Cardioplegic Solution is a sterile, nonpyrogenic, essentially isotonic, formulation of electrolytes in water for injection. It is a "core solution" intended for use only after addition of sodium bicarbonate to adjust pH prior to administration.
What are the components of cardioplegia?
[1] Cardioplegia varies by composition, delivery methods, temperature, and additives; however, all solutions must include potassium chloride (15-35 meq/L) important for inducing cardiac arrest, and other electrolytes such as Mg2+, low-dose Ca2+, Cl-. Na+.
What's cardioplegic solution?
Solution. Cardioplegia Solution A is a sterile, non-pyrogenic solution for cardiac perfusion in a Viaflex bag. It is used to induce cardiac stasis and to protect the myocardium during open-heart surgery.
What are cardioplegic drugs?
DESCRIPTION. Cardioplegic Solution is a sterile, nonpyrogenic, essentially isotonic, formulation of electrolytes in water for injection. It is a "core solution" intended for use only after addition of sodium bicarbonate to adjust pH prior to administration.
How do you prepare a cardioplegia solution?
It is required that 10 mL (840 mg) of 8.4% Sodium Bicarbonate Injection, USP (10 mEq each of sodium and bicarbonate) be added aseptically and thoroughly mixed with each 1000 mL of cardioplegic solution to adjust pH.
Why potassium is used in cardioplegia?
Chemically, the high potassium concentration present in most cardioplegic solutions decreases the membrane resting potential of cardiac cells.
Why does cardioplegia stop the heart?
These voltage-gated channels are targeted with cardioplegia to induce cardiac arrest. The persistence of potassium reduces the membrane potential and does not allow for adequate repolarization. This, in turn, creating a diastolic cardiac arrest.
Where is cardioplegia injected?
Anterograde cardioplegia is administered into a small cannula placed in the ascending aorta or directly into the coronary ostia. Retrograde cardioplegia is delivered through a catheter placed through the right atrium into the coronary sinus. Cardioplegia is then delivered into the venous system of the heart.
Who invented cardioplegia?
The term cardioplegia (cardio, heart and plegia, paralysis) was first introduced by Lam in 1957 (Lam et al., 1957), yet the method of arrest has its roots in the early experiments of British physiologist Sidney Ringer using the frog heart (Figure 2).
How do doctors induce cardioplegia for open-heart surgery?
Hyperkalemic, hypothermic solutions are frequently used to induce cardioplegic arrest and protect the heart during cardiac surgery involving CPB.
What is St Thomas solution?
St. Thomas solution is an extracellular, potassium-based cardioplegia solution that can be administered as a crystalloid solution or combined with a blood component. At the time, the addition of magnesium was unique to St. Thomas solution.
What is del Nido cardioplegia?
Del Nido cardioplegic solution (DNC), a blood-and-crystalloid solution, is used as a single-dose antegrade infusion to induce rapid cardiac arrest and provide at least 90 minutes of myocardial protection in neonatal heart surgery.
What is buckberg cardioplegia?
Modified Buckberg cardioplegia is a dextrose-based solution in normal saline with potassium chloride as the depolarizing agent, tromethamine as the buffer, and citrate phosphate double dextrose as a calcium chelator and delivered 4:1 oxygenated patient's blood to crystalloid.
How do you give cardioplegia?
Anterograde cardioplegia is administered into a small cannula placed in the ascending aorta or directly into the coronary ostia. Retrograde cardioplegia is delivered through a catheter placed through the right atrium into the coronary sinus. Cardioplegia is then delivered into the venous system of the heart.
What is blood cardioplegia?
The warm blood cardioplegia technique is a promising strategy in the ever-expanding field of myocardial protection. Continous WBC provides variable protection against ischemia by eliminating hypothermic myocardial ischemia and reperfusion injury.
What is Vasoplegia?
Vasoplegia is characterized by a normal or augmented cardiac output with low systemic vascular resistance (SVR) causing organ hypoperfusion.
What is Baxter Cardioplegic Solution?
Baxter Cardioplegic Solution is a sterile, nonpyrogenic, essentially isotonic, formulation of electrolytes in Water for Injection, USP. It is a “core solution” intended for use only after addition of sodium bicarbonate to adjust pH prior to administration. After buffering with sodium bicarbonate it is suitable for cardiac instillation ...
What is the purpose of sodium bicarbonate in cardioplegic solution?
Cardioplegic Solution with added sodium bicarbonate when cooled and instilled into the coronary artery vasculature, causes prompt arrest of cardiac electromechanical activity, combats intracellular ion losses and buffers ischemic acidosis. When used with hypothermia and ischemia, the action may be characterized as cold ischemic potassium-induced cardioplegia.
Why is sodium important in myocardial fluid?
Sodium is essential to maintain ionic integrity of myocardial tissue. The chloride ions are present to maintain the electroneutrality of the solution. Added bicarbonate (HCO 3-) anion is included as a buffer to render the solution slightly alkaline and compensate for the metabolic acidosis that accompanies ischemia.
How to protect pharmaceutical products from heat?
Exposure of pharmaceutical products to heat should be minimized. Avoid excessive heat. Protect from freezing. It is recommended that the product be stored at room temperature (25°C); however, brief exposure up to 40°C does not adversely affect the product.
How much solution is instilled during bypass?
Development of severe hypotension and metabolic acidosis while on bypass has been reported when large volumes (8 to 10 liters) of solution are instilled and allowed to enter the pump and then the systemic circulation. Right heart venting is therefore recommended.
Can you instill a cardiac solution into the heart?
Do not instill the solution into the coronary vasculature unless sodium bicarbonate has been added. If large volumes of Cardioplegic solution are infused and allowed to return to the heart lung machine without any venting from the right heart, then plasma magnesium and potassium levels may rise.
What are the chemical components of cardioplegia?
Chemical components added to the cardioplegia solution, such as potassium and glucose, are largely responsible for this protective effect. Basic characteristics of cardioplegia solutions include temperature, osmolarity, and pH.
What is the role of pharmacist in cardioplegia?
The pharmacist's role in the formulation, preparation, and quality control of cardioplegia solution is also discussed. The use of cardioplegia solution has substantially increased the safety of cardiac surgery.
How does a syringe protect the myocardium?
It protects the myocardium by inducing a rapid and complete diastolic arrest, minimizing myocardial energy requirements and preventing ischemic damage during the arrest phase, and minimizing or preventing reperfusion injury once coronary blood flow is restored.
What is the best solution for cardioplegia?
A global survey sent to Europe, Australia/New Zealand, North and South America regarding cardioplegia use and practices during cardiac surgery and found a wide variety in responses confirming there is no clear consensus on best practices regarding cardioplegia use.[1] Cardioplegia varies by composition, delivery methods, temperature, and additives; however, all solutions must include potassium chloride (15-35 meq/L) important for inducing cardiac arrest , and other electrolytes such as Mg2+, low-dose Ca2+, Cl-. Na+.[14] Bicarbonate is added just prior to administration to ensure its integrity and to adjust the pH of the solution as needed.
What is cardioplegia in surgery?
Cardioplegia serves to intentionally and temporarily arrest the heart for myocardial protection during cardiac surgery. This activity describes cardioplegia as well as outlines the various components and delivery methods and highlights the role of the interprofessional team in managing patients who require cardioplegia.
What is cardioplegia in aortic bypass?
Cardioplegia is an essential component in myocardial protection during aortic cross-clamping and cardiopulmonary bypass. A good understand of the various compositions of cardioplegia, routes of administration, and potential side effects are necessary to reduce morbidity and mortality in patients undergoing cardiac surgery. Inadequate administration may result in permanent reperfusion injury and myocardial ischemia.
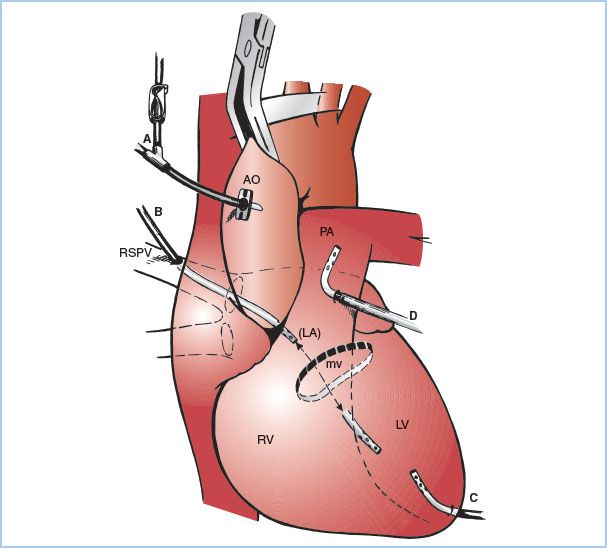
What is anterograde cardioplegia?
Cardioplegia administration can be anterograde, retrograde, or both. The anterograde cardioplegia is inserted in the proximal aorta and contains three lumens: one to administer the cardioplegia, another for suctioning, and the third to measure intraluminal pressure.[4] Barometric monitoring of cardioplegia administration is required to prevent potential endothelial cell damage and reperfusion injury secondary to elevated infusion pressures.[5] The patient is heparinized, cooled, and, when appropriate, is placed on cardiopulmonary bypass. The aortic cross-clamp is placed just distal to the anterograde cardioplegia cannula, and once secured, the perfusionist can begin administering cardioplegia at set doses and intervals as requested by the cardiothoracic surgeon.[4] Anterograde simply means that the solution runs down the right and left coronary arteries and supplies the myocardium in the same distribution that blood would normally.
What is the role of a perfusionist in cardioplegia?
The perfusionist is the main individual responsible for delivering cardioplegia by keeping track of the flow rate, volume, temperature, components, and timing of each dose. There is an important interplay between the cardiothoracic surgeon and perfusionist just prior, during, and coming off of bypass. The perfusionist also assesses and controls the intraluminal pressure through which the cardioplegia solution is being administered and alters the flow rate, volume, temperature, and pressure accordingly.[13] The cardiothoracic anesthesiologist will assist in confirming the position of the retrograde cardioplegia catheter placed by the cardiothoracic surgeon on TEE and also facilitates the assessment of the atherosclerosis of the ascending aorta for clamping and cannulation.
What happens to the heart after aortic crossclamping?
Cardioplegia following aortic cross-clamping results in many physiological changes that may hinder the recovery of the myocardium. It is essential to understand the electrolyte abnormalities, myocardial stunning, pH imbalance that may occur secondary to cardioplegia administration. Before coming off cardiopulmonary bypass, electrolytes, temperature, glucose, pH, hemoglobin, and hematocrit must be within normal limits. Excessive physiological changes may result in myocardial stunning, arrhythmias, ischemic injury leading to the inability to wean from cardiopulmonary bypass. Prophylactic measures are taken to reduce the complications of cardioplegia, such as frequent blood sampling by the perfusionist and notifying the surgeon and anesthesiologist of derangements while treating abnormalities as they present.
What is a variant of microplegia?
A variant known as microplegia is a concentrated version using whole blood cardioplegia
What is the Baxter Cardioplegia Solution A?
Sodium chloride, potassium chloride, calcium chloride dihydrate and magnesium chloride hexahydrate. 2 Qualitative and Quantitative Composition. Baxter Cardioplegia Solution A is a sterile, non-pyrogenic solution in a Viaflex bag. It is used to induce cardiac stasis and to protect the myocardium during open-heart surgery.
How long does it take to mix Baxter Cardioplegia?
It should be cooled to 4°C before use. Once mixed, the solution should be used within 24 hours. It should not be used in serial connections with other containers.
What is immunoglobulin therapy?
Immunoglobulin (Ig) products provide critical therapy for people with immunodeficiencies and immune-type neurological conditions.
What happens to potassium in cardioplegic solution?
Chemically, the high potassium concentration present in most cardioplegic solutions decreases the membrane resting potential of cardiac cells. The normal resting potential of ventricular myocytes is about -90 mV. When extracellular cardioplegia displaces blood surrounding myocytes, the membrane voltage becomes less negative and the cell depolarizes more readily. The depolarization causes contraction, intracellular calcium is sequestered by the sarcoplasmic reticulum via ATP-dependent Ca 2+ pumps, and the cell relaxes (diastole). However, the high potassium concentration of the cardioplegia extracellular prevents repolarization. The resting potential on ventricular myocardium is about −84 mV at an extracellular K + concentration of 5.4 mmol/l. Raising the K + concentration to 16.2 mmol/l raises the resting potential to −60 mV, a level at which muscle fibers are inexcitable to ordinary stimuli. When the resting potential approaches −50 mV, sodium channels are inactivated, resulting in a diastolic arrest of cardiac activity. Membrane inactivation gates, or h Na + gates, are voltage dependent. The less negative the membrane voltage, the more h gates that tend to close. If partial depolarization is produced by a gradual process such as elevating the level of extracellular K +, then the gates have ample time to close and thereby inactivate some of the Na + channels. When the cell is partially depolarized, many of the Na + channels are already inactivated, and only a fraction of these channels is available to conduct the inward Na + current during phase 0 depolarization.
What does cardioplegia mean?
Overview. The word cardioplegia combines the Greek cardio meaning the "heart", and plegia "paralysis". Technically, this means arresting or stopping the heart so that surgical procedures can be done in a still and bloodless field. Most commonly, however, the word cardioplegia refers to the solution used to bring about asystole of the heart, ...
What is a temporary cessation of cardiac activity?
Cardioplegia is intentional and temporary cessation of cardiac activity, primarily for cardiac surgery .
What is antegrade cardioplegia?
This is further augmented by the cardioplegia component which is high in potassium. When solution is introduced into the aortic root (with an aortic cross-clamp on the distal aorta to limit systemic circulation), this is called antegrade cardioplegia.
What does cold fluid do to the heart?
The cold fluid (usually at 4 °C) ensures that the heart cools down to a temperature of around 15–20 °C, thus slowing down the metabolism of the heart and thereby preventing damage to the heart muscle. This is further augmented by the cardioplegia component which is high in potassium.
What cations can be used to arrest the heart?
The use of two other cations, Na + and Ca 2+, also can be used to arrest the heart. By removing extracellular Na + from perfusate, the heart will not beat because the action potential is dependent upon extracellular Na + ions. However, the removal of Na + does not alter the resting membrane potential of the cell.
Does cardioplegia cause asystole?
As the cardioplegia solution distributes to the entire myocardium, the ECG will change and eventually asystole will ensue. Cardioplegia lowers the metabolic rate of the heart muscle, thereby preventing cell death during the ischemic period of time.
What are the components of cardioplegia?
Components of cardioplegia solution are varied in different institutions but include potassium to achieve diastolic arrest. A cross-clamp is applied to the ascending aorta, and the cardioplegia is administered into the aortic root in an antegrade fashion via the coronary ostia.
How is cardioplegia delivered?
Cardioplegia is delivered under pressure to the heart via either a pressurized bag or a roller pump system. The advantages of roller pump system include easy incorporation of a continuous cooling system to maintain cardioplegia hypothermia, easy incorporation of the mixing apparatus necessary for blood cardioplegia systems, ...
What are the disadvantages of hypothermic cardioplegia?
The other disadvantages of hypothermic cardioplegia, in addition to the production of the metabolic inhibition in the myocardium, are an increase in plasma viscosity and a decrease in red blood cell deformability. As a result, investigations aimed at using warmer cardioplegia temperatures have been explored.
What is the temperature of myocardial solution?
The composition of cardioplegia solutions varies considerably; in contrast, myocardial temperature during cardioplegia is almost uniformly reduced to between 10°C and 12°C or less by the infusion of refrigerated cardioplegia and external topical cooling with ice slush.
Why do we need a pump for cardioplegia?
Cardioplegia must be delivered accurately to prevent myocardial damage, and new pump delivery systems provide a better operator-interface for effective delivery .
What temperature is used for cardioplegia?
Although hypothermic cardioplegia is the most commonly used temperature, numerous investigations have examined tepid (27–30°C) and warm (37–38°C) temperature ranges for the administration of cardioplegia.
Which loop is used to pull the right atrial appendage inferiorly?
Alternatively, and preferentially, retrograde cardioplegia cannulation is omitted, and the right atrial appendage is retracted with a no. 2 silk loop. This loop is tunneled through the utility port and pulls the right atrial appendage inferiorly to improve visualization of the aortic root (Figs. 10.5 and 10.6 ).
cardioplegia
arrest of myocardial contraction, as by use of chemical compounds or cold in cardiac surgery. adj., adj cardiopleg´ic.
cardioplegia
Deliberate temporary stopping of the heart beat (contractions) in the course of heart surgery, either by cooling or by means of drugs.
Why is cardioplegia red?
Dark blue blood initially drains from the coronary sinus during antegrade administration, but then becomes red because oxygenated flow exceeds energy needs. Conversely, when following retrograde administration is started, the coronary ostial effluent is blue and subsequently becomes red. This implies that some capillaries were not perfused during antegrade delivery.
What are the goals of cardiac surgery?
Two goals of a cardiac surgical procedure are technical excellence and protection of cardiac function. Cardioplegia is used, almost universally, to provide the quiet bloodless field that is critical for surgical precision. Stepwise methodological strategies are used to correct anatomic defects. Their technical success is gauged by return ...
How does warm blood cardioplegia affect metabolism?
Conversely, warm blood cardioplegia enhances metabolism and replenishes depleted substrates in injured hearts during induction [ 5 ], and offsets reperfusion injury before aortic unclamping [ 6 ].
What is the best marker for myocardial damage?
Ventricular septal function is the best marker for determining myocardial damage, as the septum occupies ∼35–40% of the total ventricular muscle mass and 50% of the left ventricular (LV) mass [ 14] (Fig. 2 a and b). It is observable by routine intraoperative echocardiography. The septum is formed by helical fibres (Fig. 3) and produces 80% of RV function due to shortening and twisting [ 16 ]. Septal function is measured by the classical normal, slight or severe hypokinesia, akinesia or dyskinesia (paradoxical) motion. Recently, tricuspid annular plane systolic excursion (TAPSE) and its systolic excursion velocity (‘ S ’) is recommended for routine use by the American Society of Echocardiography and European Association Echocardiography [ 16 ].
What is the pre-ejection mitral valve?
Pre-ejection mitral or tricuspid valve insufficiency is secondary complication of septum damage because its paradoxical motion towards the right side tethers the posterior papillary muscle to change leaflet coaptation. Bulging towards the left side tethers the septum papillary muscle and causes tricuspid regurgitation. The importance of a midline septum position is emphasized, since biventricular pacing will move the septum into the midline to prevent mitral insufficiency, but it does not restore twisting.
Where are the muscular mass components separated from the heart?
The lower tracings show that the muscular mass components after the right ventricle (RV), septum and left ventricle are separated from the intact heart via incisions made along the septum adjacent to the left anterior and right posterior descending vessels.
Is warm reperfusion good for cardioplegia?
It has averted damage after ischaemia of the leg S4, brain [ 10 ], lung [ 11] and liver S5, and is widely used as the ‘warm reperfusion or ‘hot shot’ in cardiac surgery [ 12 ]. Teoh and Weisel independently showed accelerated myocardial metabolic and functional recovery [ 13 ]. Warm reperfusion has reversed cardiac damage following sudden death, despite ∼72 min (22–150 min) of CPR [ 14 ]. The warm reperfusate is a very powerful tool against reperfusion damage, and our recent clinical study shows that functional injury develops when the integrated strategy of myocardial protection is not followed [ 15 ].

Description
Clinical Pharmacology
- Cardioplegic Solution with added sodium bicarbonate when cooled and instilled into the coronary artery vasculature, causes prompt arrest of cardiac electromechanical activity, combats intracellular ion losses and buffers ischemic acidosis. When used with hypothermia and ischemia, the action may be characterized as cold ischemic potassium-induced cardioplegia. This is cond…
Indications and Usage
- Cardioplegic Solution when suitably buffered in combination with ischemia and hypothermia is used to induce cardiac arrest during open heart surgery.
Contraindications
- Cardioplegic Solution must not be administered without the addition of 8.4% Sodium Bicarbonate Injection, USP. NOT FOR INTRAVENOUS INJECTION. This solution is only for instillation into cardiac vasculature after buffering with sodium bicarbonate.
Warnings
- This solution should be used only by those trained to perform open heart surgery. This solution is intended only for use during cardiopulmonary bypass when the coronary circulation is isolated from the systemic circulation (See INDICATIONS AND USAGE). Do not instill the solution into the coronary vasculature unless sodium bicarbonate has been added. If large volumes of Cardiople…
Precautions
- Myocardial temperature should be monitored during surgery to maintain hypothermia. Continuous electrocardiogram monitoring is essential to detect changes in myocardial activity during the procedure. Appropriate equipment to defibrillate the heart following cardioplegia should be readily available. Inotropic support drugs should be available during postoperative recovery. Do not ad…
Adverse Reactions
- Intraoperative and perioperative potential hazards of open heart surgery include myocardial infarction, electrocardiographic abnormalities, and arrhythmias, including ventricular fibrillation. Spontaneous recovery after Cardioplegic cardiac arrest may be delayed or absent when circulation is restored. Defibrillation by electric shock may be required to restore normal cardiac …
Overdosage
- Overzealous instillation of the solution may result in unnecessary dilatation of the myocardial vasculature and leakage into the perivascular myocardium, possibly causing tissue edema (See WARNINGS, PRECAUTIONS, and ADVERSE REACTIONS).
Dosage and Administration
- The following information is suggested as a guide and is subject to variation according to the preference and experience of the surgeon. It is required that 10 mL (840 mg) of 8.4% Sodium Bicarbonate Injection, USP (10 mEq each of sodium and bicarbonate) be added aseptically and thoroughly mixed with each 1000 mL of Cardioplegic solution to adjust pH. Use 10 mL of 8.4% S…
Instructions For Use
- Flexible Plastic Container (freeflex® bag) Do not remove solution container from its overwrap until immediately before use. The intact port cap provides visual tamper evidence. Do not use if port cap is prematurely removed. Maintain strict aseptic technique during handling. To Open 1. Always inspect the solution container before and after removal from the overwrap. 2. Place the s…