
Is 60 good pulse?
For most of us (adults), between 60 and 100 beats per minute (bpm) is normal.1 The rate can be affected by factors like stress, anxiety, hormones, medication, and how physically active you are. An athlete or more active person may have a resting heart rate as low as 40 beats per minute. Now that’s chill!
What are the main causes of bradycardia?
Causes of bradycardia (slow heart rate) may include:
- Problems with the sinoatrial (SA) node, considered the heart’s natural pacemaker
- Problems in the conduction pathways of the heart that don’t allow electrical impulses to pass properly from the atria to the ventricles
- Metabolic problems such as low thyroid hormone ( hypothyroidism)
- Heart damage from heart disease or a heart attack
What is the prognosis of bradycardia?
Prognosis. Bradycardia may be an acute or chronic problem depending upon the etiology. It may resolve and never recur if the inciting event is treated or removed (e.g., hypothyroidism, electrolyte derangements, or medications). However, for patients with an underlying conduction system disease, bradycardia will require frequent follow-up, with long-term and sometimes lifelong therapy for those with a pacemaker.
What is bradycardia and what causes it?
What causes a low heart rate?
- A heart malfunction. The most common cause for bradycardia is a malfunction in the heart’s natural pacemaker, the sinus node.
- AV Block. Another cause of bradycardia is atrioventricular block ( AV Block ), in which the top and bottom chambers don’t communicate well and your heart rate drops as a ...
- Age. ...
- Having certain illnesses or conditions. ...

What causes junctional bradycardia?
Causes of a junctional rhythm include: Inflammation of the heart: If your heart muscle is inflamed, the SA node may become damaged or stop working. Heart surgery and myocarditis are common causes of heart inflammation. It can also occur from sepsis or certain infections like Lyme disease or rheumatic fever.
What are the symptoms of junctional bradycardia?
Complications of junctional rhythm are usually limited to symptoms such as dizziness, dyspnea, or presyncope. Accidental injury may result from syncope if the arrhythmia is not tolerated well. Exacerbation of cardiac comorbidities, such as congestive heart failure and rate-related cardiac ischemia, may occur.
How is junctional bradycardia treated?
No pharmacologic therapy is needed for asymptomatic, otherwise healthy individuals with junctional rhythms that result from increased vagal tone. In patients with complete AV block, high-grade AV block, or symptomatic sick sinus syndrome (ie, sinus node dysfunction), a permanent pacemaker may be needed.
What does junctional mean in ECG?
A junctional rhythm is where the heartbeat originates from the AV node or His bundle, which lies within the tissue at the junction of the atria and the ventricle. Generally, in sinus rhythm, a heartbeat is originated at the SA node.
What is the most common initial treatment for junctional rhythm?
Treatment of junctional beats and rhythm Symptomatic junctional rhythm is treated with atropine. Doses and alternatives are similar to management of bradycardia in general.
Can anxiety cause junctional rhythm?
An issue with your heart's electrical wiring system can lead to junctional tachycardia. You may be born with it, or it might happen later. Drug use or anxiety could trigger the condition.
What are the three types of junctional rhythms?
Types of Junctional Rhythm. The three types of junctional rhythm are categorized according to the resulting heart rate. In order of ascending beats per minute (bpm), these are junctional rhythm (or junctional escape rhythm), accelerated junctional rhythm, and junctional tachycardia.
What symptoms might occur in a patient with junctional escape rhythm?
Palpitations, fatigue, or poor exercise tolerance: These may occur during a period of junctional rhythm in patients who are abnormally bradycardic for their level of activity. Dyspnea: Sudden onset of symptoms and sudden termination of symptoms may occur, especially in the setting of complete heart block.
Is junctional tachycardia life threatening?
Primary or congenital (since birth) junctional tachycardia is harder to treat and can lead to heart failure, complete heart block or ventricular fibrillation. Up to 9% of cases are fatal without treatment.
What makes a rhythm junctional?
Junctional rhythm can be due to hypokalemia, MI (usually inferior), cardiac surgery, digitalis toxicity (rare today), sinus node dysfunction, or after ablation for AV node reentrant tachycardia. It can be caused by necessary medications (e.g., β-adrenergic blockers, verapamil, digitalis, sotalol, amiodarone).
What is the difference between AFIB and junctional rhythm?
Atrial fibrillation is also considered to be an atrial tachycardia. Junctional tachycardias originate from within the AV node or involve re-entrant circuits within the AV node. Supraventricular tachycardias are also known as narrow-complex tachycardias, as the QRS complex resembles normal sinus complexes.
Where is the junction in the heart?
Atrioventricular (AV) junction is the area separating atria and the ventricles of the heart. [1] Specifically, when talking about the AV junction, the focus is put more on its contents, the AV node and the nonbranching bundle of His.
What symptoms might occur in a patient with junctional escape rhythm?
Palpitations, fatigue, or poor exercise tolerance: These may occur during a period of junctional rhythm in patients who are abnormally bradycardic for their level of activity. Dyspnea: Sudden onset of symptoms and sudden termination of symptoms may occur, especially in the setting of complete heart block.
What drug can cause a junctional rhythm?
Junctional rhythm can be due to hypokalemia, MI (usually inferior), cardiac surgery, digitalis toxicity (rare today), sinus node dysfunction, or after ablation for AV node reentrant tachycardia. It can be caused by necessary medications (e.g., β-adrenergic blockers, verapamil, digitalis, sotalol, amiodarone).
What is the most common cause of junctional tachycardia?
What causes junctional tachycardia?Myocarditis (inflammation of your heart muscle).Heart attack.Heart valve replacement or other heart surgeries.Congenital (since birth) heart disease (this is a rare cause).Catheter ablation for a different abnormal rhythm.Lyme disease.
What are the three types of junctional rhythms?
Types of Junctional Rhythm. The three types of junctional rhythm are categorized according to the resulting heart rate. In order of ascending beats per minute (bpm), these are junctional rhythm (or junctional escape rhythm), accelerated junctional rhythm, and junctional tachycardia.
Overview
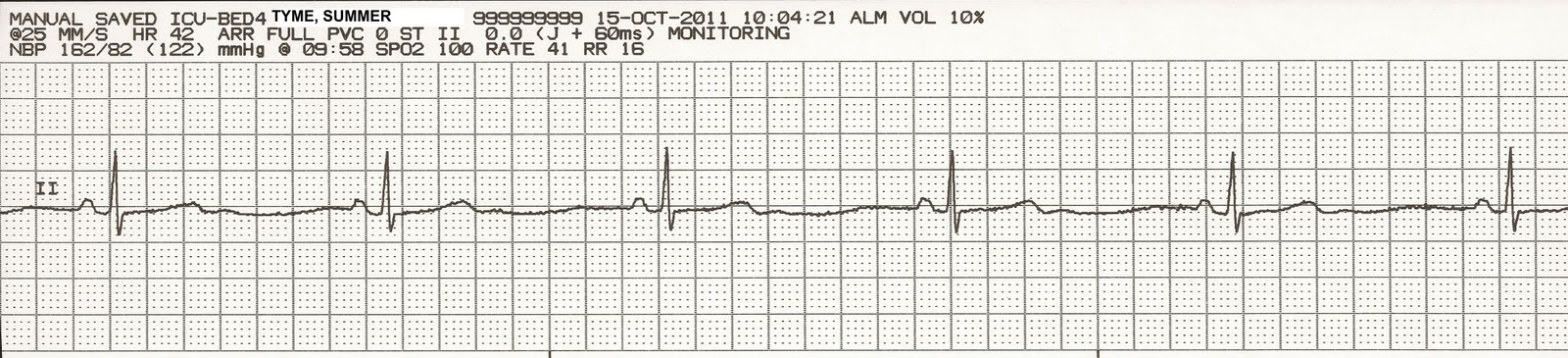
Junctional bradycardia is a slow (40 to 60 beats per minute) narrow complex escape rhythm that originates in the atrioventricular node to compensate for slow or impaired conduction of pacemaker activity in the atrium.
Pathophysiology
Junctional bradycardia or an AV junctional escape is a delayed heartbeat originating from an ectopic focus somewhere in the AV junction to compensate for an SA node that is no longer handling the pacemaking activity.
Causes
Junctional bradycardia occurs when the rate of depolarization of the SA node falls below the rate of the AV node or when the electrical impulses from the SA node fail to reach the AV node because of SA or AV block.
Differentiating Junctional Bradycardia from other Diseases
Junctional bradycardia or junctional escape rhythm need to be differentiated from other bradycardia conditions which has the bundle of His or the ventricles as their pacemaker compensating for the failed SA node.
Epidemiology and Demographics
Junctional bradycardia is fairly uncommon. It can occur in any age group, however it is more likely to be observed in elderly people with underlying heart disease.
Natural History, Complications and Prognosis
Junctional bradycardia mostly results due to failure of impulse transmission from SA node. Its severity of symptoms depends on the underlying cause.
Diagnosis
Junctional bradycardia symptoms mostly are due to decrease cardiac output and may present with sometimes with loss of consciousness and syncope.
Objectives
Identify a junctional rhythm based on a narrow QRS complex without a preceding P wave.
Teaching Instructions
Preparation: Plan to spend 5-10 minutes familiarizing yourself with the animations of the PowerPoint and the key findings of this ECG.
Where does Bradycardia start?
Bradycardia often starts in the area of the heart called the sinus node. In some people, sinus node problems cause alternating slow and fast heart rates (bradycardia-tachycardia syndrome).
How to prevent bradycardia?
The most effective way to prevent bradycardia is to reduce your risk of developing heart disease. If you already have heart disease, monitor it and follow your treatment plan to lower your risk of bradycardia.
Why is my heart slow?
Bradycardia, shown on the right, is a slower heart rhythm that may occur because the sinus node in the heart may be discharging electrical impulses at a slower than normal rate. A heart with a normal heart rhythm is shown on the left. Bradycardia may also be due to other causes. Bradycardia can be caused by:
What causes a bamcardia?
Bradycardia can be caused by: Heart tissue damage related to aging. Damage to heart tissues from heart disease or heart attack. Heart disorder present at birth (congenital heart defect) Infection of heart tissue (myocarditis) A complication of heart surgery.
Why do you need a pacemaker for bradycardia?
If bradycardia is severe, an implanted pacemaker may be needed to help the heart maintain an appropriate rate.
What to do if you faint from bradycardia?
If you faint, have difficulty breathing or have chest pain lasting more than a few minutes, get emergency care or call 911 or your local emergency number. Seek emergency care for anyone with these symptoms.
Does heart disease increase risk of bradycardia?
Therefore, factors that increase your risk of heart disease can also increase the risk of bradycardia. Lifestyle changes or medical treatment might decrease the risk of heart disease associated with the following factors:
What is junctional rhythm?
A junctional rhythm is an abnormal heart rhythm that originates from the AV node or His bundle. This activity reviews the evaluation and management of junctional rhythm and highlights the role of the interprofessional team in educating patients about their prognosis.
Which artery supplies blood to the AV node?
The blood supply to the AV node is from the AV nodal branch of the right coronary artery (90%) or the left circumflex artery (10%) depending on right or left dominant blood supply to the heart. The first septal perforator of the left anterior descending artery also supplies blood to the AV node.
What is the histopathology of a disease that can contribute to the AV node/His bundle?
Histopathology of a disease SA node that can contribute to the AV node/His bundle taking over as a pacemaker secondary to their intrinsic automaticity includes SA node fibrosis, atrophy, hypoplasia, or amyloidosis. A normal SA node histopathology does not rule out reduced SA node automaticity contributing to a junctional rhythm. [11][12]
What is the difference between atrioventricular and sinoatrial node?
The sinoatrial node (SA) is the default pacemaker and is located subepicardially and is crescent in shape. The atrioventricular node (AV) is a subendocardial structure situated in the inferior-posterior right atrium. It sits within an anatomic region bordered posteriorly by the coronary sinus ostium, superiorly by the tendon of Todaro, and anteriorly by the septal tricuspid valve annulus. This anatomic region is also commonly referred to as the triangle of Koch. The sinoatrial nodal artery supplies blood to the sinoatrial node, it branches off the right coronary artery in 60% of cases, whereas in 40% of cases, it comes from the left circumflex coronary artery. The blood supply to the AV node is from the AV nodal branch of the right coronary artery (90%) or the left circumflex artery (10%) depending on the right or left dominant blood supply to the heart. The first septal perforator of the left anterior descending artery also supplies blood to the AV node. A junctional rhythm is where the heartbeat originates from the AV node or His bundle, which lies within the tissue at the junction of the atria and the ventricle. Generally, in sinus rhythm, a heartbeat is originated at the SA node. This electrical activity then travels through the atria to the AV node from where it reaches the Bundle of His from where the electrical signals travel to the ventricles through the Purkinje fibers. [1][2][3][4][5][6]
Where is the sinoatrial node?
The sinoatrial node is the natural cardiac pacemaker located in the upper right atrium. The atrioventricular node is a separate cardiac pacemaker located in the inferior-posterior right atrium. The His bundle is a separate cardiac pacemaker located at the inferior end of the atria and ventricle. A junctional rhythm is an abnormal heart rhythm ...
Where does the heartbeat originate?
A junctional rhythm is where the heartbeat originates from the AV node or His bundle , which lies within the tissue at the junction of the atria and the ventricle. Generally, in sinus rhythm, a heartbeat is originated at the SA node.
Can junctional rhythm cause shortness of breath?
Patients with junctional rhythm may present with a varied array of symptoms or may be asymptomatic. Symptoms mostly depend on the underlying cause of the junctional rhythm, for instance, a patient presenting with heart failure exacerbation may present with shortness of breath, wheezing, and lower extremity edema.
What is the heart rate of junctional tachycardia?
With accelerated, it's between 60 and 100. With junctional tachycardia, the heart rate will be over 100. In this case, we have approximately 115 beats per minute, so that fits the bill for junctional tachycardia.
What are the different types of junctional dysrhythmias?
In this article, you will learn about the different junctional dysrhythmias, including junctional rhythms, junctional bradycardia, accelerated junctional rhythms, and junctional tachycardia. The EKG Interpretation video series follows along with our EKG Interpretation Flashcards, which are intended to help RN and PN nursing students study for nursing school exams, including the ATI, HESI exams, and NCLEX.
What is the secondary backup for the heart?
As we explained in our article on the natural pacemakers of the heart, a junctional rhythm is the secondary backup for the heart. When the sinus node fails to kick off an electrical impulse to make the heart beat, the atrial foci are the first backup, and if that fails, the junctional foci are the next backup.
How many beats per minute is junctional rhythm?
The inherent rate of a junctional rhythm is a little slower, so it's between 40 and 60 beats per minute. And the key characteristic of a junctional rhythm is that the P wave is messed up. It's either absent, it's inverted, it happens after the QRS complex instead of before, or we have a very short PR interval.
What is the rate of junctional rhythm?
The inherent rate of a junctional rhythm is slower than a normal heart rate, usually between 40 and 60 beats per minute. The key characteristic of a junctional rhythm is an abnormal P rate. The P rate will be either absent, inverted, in the wrong place, or with a very short PR interval. When you encounter an EKG strip on a test, looking for those abnormal P wave conditions can help you identify a rhythm as junctional.
Can digoxin cause junctional dysrhythmia?
One important tip to keep in mind is that you would NOT use digoxin in patients with junctional dysrhythmias. Digoxin toxicity is one of the most common causes of junctional rhythms.
Is the ventricular rhythm regular?
There are equal distances between the R waves, meaning the ventricular rhythm is regular. The P waves, though they look strange, are also regular; they have an equal distance between them. So the atrial rhythm is also regular.
What causes bradycardia in the AV node?
Junctional bradycardia is most commonly caused by toxicity from AV node blockers, post valve surgery and inferior MI
What are the signs of an unstable bradycardic patient?
Cardiac output is dependent on heart rate and stroke volume. Depressed cardiac output in the setting of overt bradycardic shock will manifest as hypotension, as well as signs of decreased organ perfusion such as altered mental status, chest pain, dyspnea or syncope – all signs of an “unstable” bradycardic patient. However, be cautious to not miss occult bradycardic shock where the vasoconstrictor response in the setting of bradycardia maintains ones blood pressure and mental status. The patient however may still have low cardiac output and thus be “unstable”. The clinical exam assessing for poor end-organ perfusion (altered LOA, cool extremities, low urine output etc) is critical in diagnosing occult bradycardic shock.
What is the name of the condition where the sinus node is dysfunctional?
One variant of sinus node dysfunction (sick sinus syndrome) is tachy-brady syndrome. This syndrome tends to occur in older patients with a history of paroxysmal atrial fibrillation, and it manifests as conversion pauses or sinus bradycardia when the patient converts from atrial fibrillation to sinus, giving rise to presyncope/syncope.
What is BRASH syndrome?
BRASH syndrome ( Bradycardia, Renal Failure, AV Blockade, Shock, and Hyperkalemia) refers to a vicious cycle which may occur in the setting of AV node blockers, renal failure and hyperkalemia. A patient on AV nodal blocking agents sustains renal injury, causing hyperkalemia which synergizes with AV nodal blockers causing a worsening spiral of hyperkalemia, renal failure, and bradycardic shock.
What happens if you have AV block with bradycardia?
If you see the presence of bradycardia with AV block along with short runs of polymorphic VT, these patients need urgent treatment as they may degenerate into ventricular fibrillation.
What is the 4th step of bradycardia?
The 4 th step often needs to be done in parallel with steps 1-3 in order to rule out secondary cause or causes that if treated, may preclude the need for atropine, sympathetic stimulation and pacing.
What is the common pitfall for tachy-brady?
Pitfall: A common pitfall is to administer standard rate control agents such as beta blockers and calcium channel blockers to a patient who presents in rapid atrial fibrillation who has underlying tachy-brady syndrome.
How many beats per minute in a junctional bradycardia strip?from leveluprn.com
With junctional bradycardia, the heart rate is under 40 beats per minute. So in this case, we have 33 beats per minute. So that fits the bill here, and that's how we know we are looking at a junctional bradycardia strip.
What is the key characteristic of junctional rhythm?from leveluprn.com
And the key characteristic of a junctional rhythm is that the P wave is messed up. It's either absent, it's inverted, it happens after the QRS complex instead of before, or we have a very short PR interval.
What is the secondary backup for the heart?from leveluprn.com
As we explained in our article on the natural pacemakers of the heart, a junctional rhythm is the secondary backup for the heart. When the sinus node fails to kick off an electrical impulse to make the heart beat, the atrial foci are the first backup, and if that fails, the junctional foci are the next backup.
What are the different types of junctional dysrhythmias?from leveluprn.com
In this article, you will learn about the different junctional dysrhythmias, including junctional rhythms, junctional bradycardia, accelerated junctional rhythms, and junctional tachycardia. The EKG Interpretation video series follows along with our EKG Interpretation Flashcards, which are intended to help RN and PN nursing students study for nursing school exams, including the ATI, HESI exams, and NCLEX.
What is the rate of junctional rhythm?from leveluprn.com
The inherent rate of a junctional rhythm is slower than a normal heart rate, usually between 40 and 60 beats per minute. The key characteristic of a junctional rhythm is an abnormal P rate. The P rate will be either absent, inverted, in the wrong place, or with a very short PR interval. When you encounter an EKG strip on a test, looking for those abnormal P wave conditions can help you identify a rhythm as junctional.
What is the heart rate of junctional tachycardia?from leveluprn.com
With accelerated, it's between 60 and 100. With junctional tachycardia, the heart rate will be over 100. In this case, we have approximately 115 beats per minute, so that fits the bill for junctional tachycardia.
Is the ventricular rhythm regular?from leveluprn.com
There are equal distances between the R waves, meaning the ventricular rhythm is regular. The P waves, though they look strange, are also regular; they have an equal distance between them. So the atrial rhythm is also regular.
Overview
- Junctional bradycardia is a slow (40 to 60 beats per minute) narrow complex escape rhythm that originates in the atrioventricular nodeto compensate for slow or impaired conduction of pacemaker activity in the atrium.
Pathophysiology
- Junctional bradycardia or an AV junctional escape is a delayed heartbeat originating from an ectopic focus somewhere in the AV junction to compensate for an SA nodethat is no longer handling the pacemaking activity.
Causes
- Junctional bradycardia occurs when the rate of depolarization of the SA node falls below the rate of the AV node or when the electrical impulses from the SA node fail to reach the AV node because of SA or AV block. SA node fibrosis and inferior wall myocardial infarction causing sinus arrestmay cause the AV node to become the dominant pacemaker of the heart.
Differentiating Junctional Bradycardia from Other Diseases
- Junctional bradycardia or junctional escape rhythm need to be differentiated from other bradycardia conditions which has the bundle of His or the ventriclesas their pacemaker compensating for the failed SA node.
Epidemiology and Demographics
- Junctional bradycardia is fairly uncommon. It can occur in any age group, however it is more likely to be observed in elderly people with underlying heart disease.
Natural History, Complications and Prognosis
- Junctional bradycardia mostly results due to failure of impulse transmission from SA node. Its severity of symptoms depends on the underlying cause.
Diagnosis
- History and Symptoms
Junctional bradycardia symptoms mostly are due to decrease cardiac outputand may present with sometimes with loss of consciousness and syncope. - Physical Examination
Complete physical examination help determine any heart defectsas a cause for junctional bradycardia and assess the severity of the condition.
Treatment
- Medical Therapy
Treatment of junctional bradycardia depends on the severity of presentation. Atropinecan be used to manage symptomatic patients. - Surgery
Junctional bradycardia patients should be placed on pacemaker if there is complete AV block or sick sinus syndrome.