
Pleural effusion is a relatively rare complication of chronic lymphatic leukemia (CLL). It can be the result of primary pleural involvement, central lymphatic blockage, infection or changes induced by previous irradiation or chemotherapy.
How serious is a pleural effusion?
The seriousness of the condition depends on the primary cause of pleural effusion, whether breathing is affected, and whether it can be treated effectively. Causes of pleural effusion that can be effectively treated or controlled include an infection due to a virus, pneumonia or heart failure.
What are the treatments for a pleural effusion?
Treatment
- Thoracentesis. If the effusion is large, your doctor may take more fluid than they need for testing, just to ease your symptoms.
- Pleural drain. If your pleural effusions keep coming back, your doctor may put a long-term catheter through your skin into the pleural space.
- Pleurodesis. ...
- Pleural decortication. ...
What are the risk factors for pleural effusion?
The potential complications associated with pleural effusion are:
- Lung scarring,
- Pneumothorax (collapse of the lung) as a complication of thoracentesis,
- Empyema (a collection of pus within the pleural space), and
- Sepsis (blood infection) sometimes leading to death.
What are the causes of pleural effusion?
Other less common causes of pleural effusion include:
- Tuberculosis
- Autoimmune disease
- Bleeding (due to chest trauma)
- Chylothorax (due to trauma)
- Rare chest and abdominal infections
- Asbestos pleural effusion (due to exposure to asbestos)
- Meig’s syndrome (due to a benign ovarian tumor)
- Ovarian hyperstimulation syndrome
Are lymphocytes normal in pleural fluid?
While previous studies have shown that lymphocytes constitute up to 90% of total cells in pleural fluid with pleural TB [9, 10], recent retrospective studies have reported that the level of lymphocytes in pleural fluid decreased in patients who were diagnosed with pleural TB [11, 12].
What is the best treatment for pleural effusion?
Diuretics and other heart failure medications are used to treat pleural effusion caused by congestive heart failure or other medical causes. A malignant effusion may also require treatment with chemotherapy, radiation therapy or a medication infusion within the chest.
What are the 2 types of pleural effusion?
There are two types of pleural effusion:Transudative pleural effusion is caused by fluid leaking into the pleural space. ... Exudative effusion is caused by blocked blood vessels or lymph vessels, inflammation, infection, lung injury, and tumors.
Does pleural effusion mean cancer?
For people with cancer, pleural effusions are often malignant (see above). This means that there are cancer cells in the pleural space causing fluid to build up. Sometimes, a pleural effusion can occur as a result of inflammation, lung obstruction, trauma, or another medical condition that may not be due to cancer.
Is pleural effusion serious?
Fluid around the lung (pleural effusion) is a potentially dangerous condition that can masquerade as something less worrisome. What may seem like chest pain or coughing due to a bad cold could actually have serious health ramifications.
How long can you live with pleural effusion?
Many patients with pleural effusions die within 30-days of admission to the hospital, and nearly 1/3 are dead within one year. A higher level of aggressive medical therapy may be warranted for those patients who present with pleural effusions in order to decrease their potential risk of death.
What is the most common cause of pleural effusion?
There are two types of pleural effusion: Transudative pleural effusion is caused by fluid leaking into the pleural space. This is from increased pressure in the blood vessels or a low blood protein count. Heart failure is the most common cause.
What happens if pleural effusion is left untreated?
Without treatment, pleural effusion can be very serious and even life-threatening. Depending on its severity and its cause, it can lead to a collapsed lung, lung scarring or sepsis (an out-of-control infection). It may indicate progression of the underlying disease.
Will pleural effusion go away?
A minor pleural effusion often goes away on its own. Doctors may need to treat the condition that is causing the pleural effusion. For example, you may get medicines to treat pneumonia or congestive heart failure. When the condition is treated, the effusion usually goes away.
What stage of cancer causes pleural effusion?
Stage IV cancer also includes people who have a fluid collection around the lung (called a malignant pleural effusion) caused by the cancer. Stage IV NSCLC cannot be cured, but treatment can reduce pain, ease breathing, and extend and improve quality of life.
What type of cancer causes pleural effusion?
Who can get a malignant pleural effusion? People with lung cancer, breast cancer, and lymphoma (a cancer of lymphatic tissue) are most likely to get a MPE. Mesothelioma (a rare cancer of the pleura itself) is another common cause of MPE.
What are the stages of pleural effusion?
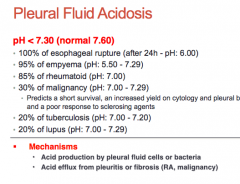
The evolution of a parapneumonic pleural effusion, as shown in the image below, can be divided into 3 stages, including exudative, fibrinopurulent, and organization stages. Left pleural effusion developed 4 days after antibiotic treatment for pneumococcal pneumonia.
Can pleural effusion be treated with medication?
Medication. Medication may be used in treatment especially if there is an infection. Types of medication used to treat pleural effusion include steroids, anti-inflammatories, diuretics or antibiotics.
How long does it take to cure pleural effusion?
The time that it will take to recover can be dependent on the size, severity, cause, and your overall health. You will have to stay in the hospital overnight, but you will feel back to normal, on average, between 2-4 weeks.
Can Lasix remove pleural effusion?
The use of medications for pleural effusions depends on the underlying cause. Antibiotics are used when there is an infectious cause, whereby diuretics such as furosemide (Lasix) may be used to slowly help reduce the size of the pleural effusion.
Can antibiotics cure pleural effusion?
(See "Society guideline links: Pleural effusion".) Antibiotics – All patients with suspected (or diagnosed) parapneumonic effusion or empyema should be treated with antibiotics. Antibiotic therapy should be administered promptly and not delayed for sampling or drainage procedures.
What Is Pleural Effusion?
Pleural effusion, sometimes referred to as “water on the lungs,” is the build-up of excess fluid between the layers of the pleura outside the lungs...
What Causes Pleural Effusion?
Pleural effusions are very common, with approximately 100,000 cases diagnosed in the United States each year, according to the National Cancer Inst...
Is Pleural Effusion Serious?
The seriousness of the condition depends on the primary cause of pleural effusion, whether breathing is affected, and whether it can be treated eff...
What Are The Symptoms of Pleural Effusion?
Some patients with pleural effusion have no symptoms, with the condition discovered on a chest x-ray that is performed for another reason. The pati...
How Is Pleural Effusion Diagnosed?
The tests most commonly used to diagnose and evaluate pleural effusion include: 1. Chest x-ray 2. Computed tomography (CT) scan of the chest 3. Ult...
How Is Pleural Effusion Treated?
1. Treatment of pleural effusion is based on the underlying condition and whether the effusion is causing severe respiratory symptoms, such as shor...
What causes pleural effusion?
Causes of pleural effusion that can be effectively treated or controlled include an infection due to a virus, pneumonia or heart failure. Two factors that must be considered are treatment for associated mechanical problems as well as treatment of the underlying cause of the pleural effusion.
How many incisions are needed for pleural effusion?
A minimally-invasive approach that is completed through 1 to 3 small (approximately ½ -inch) incisions in the chest. Also known as thoracoscopic surgery, this procedure is effective in managing pleural effusions that are difficult to drain or recur due to malignancy. Sterile talc or an antibiotic may be inserted at the time of surgery to prevent the recurrence of fluid build-up.
What is the water on the lungs called?
Pleural effusion, sometimes referred to as “water on the lungs,” is the build-up of excess fluid between the layers of the pleura outside the lungs. The pleura are thin membranes that line the lungs and the inside of the chest cavity and act to lubricate and facilitate breathing. Normally, a small amount of fluid is present in the pleura.
Can pleural effusions be treated?
Pleural effusions that cannot be managed through drainage or pleural sclerosis may require surgical treatment.
Can radiation cause pleural effusion?
Certain medications, abdominal surgery and radiation therapy may also cause pleural effusions. Pleural effusion may occur with several types of cancer including lung cancer, breast cancer and lymphoma. In some cases, the fluid itself may be malignant (cancerous), or may be a direct result of chemotherapy.
Can pleural effusion cause cough?
Some patients with pleural effusion have no symptoms, with the condition discovered on a chest x-ray that is performed for another reason. The patient may have unrelated symptoms due to the disease or condition that has caused the effusion.Symptoms of pleural effusion include: Chest pain. Dry, nonproductive cough.
What is pleural effusion?
Pleural effusion. Pleural effusions are abnormal accumulations of fluid within the pleural space . They may result from a variety of pathological processes which overwhelm the pleura's ability to reabsorb fluid.
What are some examples of pleural effusions?
Examples: bronchial carcinoma. secondary (metastatic) malignancy. pulmonary embolism and infarction - pleural effusions in pulmonary embolism. pneumonia.
How many mL of pleural effusion is there?
In routine practice the above calculation is rarely needed (online calculators are available for this purpose 17 ), as with a slight rounding maximum effusion depths of 2, 4, 6, 8, and 10 cm represent volumes of approximately 200, 500, 800, 1100, and 1400 mL of pleural effusion.
How much fluid is in the pleural cavity?
Physiologically, the pleural cavities normally contain approximately 15 mL of serous pleural fluid 6. Any process which results in more fluid forming than can be absorbed will produce a pleural effusion.
How much fluid is needed for a pleural effusion?
Chest radiographs are the most commonly used examination to assess for the presence of a pleural effusion; however, it should be noted that on a routine erect chest x-ray as much as 250-600 mL of fluid is required before it becomes evident 6.
Why does lymph node drainage occur?
It occurs due to the increase in permeability of the microcirculation or alteration in the pleural space drainage to lymph nodes. Examples:
Is pleural fluid accumulation a demographic?
As the accumulation of fluid in the pleural space occurs in a broad range of disparate clinical scenarios, no single demographic is affected ; rather the epidemiology will match that of the underlying condition. However, it is probably safe to say that as congestive cardiac failure and malignancy are some of the most common causes, older patients would be over-represented.
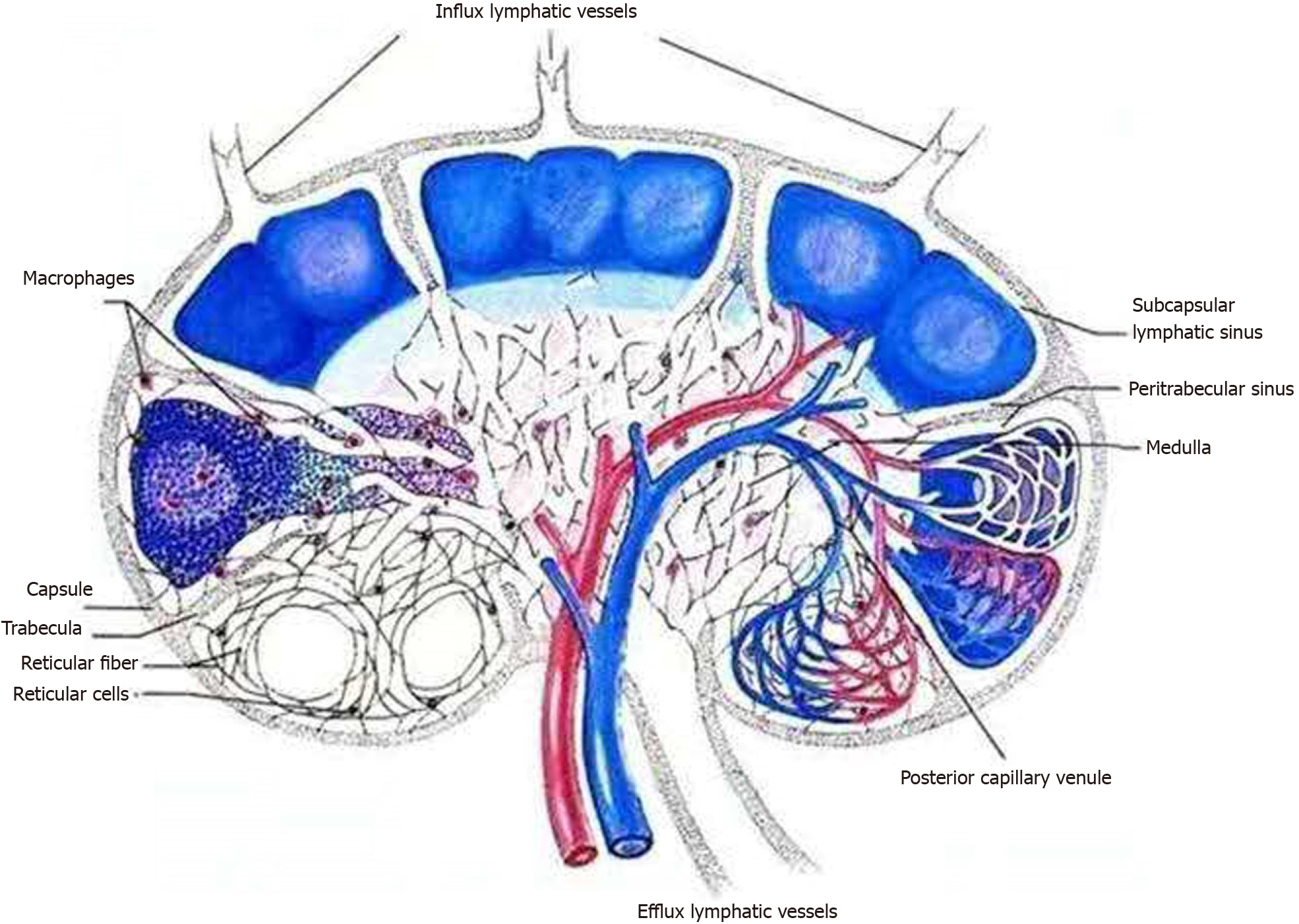
What is the function of the pleural lymphatic system?
The pleural lymphatic system has a great absorption capacity. Its most known function is fluid resorption. The pleura which cover the lungs (visceral pleura), the mediastinum, diaphragm and thoracic wall (parietal pleura) are formed by a mesothelial cell layer (mesothelium). This permeable layer is in direct contact with the vascular endothelium. The mesothelium is based over a connective tissue (interstitium) containing the blood and lymphatic vessels. The primary lymphatic vessels drain interstitium but are also in direct contact with pleural space by the stoma or openings, situated in the lower parts of parietal pleura, i.e: diaphragm, over lower ribs and mediastinum but not existing in the adjacent visceral pleura. In addition, a part of interstitial pulmonary fluid entered in the pleural cavity by passing the visceral pleura would be absorbed by these openings. The resorption process is active and directly related to the function of smooth muscles of lymphatic vessels. Besides resorption, we must emphasize that this "pumping" activity is permanent and the origin of negative pressure (the pleural void) in pleural cavity, a unique property. The other resorbed elements are molecules, bacterial and cellular debris, cells, red blood and cancer cells.
Which lymphatic system has the greatest capacity for fluid resorption?
The pleural lymphatic system has a great absorption capacity. Its most known function is fluid resorption. The pleura which cover the lungs (visceral pleura), the mediastinum, diaphragm and thoracic wall (parietal pleura) are formed by a mesothelial cell layer (mesothelium). This permeable layer is …
What causes pleural effusion?
There is a wide differential for an exudative lymphocyte-rich pleural effusion, with the most common causes listed in the BTS pleural disease guidelines, 1 including malignancy, lymphoma, tuberculosis, cardiac failure, postcoronary artery bypass graft and rheumatological disease .
What causes pleural effusion in granulomatous disease?
Rarer causes of a lymphocytic pleural effusion in a patient with granulomatous disease include Coxiella burnetii, Mycoplasma pneumoniae, Brucella species, Borrelia burgdorferi, Yersinia enterocolitica, Yersinia pseudotuberculosis and hepatitis viruses including hepatitis A, B and C.
Is pleural effusion present before splenectomy?
When reviewing the cross-sectional imaging taken during the patient’s acute surgical admission, it became apparent that a small pleural effusion was present before splenectomy ( figure 1D ). The lymphocyte-rich effusion was unlikely attributable to acute bacterial infection, indicating a more chronic process. Of note, the patient’s inflammatory markers had also fallen (C reactive protein currently 40 mg/L vs 221 mg/L at time of aspiration).
Is pleural fluid adenosine deaminase positive for TB?
TB pleuritis is an infrequent cause of a lymphocyte-rich effusion in the UK. Pleural fluid adenosine deaminase (pfADA) can be used in populations with low TB prevalence to exclude pleural TB. A prospective trial performed by Arnold et al concluded that pfADA<35 iU/L has a 99% specificity and 98.9% negative-predictive value in excluding TB in patients with lymphocyte-rich pleural effusions. 2 Raised pfADA can be found in empyema, complex parapneumonic effusion and in some cases of malignancy. However, these processes are associated with neutrophil predominance, as opposed to TB in which the effusion is lymphocyte-rich. In the same prospective trial, malignant effusions with high pfADA were found to be neutrophilic, with only a single lymphocyte-predominant false positive found. 2
Does pleural aspiration reveal lymphoma?
A repeated pleural aspiration underwent lymphocyte subset analysis and did not reveal any evidence of lymphoma.
Can sarcoidosis cause pleural effusions?
While the concurrent finding of granuloma may height en the clinical suspicion of sarcoidosis, it is extremely rare for sarcoidosis to cause clinically significant pleural effusions. It is therefore unlikely that this large pleural effusion is attributable to sarcoidosis, and we would only revisit sarcoidosis as a diagnosis once all other causes of granulomas with concurrent pleuritis have been excluded.
What are the side effects of pleural effusion?
Talk with your health care team about any symptoms you experience and any changes in symptoms. People with a pleural effusion may experience the following symptoms: Shortness of breath. Dry cough.
What is the pleural space?
A pleural effusion is a buildup of extra fluid in the space between the lungs and the chest wall. This area is called the pleural space. About half of people with cancer develop a pleural effusion. When cancer grows in the pleural space, it causes a malignant pleural effusion.
What is a temporary insertion of a catheter into the pleural space?
Temporary insertion of a catheter into the pleural space. You or your family member use the catheter to drain the fluid into a bottle as instructed by your doctor . Insertion of a shunt, which bypasses or diverts excess fluid from 1 place to another. Treating the cancer with chemotherapy to prevent the effusion from returning.
How to drain malignant fluid?
This may be done in several ways: Thoracentesis (see above) Tube thoracostomy, which uses a tube inserted into the chest for 24 hours to drain the fluid. This is usually followed by a process called pleurodesis.
What is the process of putting talc in the lung?
This is usually followed by a process called pleurodesis. This process uses substances, such as talc, to stick the edge of the lung to the chest wall. This decreases the chance that the fluid will return. Temporary insertion of a catheter into the pleural space.
Is pleural effusion a cancer?
Common causes of malignant pleural effusion are lymphoma and cancers of the breast, lung, and ovary. A malignant pleural effusion is treatable. But it can be a serious and potentially life-threatening condition.
Terminology
Epidemiology
- As the accumulation of fluid in the pleural space occurs in a broad range of disparate clinical scenarios, no single demographic is affected; rather the epidemiology will match that of the underlying condition. However, it is probably safe to say that as congestive cardiac failureand malignancy are some of the most common causes, older patients would be over-represented.
Clinical Presentation
- A small amount of fluid is completely asymptomatic. In fact, depending on the respiratory reserve of the patient, even large amounts of fluid can accumulate within the pleural space before any symptoms are recognized. Eventually as the volume of fluid increases, with resulting passive (relaxation) atelectasisof the adjacent lung, the patient will experience reduced exercise toleranc…
Pathology
- Physiologically, the pleural cavities normally contain approximately 15 mL of serous pleural fluid 6. Any process which results in more fluid forming than can be absorbed will produce a pleural effusion. There are many causes of pleural effusion that are broadly split into transudates and exudates. This categorization relies upon the biochemical analysis of aspirated pleural fluid 5: 1…
Radiographic Features
- Chest radiographs are the most commonly used examination to assess for the presence of pleural effusion; however, it should be noted that on a routine erect chest x-ray as much as 250-600 mL of fluid is required before it becomes evident 6. A lateral decubitus projection is most sensitive, able to identify even a small amount of fluid. At the other extreme, supine projectionsc…
Treatment and Prognosis
- The treatment of pleural effusions is usually targeted to the underlying condition (e.g. congestive cardiac failure or malignancy). Symptomatic patients with large effusions may be treated by therapeutic aspiration (thoracentesis). When effusions are very large, this can safely be done 'blind' although increasingly ultrasound is used to at least mark an appropriate site. Ultrasound-g…
Differential Diagnosis
- Imaging differential considerations include: 1. raised hemidiaphragm, e.g. hepatomegaly, phrenic nerve palsy 2. collapse or consolidation 3. pleural thickening, e.g. old tuberculosis or empyema 4. inferior pulmonary ligament 5. poor radiographic technique
Practical Points
- strange or atypical configurations of pleural fluid can be due to either adhesions (i.e. loculated effusion) or underlying atelectasis. The latter are more likely to change with patient positioning...
See Also