Hypoproliferative anemia is the result of a deficiency of erythropoietin Erythropoietin, also known as haematopoietin or haemopoietin, is a glycoprotein cytokine secreted by the kidney in response to cellular hypoxia; it stimulates red blood cell production in the bone marrow. Low levels of EPO are constantly secreted sufficient to compensate for normal red blood ce…Erythropoietin
Normochromic anemia
Normochromic anemia is a form of anemia in which the concentration of hemoglobin in the red blood cells is within the standard range, but there is an insufficient number of red blood cells. Conditions where this is found include aplastic, posthemorrhagic, and hemolytic anemias and anemia of chronic disease.
Kidney
The kidneys are two bean-shaped organs found in vertebrates. They are located on the left and right in the retroperitoneal space, and in adult humans are about 11 centimetres in length. They receive blood from the paired renal arteries; blood exits into the paired renal veins. Each kidney is attached to a ureter, a tube that carries excreted urine to the bladder.
Which malignancies are associated with pernicious anemia?
Pernicious anemia (PA) is associated with an increased rate of secondary malignancies, which include cancer of the stomach (standardized incident rate (SIR) = 2.9), esophagus (SIR = 3.2), and pancreas (SIR = 1.7) among men and women; myeloid leukemia among men (SIR = 1.8-5.2); and multiple myeloma among women (SIR = 2.5) [5].
What are pernicious anemia symptoms?
What Is Pernicious Anemia?
- Pernicious Anemia Symptoms. Symptoms often come on gradually and are mild at first but may worsen if untreated. ...
- Causes. The most common cause of pernicious anemia is autoimmune gastritis leading to vitamin B12 deficiency.
- Diagnosis. ...
- Treatment. ...
- A Word From Verywell. ...
What are the effects of hyper-chromic anemia?
Some of the common symptoms associated with hypochromic anemia include: Weakness and generalized fatigue are common symptoms associated with this condition. ... The skin often looks pale and the nails become brittle and white. The heart rate increases to more than 100 beats per minute. ... Clinical depression is observed in some individuals associated with the disease. More items...
What are the treatments for iron deficiency anemia?
Treatment
- Iron deficiency anemia. Treatment for this form of anemia usually involves taking iron supplements and changing your diet. ...
- Vitamin deficiency anemias. ...
- Anemia of chronic disease. ...
- Aplastic anemia. ...
- Anemias associated with bone marrow disease. ...
- Hemolytic anemias. ...
- Sickle cell anemia. ...
- Thalassemia. ...
What is the most common Hypoproliferative anemia?
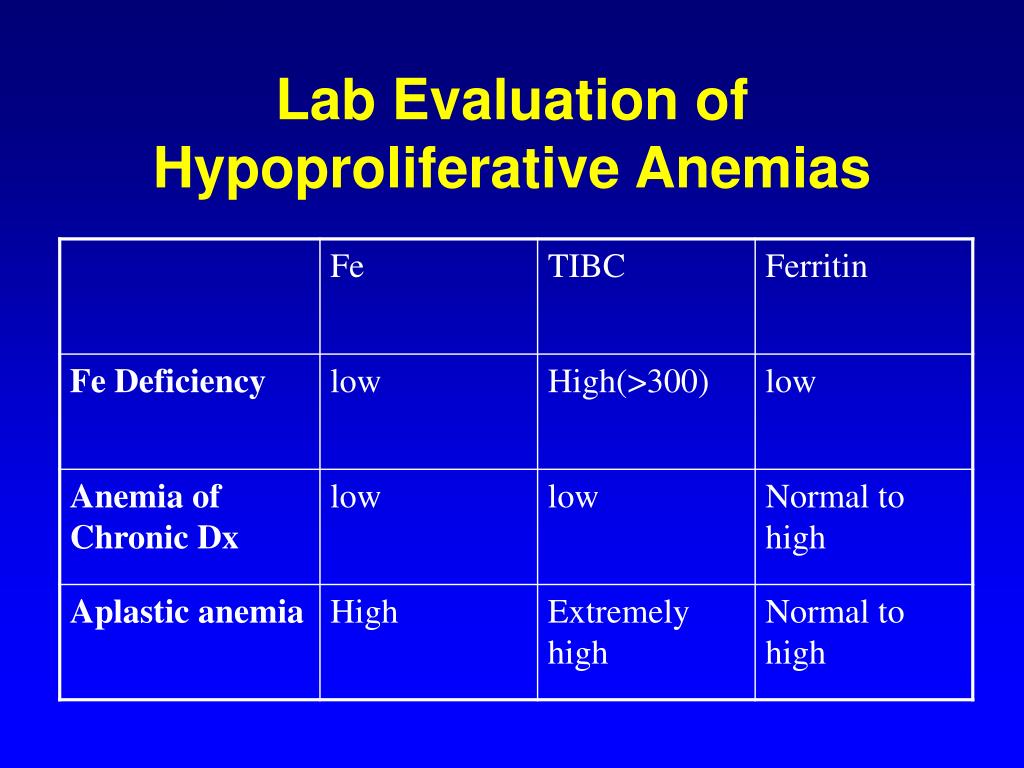
Iron deficiency is the most common hypoproliferative anemia, followed by anemia of chronic inflammation and renal disease.
What is the definition of Hypoproliferative?
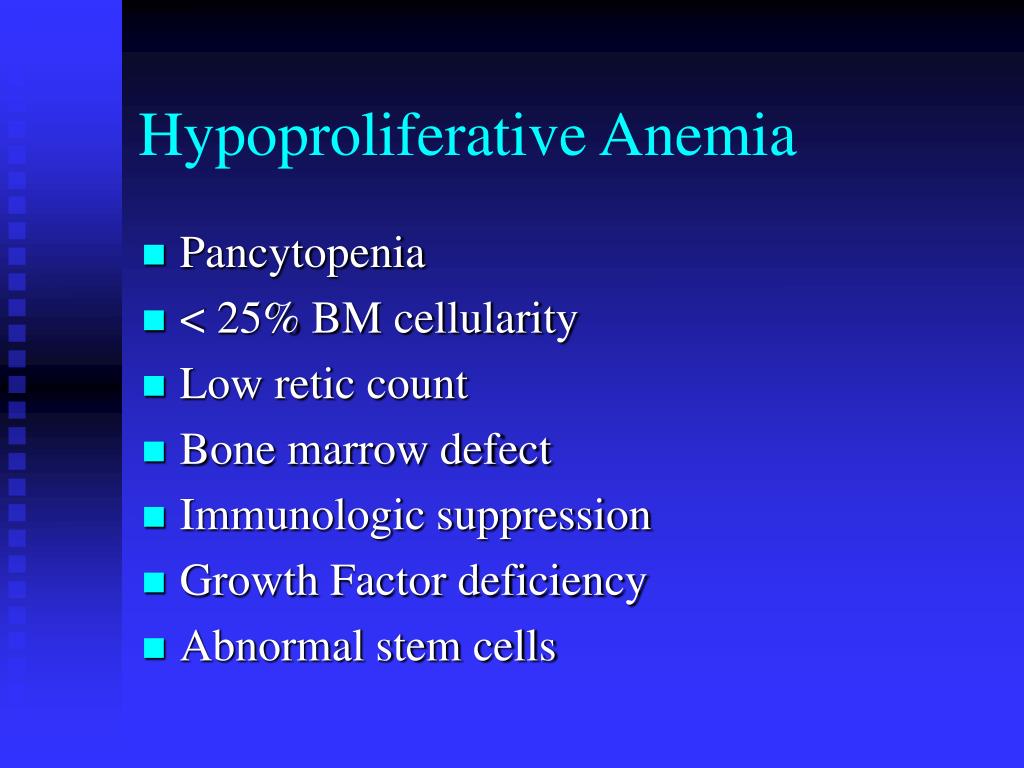
Hypo-proliferative anemia is an anemia where the bone marrow's response, the production of reticulocytes, is absolutely low, or low for the degree of anemia (Reticulocytopenia).
What are the 4 types of anemia?
Many types of anemia exist, such as iron-deficiency anemia, pernicious anemia, aplastic anemia, and hemo- lytic anemia. The different types of anemia are linked to various diseases and conditions.
Is thalassemia a Hypoproliferative anemia?
There is intense reticulocytosis, as evidenced by a large number of nucleated red blood cells in the peripheral blood. The thalassemias are hyperproductive anemias manifested by hemolysis occurring in the bone marrow compartment due to mispairing of beta and globin units.
How is Hypoproliferative anemia diagnosed?
The reticulocyte count, a marker of effective erythropoiesis, is the single blood test most important for distinguishing hypoproliferative anemia from other causes (Figure 1).
Is Sickle cell Hypoproliferative anemia?
Anemia in SCD is chronic and hemolytic in nature. This results in a hyperproliferative anemia.
What are 3 symptoms of anemia?
SymptomsFatigue.Weakness.Pale or yellowish skin.Irregular heartbeats.Shortness of breath.Dizziness or lightheadedness.Chest pain.Cold hands and feet.More items...•
What are the 7 types of anemia?
In this ArticleAplastic (or Hypoplastic) Anemia.Sideroblastic Anemia.Myelodysplastic Syndromes.Autoimmune Hemolytic Anemia.Congenital Dyserythropoietic Anemia (CDA)Diamond-Blackfan Anemia.Megaloblastic Anemia.Fanconi Anemia.
What organ is affected by anemia?
Severe anemia can cause low oxygen levels in vital organs such as the heart, and can lead to heart failure.
What are the 4 types of thalassemia?
Alpha thalassemia occurs when some or all of the 4 genes that make hemoglobin (the alpha-globin genes) are missing or damaged....There are 4 types of alpha thalassemia:Alpha thalassemia silent carrier. ... Alpha thalassemia carrier. ... Hemoglobin H disease. ... Alpha thalassemia major.
What is the difference between alpha thalassemia and beta thalassemia?
The thalassemias are a group of inherited hematologic disorders caused by defects in the synthesis of one or more of the hemoglobin chains. Alpha thalassemia is caused by reduced or absent synthesis of alpha globin chains, and beta thalassemia is caused by reduced or absent synthesis of beta globin chains.
How long do thalassemia patients live?
Survival of thalassemia patients The cumulative survival rate from birth until 10 years old was 99%. After reaching the age of 20 years, 88% of the patients survived until 30 years, 74% survived until 45, 68% survived until 50, and 51% survived until 55 years old.
What is hypoproliferative anemia?
Hypo-proliferative anemia is an anemia where the bone marrow’s response, the production of reticulocytes, is absolutely low, or low for the degree of anemia (Reticulocytopenia). It is possible to have a hemolytic anemia or blood loss (a ‘hyper-proliferative anemia”) simultaneously, in which case the hemoglobin level will fall more rapidly.
What is the most common error in approaching anemias?
The most common error in approaching anemias is to think of all the causes that come to mind and try to fit one to the situation. Forgetting uncommon diagnoses, missing simultaneous multiple etiologies or simply being overwhelmed by the possibilities are all common outcomes. Fortunately, the evaluation of anemia lends itself to a systematic approach.
Why is thalassemia obvious?
Thalassemia is usually obvious because of the normal iron studies and chronic microcytosis with or without anemia. Rarely, with hematologic malignancy, you can see acquired thalassemia.
What causes macrocytic anemia?
A good history will help evaluate the most common causes of macrocytic anemia. Liver disease (which should also be showing other manifestations-hypoalbuminemia, transaminitis, thrombocytopenia) and alcohol (ETOH) use (which may be quite occult – “only an occasional glass of wine” confirmed by the family is common in patients who will later be seen to be significant ETOH users). A trial of complete abstinence from Alcohol may resolve macrocytosis during follow up labs. It is often worth repeating full history and review of all medications since often patients will forget them because they think of them as rheumatologic/GI or dermatologic drugs.
What happens if your reticulocyte count is low?
If the reticulocyte count is inappropriately low then the bone marrow production of red blood cells (RBCs) is inadequate. Bone marrow failures can be segregated by red cell size – the mean cellular volume (MCV). The MCV is tightly regulated and even modest variation of this commonly ignored lab result is of clinical significance.
What are megaloblastic changes?
Megaloblastic changes suggesting B12, folate. Early changes of iron deficiency (although lab testing will be more valuable) Target cells and round macrocytes suggesting liver disease. Changes suggesting myelodysplasia, especially since the bone marrow may be non-diagnostic in up to 50% of patients initially.
Is reticulocyte count elevated?
The reticulocyte count may be elevated, consistent with a shortened red cell survival (e.g. autoimmune hemolytic anemia) but not as elevated as one would expect (e.g. due to the underlying lymphoma causing the hemolysis). Hyperproliferative anemias is discussed in a separate section.
What causes anemia in the kidneys?
In short, a low kidney function with a creatinine clearance of below 45 ml per minute, leads to an emia because EPO production decreases. Two disease processes that lead to severe anemia are amyloidosis and diabetic nephropathy. In addition protein deficiency and general starvation can also lead to hypoproliferative anemia.
Why is erythropoietin not produced?
This normocytic normochromic anemia develops when erythropoietin (=EPO) is not produced enough by the kidney tissue and as a result the bone marrow does not get enough stimulus from the EPO hormone to produce enough red blood cells. To clarify, the most common causes for this is kidney failure. This can be brought about from kidney diseases ...
How long does it take for iron to increase RBC?
In addition the physician prescribes iron supplements. After 8 to 12 weeks the patient reaches the maximum response in terms of increasing the RBC level. Maintenance doses are about half of the induction doses.Meanwhile many patients do not require transfusions.
Which cytokines contribute to hypoproliferative anemia?
The most extensively studied cytokines--tumor necrosis factor-[alpha], interleukin 1, interleukin 6 , and interferon--contribute to hypoproliferative anemiaeither by altering the sensitivity of erythroid precursors to Epoetin alfa or by stimulating the production of proinflammatory proteins such as C-reactive protein (CRP), fibrinogen, and serum amyloid A and decreasing levels of albumin and transferrin (Gunnell, Yeun, Depner, & Kaysen, 1999).
What is anemia of chronic disease?
Anemia of chronic disease (ACD), also known as anemia of inflammation, is a hypoproliferative anemiathat develops in response to systemic illness or inflammation such as infection, cancer, and autoimmune conditions.
What is the primary cause of anemia seen in patients with CKD?
The primary cause of anemia seen in patients with CKD is from hypoproliferative anemia( Barrett et al., 1999; Ly, Marticorena, & Donelly, 2004).
What is renal failure?
Renal failure is often associated with a decreased erythropoietin output resulting in hypoproliferative anemia. In addition, a moderate degree of hemolysis and blood loss by various means plays an important role in decreasing red cell mass, which the bone marrow is unable to restore to normal.
What causes microcytic hypochromic anemia?
Microcytic, hypochromic anemia can be caused by lead toxicity , chronic disease, thalassemia and hemoglobin E disorder. Iron deficiency is the most common cause of microcytic, hypochromic anemia. Ferritin blood levels are a measure of the body's stores of iron and are usually low in iron deficiency anemia.
What is central anemia?
Anemia of central origin, or hypoproliferative anemia, broadly refers to anemia resulting from underproduction of red blood cells by the bone marrow.
What is anemia of central origin?
Anemia of central origin, or hypoproliferative anemia, broadly refers to anemia resulting from underproduction of red blood cells by the bone marrow. Furthermore, is reticulocyte count high in iron deficiency anemia? Hemolytic anemia: Your reticulocyte count is high.
What is normochromic anemia?
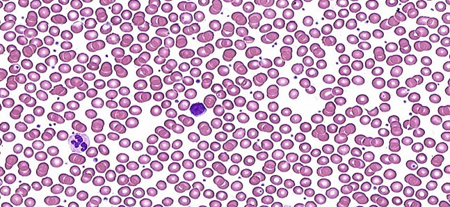
Normocytic normochromic anemia is the type of anemia in which the circulating RBCs are the same size (normocytic) and have a normal red color (normochromic). Most of the normochromic, normocytic anemias are a consequence of other diseases; a minority reflects a primary disorder of the blood.
What is the function of RBCs in anemia?
The main function of RBCs, or erythrocytes, is to carry oxygen from the lungs to the body tissues and carbon dioxide as a waste product from the body tissues to the lungs back.
How to tell if you have normocytic normochromic anemia?
A physical exam may help confirm the diagnosis. The first signs of normocytic normochromic anemia or any type of anemia are usually generalized weakness and a pale complexion.
How does normochromic anemia differ from other forms of anemia?
Normocytic normochromic anemia differs from other forms of anemia because the average size and hemoglobin content of the RBCs are typically within normal limits. RBCs typically appear similar to normal cells under microscopic examination, though in some cases, there may be variations in size and shape that equalize one another, resulting in average values within the normal range. Normocytic normochromic anemia most commonly occurs as a result of miscellaneous chronic infections and systemic diseases. Most normocytic anemias appear to be the outcome of the impaired production of RBCs. [5]
Why is RBC survival reduced?
The RBC survival is usually not markedly shortened, and marrow function should compensate for the reduced survival. In hemolytic anemias, the etiology of premature erythrocyte destruction is diverse and can be due to conditions such as intrinsic membrane defects, abnormal hemoglobin, erythrocyte enzymatic defects, immune destruction of erythrocytes, mechanical injury, and hypersplenism. Hemolysis may also be intramedullary, occurring in cases when fragile red blood cell (RBC) precursors are destroyed in the bone marrow before their release into the circulation.[15] Bone marrow changes also lead to physical obstruction and destruction of the bone marrow microenvironment.
What happens when the number of RBCs decreases?
A decrease in the number of RBCs transporting oxygen and carbon dioxide in anemia decreases the body’s capacity for proper gas exchange. The impairment may result from blood loss, an increase in the destruction, or reduced production of RBCs.
What is the impairment of RBCs?
The impairment may result from blood loss, an increase in the destruction, or reduced production of RBCs. Traditionally, the decrease is quantified by the ratio of packed RBCs to blood volume, called hematocrit and hemoglobin concentration.[1][2] . Anemia is a condition marked by a decrease in the number of red blood cell (RBC) mass in the blood.
I. Problem/Condition.
- Hypo-proliferative anemia is an anemia where the bone marrow’s response, the production of reticulocytes, is absolutely low, or low for the degree of anemia (Reticulocytopenia). It is possible to have a hemolytic anemia or blood loss (a ‘hyper-proliferative anemia”) simultaneously, in which case the hemoglobin level will fall more rapidly.
A. How to Approach A hypo-proliferative Anemia
- The most common error in approaching anemias is to think of all the causes that come to mind and try to fit one to the situation. Forgetting uncommon diagnoses, missing simultaneous multiple etiologies or simply being overwhelmed by the possibilities are all common outcomes. Fortunately, the evaluation of anemia lends itself to a systematic approach. Anemias are either h…
B. Diagnostic Approach to hypo-proliferative Anemias
- Particularly in patients with a severe anemia, a normal MCV may reflect a combined macrocytic and microcytic process. This is most likely iron deficiency or thalassemia. A quick review of patient’s hemoglobin and MCV can guide further workup when differentiating between thalassemia or iron deficiency as a cause of microcytic anemia. In iron deficiency, the MCV falls …
A. Management of Hypoproliferative Anemia
- The details of managing each specific diagnosis are discussed in separate sections. If the patient is unstable, at risk or the rate of fall of the hemoglobin is rapid, then the patient should be admitted and transfused. Most information can be retrieved after the transfusion but it is very helpful to obtain a direct Coombs, iron study, B12 study, lactate dehydrogenase (LDH) and a peri…