include: forgotten diabetes medications or insulin. an infection or illness, such as the flu or pneumonia.
What happens to the brain during hypoglycemia?
Hypoglycemia commonly causes brain fuel deprivation, resulting in functional brain failure, which can be corrected by raising plasma glucose concentrations. Rarely, profound hypoglycemia causes brain death that is not the result of fuel deprivation per se.
What is the lowest blood sugar level before coma?
Things to know about this condition include: It could happen with a blood sugar as low as 250 mg/dL or even lower in some cases....What are the causes of diabetes-related coma?Your blood sugar could be as high as 600 mg/dL.Your urine won't contain ketones usually.Your blood will be much thicker than normal.
Is hypoglycemic coma reversible?
In milder cases, hypoglycemic symptoms are quickly reversed by oral or intravenous glucose. In some cases, however, coma may persist despite restitution of normoglycemia, for reasons that are not clear. In general, complete recovery is the rule, even after an hour or more of coma.
What blood sugar level will put you in a coma?
A diabetic coma could happen when your blood sugar gets too high -- 600 milligrams per deciliter (mg/dL) or more -- causing you to become very dehydrated.
How long does it take to recover from hypoglycemia?
It will usually take around 15 minutes to recover from a mild episode of hypoglycaemia. If you have a blood glucose meter, measure your blood sugar again after 15 to 20 minutes.
Can a person recover from a diabetic coma?
If the symptoms occurred for a while before treatment or if you were in a diabetic coma for several hours or longer, you could experience some brain damage. An untreated diabetic coma may also result in death. People who receive emergency treatment for a diabetic coma usually recover fully.
How do you know when a diabetic is dying?
weight loss. fatigue. numbness in fingers/toes. wounds that are slow to heal.
What happens when your blood sugar drops to 30?
If blood glucose drops really low, the person is not able to function because physical and mental changes occur. They can have seizures or become unconscious. Hypoglycemia is the medical term used when the amount of glucose (sugar) in someone's blood is lower than 70 mg/dL, with symptoms and signs noted above.
Symptoms
Hypoglycemic coma develops in stages. At first, there are precursor symptoms, indicating a decrease in the concentration of glucose in the blood. These include:
Diagnostics
Diagnosis of hypoglycemic coma is carried out on the basis of anamnesis and clinical picture of the disease. The diagnosis is confirmed by a biochemical blood test. A hypoglycemic state is indicated by a decrease in glucose concentration to a level of less than 3.5 mmol / l. Symptoms of a coma appear when glucose levels are less than 2.77 mmol / L.
Treatment
Therapy for hypoglycemic coma begins with intravenous administration of hypertonic glucose solutions. With a deep coma, glucagon or hydrocortisone is additionally injected intramuscularly. To improve glucose metabolism, the use of ascorbic acid and cocarboxylase is shown.
Possible complications and consequences
Hypoglycemic coma is often accompanied by the development of complications, both current and distant. Current complications arise in parallel with the hypoglycemic state and accompany it. These can be myocardial infarction, stroke, aphasia.
Forecast
With timely assistance, a hypoglycemic coma quickly stops and does not entail serious consequences for the body. In this case, the prognosis is favorable. However, often occurring hypoglycemic conditions lead over time to the development of serious cerebral disorders.
Prevention
To prevent hypoglycemia, the prescribed dosage of insulin or sugar-reducing drugs should be carefully followed. Patients should be informed about the need for a mandatory meal after the injection of insulin. Compliance with the daily regimen and diet helps reduce the risk of a drop in blood glucose concentration.
Abscess - Symptoms, Treatment, Autopsy, Removal, Diagnosis, Causes
An abscess is a purulent fusion of tissue. The cause of the disease is pyogenic microflora. Its treatment is carried out by a surgeon (dissection, removal with a capsule)
What is hypoglycemic coma?
Hypoglycemic coma is a type of diabetic coma, which usually results out of acute complications of diabetes. A diabetic coma can also occur due to hyperglycemia (too much of glucose in blood). Excessive amount of blood glucose leads to loss of unusual amounts of fluid (excessive urination), which may also result in hyperosmolar coma.
How to treat a coma?
Primary treatment involves giving an injection or administering intravenous form of hormonal medicine called glucagon. This helps restore the blood sugar levels quickly. The prognosis may vary according to the cause of coma, and the possibility to correct the particular situation.
What is the condition where blood sugar drops below normal levels?
This article discusses the causes and symptoms regarding the same. Hypoglycemia is a condition, wherein the blood sugar drops below the normal level. If this condition is left untreated, it may result in seizures and coma. Hypoglycemic coma is a type of diabetic coma, which usually results out of acute complications of diabetes.
Why does my body absorb glucose?
Causes. Severe hypoglycemia or untreated diabetes. Excessive alcohol intake. Skipping meals or severe mismanagement of food and liquid intake, for prolonged period. An insulin overdose can drop the blood glucose levels abnormally and quickly. As a result, the cells tend to absorb all available glucose and leave none for the brain.
What are the symptoms of low blood sugar?
Symptoms like nervousness, sweating, intense hunger, trembling, weakness, palpitations, and difficulty in speaking are easily recognizable. However, many symptoms of low blood sugar are similar to those observed in other ...
How does the body respond to low glucose levels?
The body responds to the low glucose levels, by beginning to shut down its functionality. It starts by destroying the neurons in the brain , which could cause loss of memory or function.
Is blood sugar bad for the brain?
Therefore, fluctuations in blood sugar levels can prove to be harmful for the brain.
What are the symptoms of a coma?
Symptoms include an increase in thirst and polyuria, general ill health, nausea, vomiting, drowsiness, and eventually coma. Clinically, the patient is often febrile, with evidence of dehydration (thin, rapid pulse, postural hypotension).
What is the task of the physician in first contact with the patient in metabolic coma?
The task of the physician in first contact with the patient in metabolic coma is to preserve and protect the brain from permanent damage. Metabolic and toxicologic studies must be performed on the first blood drawn (see Box 62-1 ). Treatable conditions that quickly and irreversibly damage the brain are discussed next.
What is the most serious metabolic emergency associated with type 1 diabetes?
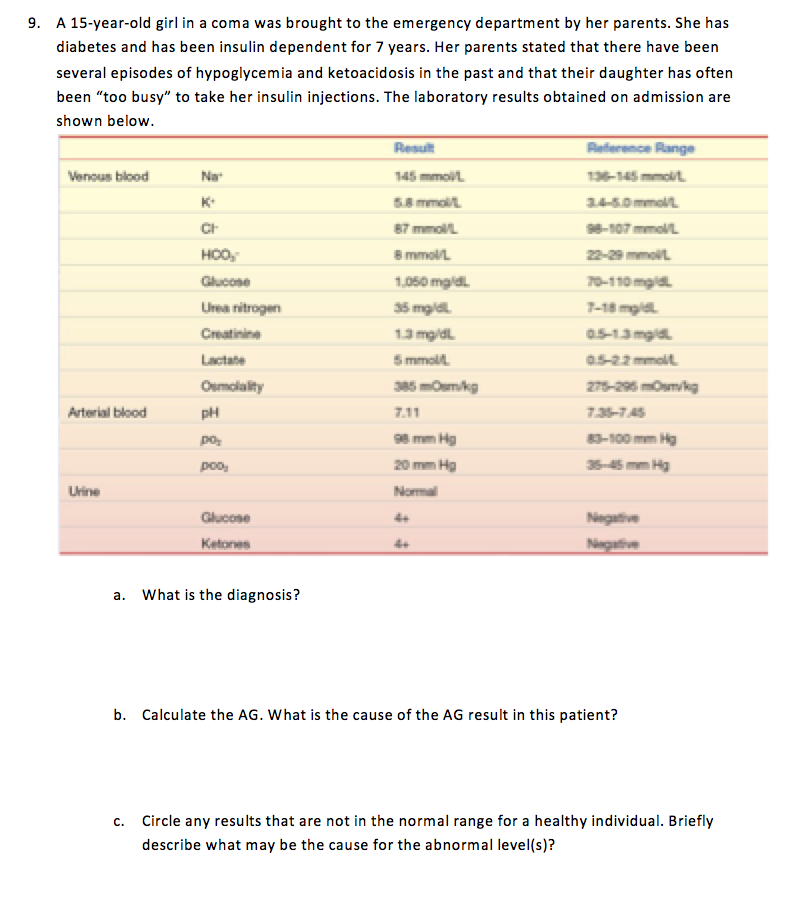
DKA is the most serious metabolic emergency associated with type 1 diabetes. It is the largest single cause of death in young diabetics and, although uncommon in older patients, when it does occur, it has a very high mortality in this age group. The fundamental cause is either absolute insulin deficiency or, less commonly, relative deficiency associated with an acute physiological stress, in association with increased secretion of counterregulatory catabolic hormones. The resultant metabolic effects consist of the following:
Can insulin overdose cause brain damage?
Patients having committed or undergone insulin overdose usually suffer from irreversible brain damage following deep hypoglycemia . Imaging studies of hypoglycemia in humans are obtained mostly from patients in hypoglycemic coma but rarely from patients with reversible focal neurological deficit. Cerebral hypoglycemic insult prominently affects the gray matter. Neurochemical changes in hypoglycemia significantly impair protein synthesis in many cerebral areas, with failure of ionic or energetic homeostasis, intracellular influx of calcium, and extracellular release of neuroactive amino acids. Excessive amounts of excitatory amino acids result in selective neuronal cell necrosis, prominently in the cortex, striatum, and hippocampus. Other structures, like the cerebellum, brainstem, and hypothalamus, have demonstrated resistance to hypoglycemia in a rat experimental model. CT examinations at the acute stage are often unremarkable. Depending on the severity and duration of hypoglycemia, decreased x-ray attenuation restricted to basal ganglia may be observed. Diffuse edematous swelling of brain parenchyma occurs in the most severe cases. In the chronic stage, CT findings of diffuse brain atrophy and subsequent enlargement of the ventricular system remain nonspecific. MRI studies have confirmed the preferential localization of the lesions to deep and cortical gray matter. After a delay of 7 to 14 days following the onset of the hypoglycemic coma, a strong bilateral T2 -hyperintensity and faint T 1 -hypointensity due to increases in free water content are commonly observed within the caudate and lenticular nuclei, cerebral cortex, substantia nigra, and hippocampus ( Figure 19-8 ). 45,46 The thalami are usually spared for unknown reasons. A possible explanation could be that hypoglycemia induces less severe energy failure than does ischemia. At the acute stage, increased T 2 -signal intensity within gray matter may be observed on both FLAIR and diffusion-weighted images. Decreased ADC values in the injured areas are then obtained. 47–49 Thus far, diffusion-weighted imaging detects changes in water diffusivity not only resulting from oxygen deprivation, but also resulting from other metabolic changes. Like what happens in hypoglycemia, the diffusion-weighted hypersignal intensity reflecting decrease in water diffusivity and subsequently decrease in apparent diffusion coefficient (ADC) values due to cytotoxic edema with loss of transmembrane ionic homeostatis due to the failure of ATPase-dependant pumps, cell swelling, and interstitial space volume restriction. However, the topographical distribution and the temporal evolution of hypoglycemic brain damage differ from that due to anoxia or ischemia. Monitoring of ADC changes can demonstrate the evolution from cell swelling with restricted water diffusivity at the acute stage to cell death with abnormally increased ADC values at chronic stages. A series of patients with reversible focal neurological deficits due to transient hypoglycemia has been investigated by diffusion-weighted imaging. 50–53 Transiently hyperintense lesions were seen bilaterally in internal capsules, in the corona radiate, and in the splenium of the corpus callosum. In conclusion, transient or definitive lesions can be observed using the different MRI techniques, according to the severity and duration of the hypoglycemia. The lesions are seen within cerebral cortex, hippocampus, and basal ganglia and are not specific to hypoglycemia. Differential diagnosis mainly includes ischemic injuries.
Can insulin cause a coma?
Hypoglycemia may occur in a large number of different conditions , but excessive doses of insulin for the treatment of diabetes are the most common cause of severe hypoglycemic coma. In addition, patients with early diabetes and diabetics with renal insufficiency may show spontaneous mild postprandial hypoglycemia,114 and both insulin and oral hypoglycemic agents may produce hypoglycemia of variable severity with a corresponding range of neurological symptoms and signs. Newer, rapidly acting insulin analogues have not had a significant effect on the rate of hypoglycemic episodes in diabetics. 115
Does insulin cause hypoglycemia?
Hypoglycemia occurs predominantly in patients taking insulin but also in patients taking sulfonylureas, particularly long-acting preparations such as chlorpropamide and glibenclamide. The factors which commonly predispose to hypoglycemia, either alone or in combination, are:
Is nonketotic hyperosmolar coma a presenting feature?
Nonketotic hyperosmolar coma only occurs in type 2 diabetes, sometimes as a presenting feature, and consists of gross hyperglycemia and dehydration but without ketosis and significant acidosis. The mechanism of this is uncertain. The condition develops more insidiously than DKA, allowing time for a greater degree of dehydration to develop. Treatment consists of fluid replacement and low-dose insulin therapy. The prognosis is poor, with a significant mortality especially in older patients.
Why does hypoglycemia happen?
Hypoglycemia occurs when your blood sugar (glucose) level falls too low. There are several reasons why this can happen; the most common is a side effect of drugs used to treat diabetes.
What causes hypoglycemia in the pancreas?
Other tumors also can result in too much production of insulin-like substances. Enlargement of cells of the pancreas that produce insulin can result in excessive insulin release, causing hypoglycemia.
What is the condition where blood sugar is low?
Hypoglycemia is a condition in which your blood sugar (glucose) level is lower than normal. Glucose is your body's main energy source. Hypoglycemia is often related to diabetes treatment. But other drugs and a variety of conditions — many rare — can cause low blood sugar in people who don't have diabetes. Hypoglycemia needs immediate treatment ...
Why is my glucose level dangerously high?
As a result, glucose tends to build up in the bloodstream and can reach dangerously high levels.
What happens when you have diabetes?
When this happens, the risk of severe, life-threatening hypoglycemia increases. If you have diabetes, recurring episodes of hypoglycemia and hypoglycemia unawareness, your doctor might modify your treatment, raise your blood sugar level goals and recommend blood glucose awareness training.
What are the symptoms of low blood sugar?
If blood sugar levels become too low, signs and symptoms can include: As hypoglycemia worsens, signs and symptoms can include: Confusion, abnormal behavior or both, such as the inability to complete routine tasks.
What is the recommended blood sugar level for hypoglycemia?
For many people, a fasting blood sugar of 70 milligrams per deciliter (mg/dL), or 3.9 millimoles per liter (mmol/L), or below should serve as an alert for hypoglycemia. But your numbers might be different.
What is hypoglycemia in medical terms?
Hypoglycemia is a clinical syndrome caused by a decrease in blood glucose and characterized by clinical signs of activation of the autonomic nervous system and neuroglycopenic symptoms. [ 1 ], [ 2 ], [ 3 ], [ 4 ], [ 5 ], [ 6 ], [ 7]
What causes a coma in diabetics?
The main factors provoking the development of hypoglycemia in diabetes mellitus: accidental or intentional overdose of insulin or BSSS;
What are the features of alcoholic hypoglycemia?
Features of the clinical picture of alcoholic hypoglycemia are the delayed nature of the occurrence and the probability of recurrences of hypoglycemia (due to suppression of gluconeogenesis in the liver), as well as frequent prevalence of neuroglycemia symptoms over autonomic symptoms.
What is the prevalence of hypoglycemia?
The exact prevalence of hypoglycemia is unknown, but hypoglycemic coma cause death of 3-4% of patients with diabetes mellitus.
How much sugar should I take for mild hypoglycemia?
For the treatment of mild hypoglycemia (consciousness is preserved), it is advisable to take inwardly digestible carbohydrates in an amount of 1.5-2 XE (for example, 200 ml of sweet fruit juice, 100 ml of pepsi-cola or phantoms, 4-5 slices of sugar-refined sugar).
What hormones are elevated with hypoglycemia?
With a glycemic level of 3.8 mmol / l, an increase in the secretion of the contrinsular hormones glucagon, epinephrine, growth hormone and cortisol is noted (the level of growth hormone and cortisol increases only with prolonged hypoglycemia).
Does glucagon decrease with neuropathy?
Later, reactive secretion of epinephrine decreases even in patients without autonomic neuropathy. Decreased secretion of glucagon and adrenaline hypoglycemia increases the risk of severe hypoglycemia.
What is a diabetic coma?
A diabetic coma is a life-threatening diabetes complication that causes unconsciousness. If you have diabetes, dangerously high blood sugar (hyperglycemia) or dangerously low blood sugar (hypoglycemia) can lead to a diabetic coma.
What to do if you pass out from a diabetic coma?
When to see a doctor. A diabetic coma is a medical emergency. If you feel extreme high or low blood sugar signs or symptoms and think you might pass out, call 911 or your local emergency number. If you're with someone with diabetes who has passed out, call for emergency help, and be sure to let the emergency personnel know ...
Why does insulin stop?
Insulin delivery can stop if the pump fails or the tubing (catheter) is twisted or falls out of place. A lack of insulin can lead to diabetic ketoacidosis. An illness, trauma or surgery. When you're sick or injured, blood sugar levels tend to rise, sometimes dramatically.
What happens if you don't monitor your blood sugar?
If you don't monitor your blood sugar properly or take your medications as directed, you'll have a higher risk of developing long-term complications and a diabetic coma. Deliberately skipping meals or insulin.
What is the name of the condition where blood sugar is low?
Low blood sugar (hypoglycemia) Signs and symptoms of a low blood sugar level may include: Some people, especially those who've had diabetes for a long time, develop a condition known as hypoglycemia unawareness and won't have the warning signs that signal a drop in blood sugar.
Can high blood sugar cause a coma?
Severely high blood sugar turns your blood thick and syrupy. The excess sugar passes from your blood into your urine, which triggers a filtering process that draws tremendous amounts of fluid from your body. Left untreated, this can lead to life-threatening dehydration and a diabetic coma. About 25 to 50 percent of people with diabetic hyperosmolar ...
Can diabetics have insulin?
Sometimes, people with diabetes who also have an eating disorder choose not to use their insulin as directed with the hope of losing weight. This is a dangerous, life-threatening practice that increases the risk of a diabetic coma. Drinking alcohol. Alcohol can have unpredictable effects on your blood sugar.

Hypoglycemic Coma
- The content of the article: 1. Causes and risk factors 2. Disease stages 3. Symptoms 4. Diagnostics 5. Treatment 6. Possible complications and consequences 7. Forecast 8. Prevention Hypoglycemic coma is an acute life-threatening condition caused by a sharp drop in the concentration of glucose in the blood; extreme hypoglycemia. Hypoglycemic coma oc...
Causes and Risk Factors
- The main causes of hypoglycemia are: 1. overdose of hypoglycemic drugs or insulin; 2. insufficient carbohydrate intake after the usual dose of insulin; 3. hypersensitivity to insulin; 4. decreased insulin-activating liver function; 5. hyperinsulinism; 6. alcohol intoxication. Much less often, the state of hypoglycemia is due to: 1. overdose of beta-blockers and aspirin; 2. chronic re…
Disease Stages
- There are several stages in the development of hypoglycemic coma: 1. Cork. It is associated with the development of hypoxia of cells of the cerebral cortex. 2. Subcortical-diencephalic. Increasing hypoglycemia leads to damage to the subcortical-diencephalic zone of the brain. 3. Precoma. It is caused by a violation of metabolic processes in the structure of the midbrain. 4. Coma itself. Th…
Symptoms
- Hypoglycemic coma develops in stages. At first, there are precursor symptoms, indicating a decrease in the concentration of glucose in the blood. These include: 1. anxiety, fear; 2. feeling of severe hunger; 3. profuse perspiration (hyperhidrosis); 4. dizziness and headache; 5. nausea; 6. sharp pallor of the skin; 7. hand tremor; 8. tachycardia; 9. increased blood pressure. If help is no…
Diagnostics
- Diagnosis of hypoglycemic coma is carried out on the basis of anamnesis and clinical picture of the disease. The diagnosis is confirmed by a biochemical blood test. A hypoglycemic state is indicated by a decrease in glucose concentration to a level of less than 3.5 mmol / l. Symptoms of a coma appear when glucose levels are less than 2.77 mmol / L. At a blood glucose concentrati…
Treatment
- Therapy for hypoglycemic coma begins with intravenous administration of hypertonic glucose solutions. With a deep coma, glucagon or hydrocortisone is additionally injected intramuscularly. To improve glucose metabolism, the use of ascorbic acid and cocarboxylase is shown. If a patient has signs of cerebral edema against the background of a hypoglycemic coma, then osmotic diur…
Possible Complications and Consequences
- Hypoglycemic coma is often accompanied by the development of complications, both current and distant. Current complications arise in parallel with the hypoglycemic state and accompany it. These can be myocardial infarction, stroke, aphasia. Long-term complications of hypoglycemic coma appear several days or even weeks after the acute condition. The most common complica…
Forecast
- With timely assistance, a hypoglycemic coma quickly stops and does not entail serious consequences for the body. In this case, the prognosis is favorable. However, often occurring hypoglycemic conditions lead over time to the development of serious cerebral disorders. In patients with diseases of the cardiovascular system, hypoglycemic coma is more severe and m…
Prevention
- To prevent hypoglycemia, the prescribed dosage of insulin or sugar-reducing drugs should be carefully followed. Patients should be informed about the need for a mandatory meal after the injection of insulin. Compliance with the daily regimen and diet helps reduce the risk of a drop in blood glucose concentration. Patients with diabetes mellitus and their loved ones should be awa…