How do you find the IVC on an ultrasound?
May start with subxyphoid view, place right atrium in center of screen and rotate probe 90 degrees clockwise to find IVC A bedside IVC ultrasound was performed to assess volume status in setting of dehydration. The IVC was identified in longitudinal access. The IVC was neither flat nor plethoric.
What does IVC mean on a ventilator?
IVC, inferior vena cava. The quality of evidence to determine volume responsiveness with IVC changes is less clear in patients who are triggering the ventilator or spontaneously breathing, and the accuracy of the 12–18% cutoffs is unknown.
Is IVC measurement by ultrasound reliable in patients with hypovolemia?
Though controversial, IVC measurement by ultrasound can estimate volume status, fluid responsiveness, and fluid tolerance There is evidence to support that IVC diameter is consistently low in hypovolemia versus euvolemia. IVC change can estimate fluid responsiveness with a Sn 0.78 and Sp 0.86.
Why is the IVC important in Emergency Imaging?
The IVC can be particularly important in emergency imaging, with two entities requiring immediate recognition and treatment: slitlike IVC and aortocaval fistula (Fig 17). A slitlike IVC is defined as an IVC with a transverse-to-anteroposterior diameter ratio greater than 3:1 that is seen at multiple levels.
What does IVC mean on ultrasound?
inferior vena cavaIntroduction. Intravascular volume status is an important clinical consideration in the management of the critically ill. Point-of-care ultrasonography (POCUS) has gained popularity as a non-invasive means of intravascular volume assessment via examination of the inferior vena cava (IVC).
What is normal IVC size?
Inferior vena cava (IVC) is normally 1.5 to 2.5 cm in diameter (measured 3 cm from right atrium) IVC <1 cm in Trauma is associated with a high likelihood of Hemorrhage requiring Blood Transfusion. IVC <1.5 cm suggests volume depletion.
What does IVC measure?
Measuring the diameter of the inferior vena cava (IVC) by ultrasonography is a fast, non-invasive tool for assessment of the blood volumetric status of critically ill patients in the early stages of care [25–27].
Why do we check IVC?
IVC - inferior vena cava. International recommendations(17,18) suggest that the IVC be assessed to estimate the pressure in the right atrium of nonventilated patients because of its collapsibility during inspiration.
What does normal IVC mean?
The normal IVC diameter is less than 1.7 cm and there is a 50% decrease in the diameter when the RA pressure is normal (0–5 mm Hg). • A dilated IVC (>1.7 cm) with normal inspiratory collapse (>50%) is suggestive of a mildly elevated RA pressure (6–10 mm Hg).
What does an enlarged IVC mean?
We propose that in healthy subjects (without volume overload, pericardial disease, and right heart abnormalities), dilated IVC may be a marker of decreased abdominal venous tone and/or increased compliance. This may lead to exaggerated abdominal venous pooling during standing and subsequently orthostatic symptoms.
What is normal IVC size on Echo?
Normal IVC diameter was measured both during inspiration and expiration by M-mode echocardiography in subcostal view. Results: The IVC diameter varied from 0.46 to 2.26cm in the study individuals. The IVC diameter ranged from 0.97 to 2.26cm during expiration and from 0.46 to 1.54cm during inspiration.
What is normal IVC collapse?
Under normal circumstances, the IVC diameter is less than 20 millimeters (mm) with a collapse of more than 50% during inspiration [4]. In cases of increased RA pressures, the collapsibility is diminished.
What are some indications for evaluating the IVC with ultrasound?
IndicationsDifferentiate causes of shock.Differentiate causes of shortness of breath.Establish likelihood of fluid responsiveness.Assess response to interventions.
Is IVC collapse serious?
Conclusion: A dilated IVC without collapse with inspiration is associated with worse survival in men independent of a history of heart failure, other comorbidities, ventricular function, and pulmonary artery pressure.
What causes IVC to collapse?
A high degree of sonographically-visualised collapse of the inferior vena cava (IVC) during inspiration suggests a volume-responsive cardiac output. This inspiratory collapse is said to be due to a fall in intra-thoracic pressure.
What is IVC syndrome?
Inferior vena cava syndrome (IVCS) is a sequence of signs and symptoms that refers to obstruction or compression of the inferior vena cava (IVC). The pathophysiology of IVCS is similar to superior vena cava syndrome (SVCS) because of the presence of an underlying process that inhibits venous return to the right atrium.
What is normal IVC collapse?
Under normal circumstances, the IVC diameter is less than 20 millimeters (mm) with a collapse of more than 50% during inspiration [4]. In cases of increased RA pressures, the collapsibility is diminished.
What is normal IVC Collapsibility?
The IVC collapsibility index was 30 percent. CVP is a standard of care for evaluating the fluid status in the PICU, and it is still commonly used in critical pediatric patients(15). It reflects the right ventricular filling pressure, and provides information about the intravascular volume(28).
What is normal IVC pressure?
Current American Society of Echocardiography (ASE) recommendations [6] state that IVC diameter ≤ 2.1 cm that collapses >50% with a sniff suggests normal RA pressure (RAP, range 0–5 mmHg), whereas IVC diameter > 2.1 cm that collapses <50% suggests high RAP (range 10–20 mmHg).
What is IVC on heart echo?
The inferior vena cava (IVC) diameter as measured by echocardiography can be affected by tumour masses, respiration, and right atrial (RA) pressure. The IVC has been studied in patients with congestive heart failure and particularly in patients with right-sided cardiovascular disease or pericardial disease.
What is the importance of IVC ultrasound?
Ultrasound evaluation of the IVC can deliver important information on a patient's volume status. As a non-invasive, fast technique POCUS of the IVC has gained means in the assessment of fluid status in critically ill patients. Even in the diagnosis of heart failure IVC ultrasound plays a role. According to the latest ASE guidelines the assessment of the IVC in a subcostal view should be part of every routine transthoracic echocardiographic examination. Measurements should be performed in a subcostal long axis view perpendicular to the IVC with the patient in a supine position at 1.0 to 2.0 cm from the junction with the right atrium.
What causes the IVC diameter to fluctuate?
We therefore get the maximum and minimum IVC diameter. These fluctuations in size of the IVC are caused by negative intrathoracic pressure during inspiration which leads to an increase of RV (right ventricular) filling of the systemic veins. We therefore get the minimum IVC diameter during inspiration.
Can IVC be dilated without collapse?
Note that normal, young athletes may have a dilated IVC with normal pressure. In patients on ventilators the IVC may be commonly dilated without appropriate collapse due to normal respiration . In these cases IVC is not recommended to routinely be used to assess RA pressure according to latest guidelines. Although the measurement of the IVC with TEE had led to a successful measurement of central venous pressure even in ventilated patients. When estimating pulmonary artery pressure with the tricuspid regurgitant jet velocity, individual RA pressures should be added by performing the above listed measurements of the IVC.
What is the IVC?
Structurally, the IVC is a thin-walled, highly compliant vessel. Its size and dynamics vary with respiration and changes in intravascular volume. The development of negative intrathoracic pressure during inspiration increases the venous blood return from the extrathoracic veins into the right heart. This leads to an increase in the blood flow through the IVC and a subsequent decrease in its blood volume, resulting in a reduction in intraluminal pressure. These changes decrease the diameter of the IVC during inspiration relative to expiration. These observations are reversed with positive pressure ventilation in which IVC diameter increases during inspiration.
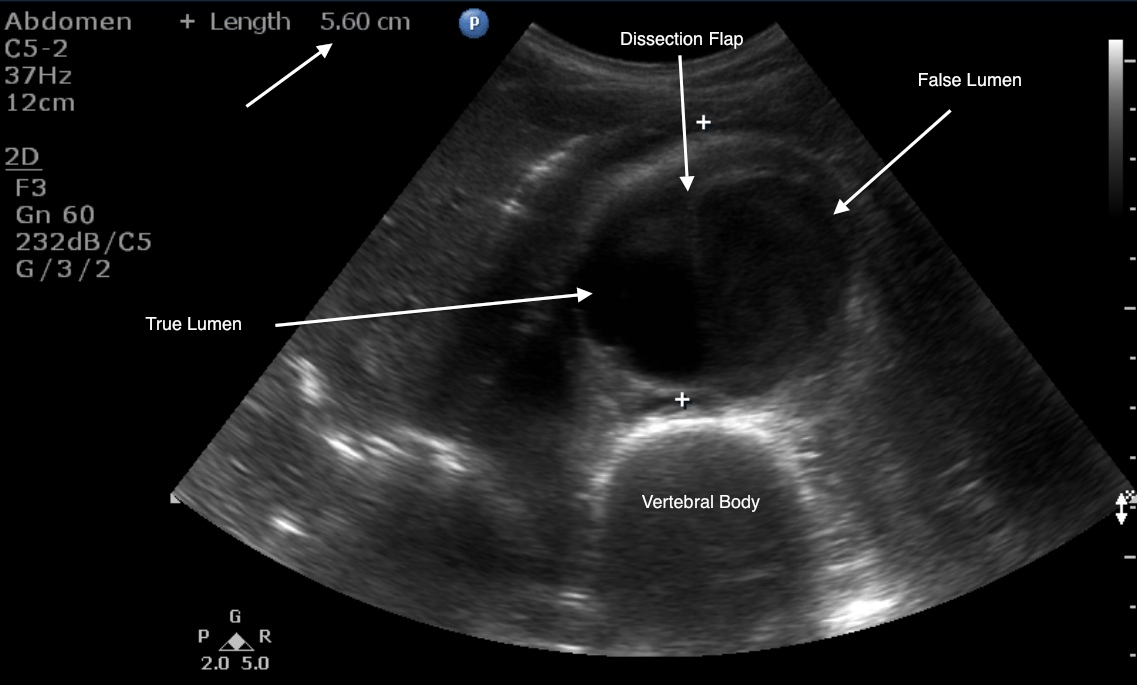
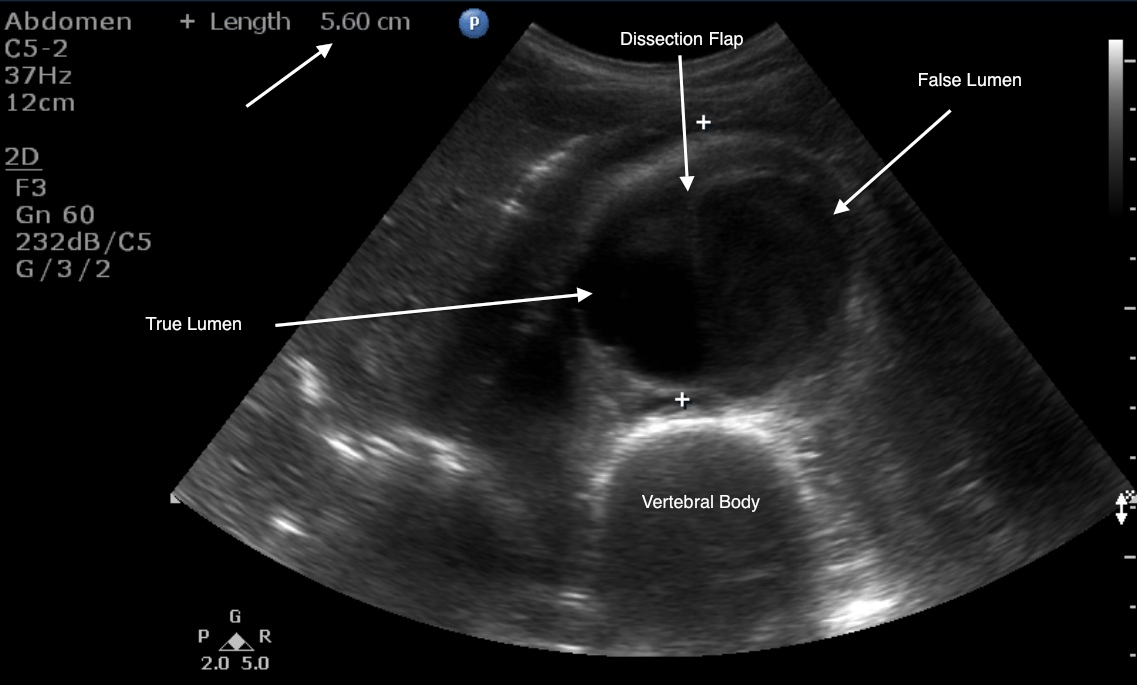
How to view IVC?
The IVC can be visualized in a transverse (short-axis) or in a sagittal (long-axis) orientation while scanning the abdomen. Imaging is performed with the patient in a supine position using the liver as an acoustic window. It is recommended to begin with a transverse view, with the probe indicator to the patient’s right side just below the xiphoid process. In this orientation, the vertebral body of the spine is seen as a bright hyperechoic structure with posterior shadowing. The aorta is seen in cross section just anterior to the spine as an anechoic blood-filled circular structure. The IVC is seen adjacent to the aorta on the patient’s right side as an anechoic circular or teardrop structure (see Chap. 5). The image on the screen will depict the IVC on the left side and the aorta on the right. As the IVC is followed toward the heart, the left, middle, and right hepatic veins will be seen to enter the IVC just before it enters the right atrium.
What happens if IVC is low?
In patients with a low RAP and/or intravascular volume, the IVC size is relatively decreased and its respiratory variability is increased. If RAP is very low, the IVC can collapse completely during spontaneous inspiration. In patients with high RAP and/or intravascular volume, the IVC size is increased and its respiratory variability is decreased. The IVC is very compliant, but its capacity to distend is not unlimited and is restricted by connective tissue in its walls and surrounding structures.
How to measure CVP?
Traditionally, central venous pressure (CVP) and volume status in the acute care setting have been measured by placing a central line. Central lines are invasive, time consuming to insert, and may cause significant complications. Bedside ultrasound has been shown to provide a good estimation of CVP in place of more invasive methods. The clinician can perform serial IVC measurements on an ill patient in order to guide their decision in providing more intravenous fluids or to administer more aggressive medication therapy.
What is color flow doppler?
Color-flow Doppler is used to detect the presence, magnitude, and direction of blood flow. It is useful in differentiating blood vessels from other structures and artifacts in the abdomen.
What frequency is used to visualize IVC?
To visualize the IVC, a phased-array (frequency of 2.0–4.0 MHz) or curvilinear probe (frequency of 3.5–5.0 MHz) should be used. These relatively low-frequency probes provide better penetration and visualization of deep structures.
Is the IVC a circular shape?
The IVC will be thinner-walled, more compressible, and will often have a teardrop shape as opposed to a circular conformation in a transverse view. The IVC will show respiratory variation and may pick up pulsations from the adjacent aorta so “pulsatility” seen on two-dimensional imaging should not be used to differentiate the two. Color-flow Doppler may be used to confirm characteristic arterial flow in the aorta.
What is IVC ultrasound?
Point-of-care ultrasound examination of the inferior vena cava (IVC) offers a rapid, noninvasive determination of right atrial pressure to guide assessment of volume status and volume responsiveness. Image acquisition and interpretation can be mastered after brief, focused training, and various training protocols have been studied in providers from diverse medical specialties. Despite relative ease in image acquisition, interpreting IVC findings requires integration of a number of patient factors before incorporating findings into clinical decision making.
Where is the IVC located?
The IVC is located to the right of the abdominal aorta , and most of the IVC lies in the retroperitoneal space. Between the diaphragm and right atrium, the IVC has a very short intrathoracic segment ( Figure 18.1 ). From the subcostal cardiac window, the IVC appears as a large, intrahepatic vessel with thin walls, and under normal conditions typically demonstrates respirophasic variations in caliber ( Figure 18.2 and#N#Video 18.1#N#). The IVC is a capacitance vessel and thus is sensitive to changes in right atrial pressure and volume status. In spontaneously breathing patients, where the intrathoracic pressure becomes negative during inspiration, the normal response to inspiration is a decrease of IVC diameter ( Figure 18.3 ). In patients on positive-pressure ventilation, the respirophasic change of the IVC is reversed with inspiration causing IVC distention. IVC size may also be influenced by venous return from the splanchnic circulation, diaphragmatic excursions during breathing, and intra-abdominal pressure.
Why is volume responsiveness the strongest correlation of IVC findings?
The strongest correlation of IVC findings to determine volume responsiveness has been demonstrated with patients who are completely passive on a ventilator because the loading conditions of each breath are regulated by the ventilator ; however, a minority of patients in most critical care environments are sedated to the point of passive ventilation.
How to measure IVC diameter?
If choosing to quantitatively measure the IVC or changes with respiration, the image may be frozen and calipers can be used to measure the diameter perpendicular to the long axis of the vein approximately 2 cm from the RA-IVC junction. Once the largest diameter is measured, the cine function can be used, or a second image can be captured, to measure the smallest IVC diameter. Measurements should be taken in an identical manner. M-mode can also be used to measure IVC diameter and respirophasic variation ( Figure 18.8 ).
What type of transducer is used for IVC?
In adults, any low-frequency transducer may be used, including a phased-array, curvilinear, or micro-convex transducer, but the IVC is generally imaged with a phased-array transducer. Two techniques to image the IVC have been described.
What is the M-mode image of the inferior vena cava?
M-mode image of inferior vena cava in a spontaneously breathing patient with respirophasic variation showing measurement of the maximum and minimum diameters.
Where to view IVC?
A long-axis view of the IVC at the right atrial junction from the subcostal window is the recommended view based on reliability and reproducibility (see Chapter 13, Cardiac Ultrasound Technique ). A phased-array transducer is placed in the subcostal window with the transducer marker pointing toward the patient’s head ( Figure 18.4 ). When the IVC is difficult to identify, a helpful strategy is to start with a subcostal 4-chamber view focusing on the right atrium (RA) and then rotate the transducer counterclockwise, aligning the ultrasound beam along the course of the IVC. An ideal long-axis view of the IVC shows the IVC entering the right atrium and a segment of the hepatic vein joining the IVC. Identifying both the RA-IVC junction and hepatic vein helps to avoid mistaking the IVC for the neighboring abdominal aorta. The pulsatile, thicker-walled abdominal aorta can be visualized by tilting the transducer medially. It is imperative to visualize the IVC longitudinally with the transducer centered on the long axis to assess the true diameter accurately. Off-axis imaging generates an oblique view of the vessel, resulting in a falsely small diameter, the so-called “cylinder effect” ( Figure 18.5 ). In general, once a long-axis view of the IVC with the RA-IVC junction and hepatic vein is visualized, fine rotation of the transducer helps to capture the true diameter.
What is the IVC?
The inferior vena cava (IVC) is a large, thin-walled, retroperitoneal blood vessel formed by the confluence of the left and right common iliac veins. It carries the deoxygenated blood from the lower body and lower extremities to the right atrium. Before it drains into the right atrium, it runs a short course through the liver and collects blood from the hepatic veins. It also acts as a venous capacitance reservoir. The IVC typically runs on the right side of the spine. The image below shows it (the large blue vessel) lying next to the abdominal aorta (Figure 1). Rarely, there could be anatomical variants such as left-sided IVC and IVC duplication.
Where does the IVC run?
It also acts as a venous capacitance reservoir. The IVC typically runs on the right side of the spine.
Why is IVC distended?
Some very well-trained and conditioned elite athletes may have a normal physiologically distended IVC due to increased venous reserves. Some examples of pathophysiological IVC dilatation may be cardiac tamponade, pneumothorax, hemodynamically significant pulmonary embolism (PE), some cases of myocardial infarction, and decompensated heart failure. IVC may be small or collapsed in severe dehydration, significant blood loss due to bleeding, and sepsis. In these conditions, the IVC diameter may not be an accurate indicator of volume status.
Where is the IVC measured?
The IVC collapses non-uniformly. Most studies measure the IVC at or around the confluence with the hepatic veins. An influential study by Wallace et al warned against measuring at the junction with the right atrium, but with no gold standard in their study they had no actual justification for this advice.
Is IVC a good test for fluid tolerance?
IVC is not a great test for intravascular volume status, fluid responsiveness or even fluid tolerance. Then again, it might be. The problem is that no-one really knows. A lot of big statements have come out of a lot of teeny studies that don’t really back them up.
Is clinical context more important than IVC ultrasound?
Be a doctor. Clinical context is more important than IVC ultrasound.
What is the most likely evaluation of IVC?
Initial evaluation of the IVC is most likely to occur at computed tomography performed for another indication. Many routine abdominal imaging protocols may result in suboptimal evaluation of the IVC; however, techniques to assist in specific evaluation of the IVC can be used.
Why is there no IVC?
Congenital absence of the entire IVC or of only the infrarenal IVC ( 6 – 10) has been previously described but has an unknown incidence and unclear cause. IVC absence may result from complete failure of embryonic vein development; however, perinatal venous thrombosis and atrophy have also been suggested ( 8 – 10 ). In addition to inability to identify the IVC at imaging, prominent venous collateralization may be a finding ( Fig 2 ). Patients may experience lower extremity venous insufficiency or idiopathic deep vein thrombosis or have prominent lumbar collateral vessels, which can be mistaken for paraspinal masses ( 6 – 11 ).
What is the most common imaging modality for initial detection of IVC variants and pathologic findings?
Because CT is used to evaluate a wide variety of abdominal symptoms, it is likely to be the most common imaging modality for initial detection of IVC variants and pathologic findings. Routine abdominal imaging at 60–70 seconds after intravenous administration of contrast material (portal venous phase) shows enhancement in the renal and suprarenal IVC but may also show admixture artifact in the infrarenal IVC ( 1, 2 ).
What is the IVC in the right atrium?
The inferior vena cava ( IVC) is the main conduit of venous return to the right atrium from the lower extremities and abdominal viscera. It can be a source of critical information for referring clinicians, and recognition of IVC variants and pathologic characteristics can help guide patient treatment.
Why is it important to identify duplication of IVC?
Identification of duplication of the IVC is important in patient treatment because if the entity is not recognized before routine placement of an infrarenal IVC filter, recurrent pulmonary embolism can develop ( 5 ).
How many segments are there in the IVC?
The mature IVC has four segments: the hepatic, suprarenal, renal, and infrarenal IVC ( 4 ). Formation of the IVC involves complex anastomoses and regression of multiple embryonic veins, including the vitelline vein and the paired posterior cardinal, subcardinal, and supracardinal veins ( Fig 1 ).
What is the inferior vena cava?
The inferior vena cava (IVC) is an essential but often overlooked structure at abdominal imaging. It is associated with a wide variety of congenital and pathologic processes and can be a source of vital information for referring clinicians. Initial evaluation of the IVC is most likely to occur at computed tomography performed for another indication. Many routine abdominal imaging protocols may result in suboptimal evaluation of the IVC; however, techniques to assist in specific evaluation of the IVC can be used. In this article, the authors review the spectrum of IVC variants and pathologic processes and the relevant findings from magnetic resonance imaging, angiography, sonography, and positron emission tomography. Embryologic development of the IVC and examples of congenital IVC variants, such as absence, duplication, left-sided location, azygous or hemiazygous continuation, and web formation, are described. The authors detail IVC involvement in Wilms tumor, leiomyosarcoma, adrenal cortical carcinoma, testicular carcinoma, hepatocellular carcinoma, renal cell carcinoma, and other neoplasms, as well as postsurgical, traumatic, and infectious entities (including filter malposition, mesocaval shunt, and septic thrombophlebitis). The implications of these entities for patient treatment and instances in which specific details should be included in the dictated radiology report are highlighted. Furthermore, the common pitfalls of IVC imaging are discussed. The information provided in this review will allow radiologists to detect and accurately characterize IVC abnormalities to guide clinical decision making and improve patient care.
Background
- Though controversial, IVC measurement by ultrasound can estimate volume status, fluid responsiveness, and fluid tolerance
- Can use as a dynamic assessment after intervention such as giving fluids or passive leg raise
- Dynamic changes is probably best measured in intubated patients
- Though controversial, IVC measurement by ultrasound can estimate volume status, fluid responsiveness, and fluid tolerance
- Can use as a dynamic assessment after intervention such as giving fluids or passive leg raise
- Dynamic changes is probably best measured in intubated patients
Indications
- Differentiate causes of shock
- Differentiate causes of shortness of breath
- Establish likelihood of fluid responsiveness
- Assess response to interventions
Technique
- Select probe
- Location
- Longitudinal view
- Dynamic measurements
Pearls and Pitfalls
- Aorta can be confused for IVC, ensure you visualize the vessel entering the atrium
- Ensure the vessel is viewed in full longitudinal axis as being off-center will give falsely narrow measurements
Documentation
- Normal Exam
A bedside IVC ultrasound was performed to assess volume status in setting of dehydration. The IVC was identified in longitudinal access. The IVC was neither flat nor plethoric. There was less than 50% collapse with respirophasic measurements. This does not imply that the patient is not … - Abnormal Exam
A bedside IVC ultrasound was performed to assess volume status in setting of dehydration. The IVC was identified in longitudinal access. The IVC was flat with over 50% collapse with respirophasic measurements. There was evidence of volume depletion and fluid tolerance. A be…
External Links