What is the difference between intertubular and peritubular dentin?
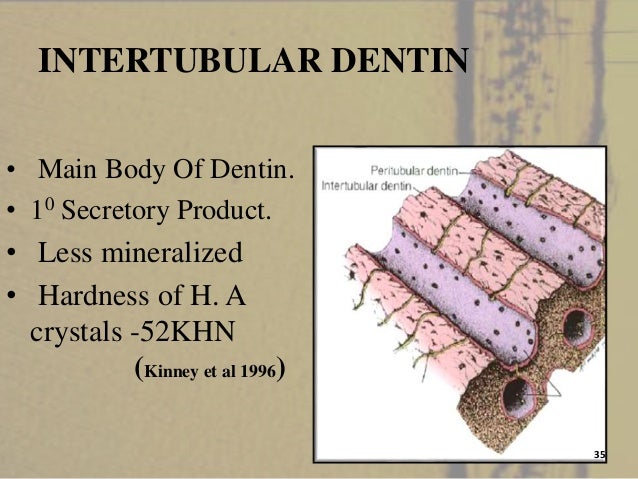
Differences in the structure and composition of the two dentins are well documented. Type I collagen is the major protein of intertubular dentin (90%), whereas no collagen fibrils are observed in the peritubular dentin. Differences have been also reported in the composition of non-collagenous proteins of the two dentins [15–18]. Along these lines, some crystallo-chemical specificities of the inter- and peri-tubular dentins have been established.
What are intertubular crystallites?
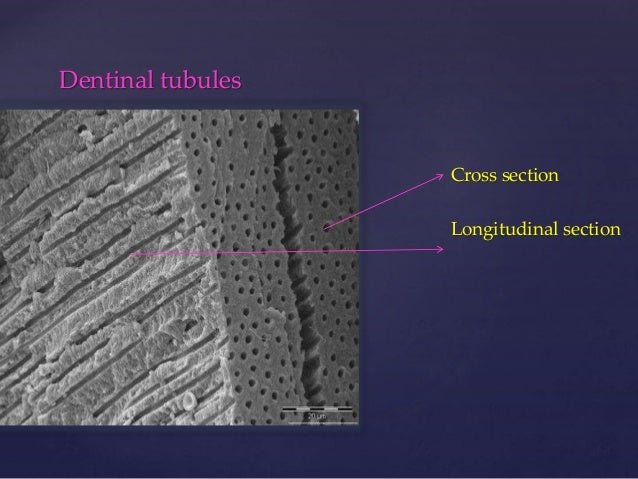
In intertubular dentin, s form the plate-like crystallites, 2–5 nm in thickness and 60nm in length. At lowermagnification, inter-tubular crystallites have a needle like appearance. They are located either at the surface the collagen fibrils, and parallel withthe collagen fibril axis; the crystallites randomly fill interfibrillar spaces [19]. Demineralization of intertubular dentin reveals a dense network of collagen fibrils, coated by non-collagenous proteins. Glycosaminoglycans as stained by cationic dyes are associated with the collagen hole zones resulting from the overlapping of collagen subunits. In the peri-tubular dentin, isodiametric structures about 25nm in diameter have been reported [15, 20]. At higher resolution, the crystals are bearing the following measurements: a= 36nm, b=25nm and c= 9.75nm [21]. They form a ring around the lumen of the tubules. After mild demineralization no collagen fibrils are detectable, but a thin network of non-collagenous proteins and phospholipids are visible [15, 18, 19].
What is the largest part of the dentin layer?
The circumpulpal dentin forms the largest part of the dentin layer. Thin at initial stages of dentinogenesis, its thickness continuously increases (about 4mm/day) at the expense of the space initially occupied by the pulp. Again, it is not a homogeneous dentin layer. The most prominent part of the circumpulpal dentin is formed by intertubular dentin, whereas peritubular dentinis found around the lumen of the tubules,. The ratio between inter-tubular and peri-tubular dentin is highly species dependant. Peritubular dentin is missing in the continuously growing rodent incisors. In contrast, in horses, the ratio is roughly 50%, and decreases in humans (about 10–20%), with huge variations depending on the area where the calculations are made.
How long does it take for a band to form in an odontoblast?
After 24 hours , the labeling is very weak in odontoblasts, firmly reduced in predentin and then only an accumulation of silver grains is seen forming a dense band 10–20 micrometers in widthat the mineralization front in the inner dentin side [34]. Later, the band is covered by the dentin newly formed during the next 48h and more, which is not labeled. This labeling is stable and remains even after longer periods of time. There is no translocation of the labeled band, at constant distance from the dentino-enamel junction.
How do odontoblasts form dentin?
During odontogenesis, odontoblasts are critical for the formation of a primary dentin, until the tooth becomes functional. When contacts between antagonistic cusps are established, then the formation of secondary dentinstarts immediately, and continues throughout life. Initially, odontoblasts constantly produce matrix molecules that result in the formation of a 10 micrometers thick layer, reduced afterward to a daily 4 micrometers deposit. However, there is not much difference between primary and secondary dentin. The only major difference is morphological, and the S-curve of the tubules is more accentuated in the secondary dentin, due to the gradual space restriction of odontoblasts, located at the periphery of a withdrawing pulp.
What is the thick layer of dental tissue?
A thick dentin layer forms the bulk of dental mineralized dental tissues. Dentin is capped by a crown made of highly mineralized and protective enamel, and in the root, it is covered by cementum, a structure implicated in the attachment of the teeth to the bony socket. Teeth contain in their central parts dental pulps, which are usually non-mineralized. This soft connective tissue also contains nerves and a vascular network connected with the surrounding tissues, the periodontal ligament and the bony socket. Taken as a whole, the general composition of dentin is summarized in Table 1.
What is the mantle dentin?
In the crown, the so-called mantle dentin, indentation measurements using Vickers microhardness show a gradual increase in hardness along the outer 200mm [7]. This outer layer is less mineralized and consequently the resilient mantle dentin may be adapted for dissipating pressures or forces which otherwise would induce enamel fissures and detachment of the fragmented enamel from the outer dentin-enamel junction. Dentin tubules are missing or reduced in number and bent in these layers of outer dentin. For some years, there was a debate about the observation that when using the “stains all” staining method [8] or antibodies raised against dentin phosphoproteins [9] the mantle dentin was unstained in contrast with the circumpulpal dentin, and consequently Takagi and Sasaki suggested that this layer was deprived of phosphorylated proteins [8]. However, chemical analysis revealed that proteins usually phosphorylated are actually present but in an underphosphorylated form or not phosphorylated at all [10]. In this context it is interesting to note that the mantle dentin is unaffected in X-linked hypophosphatemia [11] whereas in contrast rickets produces within the circumpulpal dentin enlarged non-mineralized interglobular spaces containing dentin ECM molecules [12]. Hence, the nature of the NCP’s differs between the mantle and circumpulpal dentins, the outer layer being not influenced by the organic phosphorous status. As a consequence, in the crown, the outer layers are less mineralized than the rest of the dentin. They display some elastic properties and therefore provide some resilience, important from a mechanical point of view and allowing dissipation of stress forces [7]. However, the thickness of the outer layer is about 200mm, therefore larger than the presumed width of the mantle dentin.