What does SIADH mean medically?
What is SIADH? The syndrome of inappropriate antidiuretic hormone secretion (SIADH) is characterised by excessive secretion of antidiuretic hormone (ADH) from the posterior pituitary gland or another source. ADH controls water reabsorption via its effect on kidney nephrons, causing the retention of water (but not the retention of solutes).
What can cause SIADH?
the body holds too much water. The blood becomes diluted and has a low blood sodium (salt) level. What causes SIADH? SIADH can be caused by: • Head trauma • Surgery • Stroke • Tumors • Meningitis • Pneumonia • Certain medicines • Viruses like HIV This condition may last for hours or days. What are the symptoms of SIADH?
What are symptoms of SIADH?
Symptoms of SIADH vary depending upon both the severity of the hyponatraemia and the rate at which it develops: Mild hyponatraemia: nausea, vomiting, headache, anorexia and lethargy. Moderate hyponatraemia: muscle cramps, weakness, confusion and ataxia. Severe hyponatraemia: drowsiness, seizures and coma.
What are the complications of SIADH?
- Euvolemia - SIADH
- Hypervolemia - Cardiac failure, cirrhosis
- Hypovolemia - Vomiting, diarrhea
What is the most common cause of SIADH?
The most common causes of SIADH are malignancy, pulmonary disorders, CNS disorders and medication; these are summarised in Table 3. SIADH was originally described by Bartter & Schwartz in two patients with lung carcinoma, who had severe hyponatraemia at presentation (29).
What conditions can cause SIADH?
What causes SIADH?Meningitis (inflammation of the meninges, the membranes that cover the brain and spinal cord)Encephalitis (inflammation of the brain)Brain tumors.Psychosis.Lung diseases.Head trauma.Guillain-Barré syndrome (a reversible condition that affects the nerves in the body. ... Certain medications.More items...
What is the most serious complication of SIADH?
A low sodium level or hyponatremia is a major complication of SIADH and is responsible for many of the symptoms of SIADH. Early symptoms may be mild and include cramping, nausea, and vomiting. In severe cases, SIADH can cause confusion, seizures, and coma.
Can SIADH be cured?
SIADH should be treated to cure symptoms. While this is undisputed in the presence of grave or advanced symptoms, the clinical role and the indications for treatment in the presence of mild to moderate symptoms are currently unclear.
Is SIADH life threatening?
Too much ADH leads to water retention, electrolyte imbalances and a low level of sodium in the blood (called hyponatremia or water intoxication). SIADH that develops suddenly can be life-threatening.
How do you fix SIADH?
Restrict fluid intake as first-line treatment. Second-line treatments include increasing solute intake with 0.25–0.50 g/kg per day of urea or a combination of low-dose loop diuretics and oral sodium chloride. Use of lithium, demeclocycline, or vasopressin receptor antagonists is not recommended.
What cancers does SIADH cause?
Approximately 67% of SIADH cases are reported to be caused by cancer, the majority of which (70%) are linked to small cell carcinoma of the lung (1). Head and neck cancers are responsible for only 1.5% of SIADH cases; however, the majority of these cases have the histology of small cell carcinoma (2).
What causes SIADH in elderly?
There are many causes of SIADH, such as central nervous system (CNS) disturbances, malignancies, surgery, pulmonary diseases, hormone deficiency and administration, HIV infection, hereditary SIADH, and drugs. In some cases, there is a chronic idiopathic SIADH, which is usually described in elderly patients3.
Are SIADH patients thirsty?
The principal drawback is that patients find it extremely difficult to maintain fluid restriction, as thirst in SIADH is inappropriately normal due to a downward resetting of the osmotic thirst threshold (15).
Do you pee with SIADH?
With SIADH, your pee is very concentrated, meaning there's a lot of waste product and not much water in it. Since your body doesn't release normal amounts of water through your pee, there's too much water in your blood. This dilutes many substances in your blood, such as sodium (salt).
What happens if SIADH is left untreated?
Symptoms tend to be mild at first and include cramps, muscle weakness, loss of appetite (not feeling hungry), irritability, and nausea and vomiting. The symptoms continue to become more serious if the SIADH is not treated. SIADH can lead to confusion, hallucinations, seizures, and even coma.
Can SIADH be caused by stress?
SIADH can also arise postoperatively from stress, pain, and medications used. However, not all hospital-acquired hyponatremia is SIADH and SIADH should be differentiated from the hyponatremia that occurs in patients with limited capacity to excrete free water, such as those with chronic kidney disease.
Which electrolyte disorder is most likely to trigger early symptoms of SIADH?
Symptoms of SIADH tend to be those related to the low sodium level in blood (hyponatremia. A low sodium level has many causes, including consumption of too many fluids, kidney failure, heart failure, cirrhosis, and use of diuretics... read more ) that accompanies it.
What causes SIADH in elderly?
There are many causes of SIADH, such as central nervous system (CNS) disturbances, malignancies, surgery, pulmonary diseases, hormone deficiency and administration, HIV infection, hereditary SIADH, and drugs. In some cases, there is a chronic idiopathic SIADH, which is usually described in elderly patients3.
Can SIADH be caused by stress?
SIADH can also arise postoperatively from stress, pain, and medications used. However, not all hospital-acquired hyponatremia is SIADH and SIADH should be differentiated from the hyponatremia that occurs in patients with limited capacity to excrete free water, such as those with chronic kidney disease.
Which malignancy is associated with SIADH?
The most common malignancy associated with SIADH was lung cancer, followed by colon cancer, lymphoma, breast cancer and pancreatic cancer. Most of the patients (73%) were diagnosed with malignancy associated SIADH while 27% had SIADH due to other etiologies.
What causes SIADH?
SIADH tends to occur in people with heart failure or people with a diseased hypothalamus (the part of the brain that works directly with the pituitary gland to produce hormones). In other cases, a certain cancer (elsewhere in the body) may produce the antidiuretic hormone, especially certain lung cancers. Other causes may include the following:
What are the symptoms of SIADH?
Each person may experience symptoms differently. Symptoms, in more severe cases of SIADH, may include:
What is the syndrome of inappropriate antidiuretic hormone secretion?
What is syndrome of inappropriate antidiuretic hormone secretion (SIADH)? Syndrome of inappropriate antidiuretic hormone secretion occurs when excessive levels of antidiuretic hormones (hormones that help the kidneys, and body, conserve the correct amount of water) are produced. The syndrome causes the body to retain water and certain levels ...
What is the treatment for SIADH?
The most commonly prescribed treatment for SIADH is fluid and water restriction. If the condition is chronic, fluid restriction may need to be permanent. Treatment may also include: Certain medications that inhibit the action of ADH (also called vasopressin) Surgical removal of a tumor that is producing ADH.
What tests are needed for SIADH?
In addition to a complete medical history and physical examination, to confirm diagnosis of SIADH, blood and urine tests will need to be performed to measure sodium, potassium, and osmolality (concentration of solution in the blood and urine).
What is the term for inflammation of the brain membranes?
Meningitis (inflammation of the meninges, the membranes that cover the brain and spinal cord) Encephalitis (inflammation of the brain) Brain tumors. Psychosis. Lung diseases. Head trauma. Guillain-Barré syndrome (a reversible condition that affects the nerves in the body.
What does SIADH stand for?
SIADH. Abbrev. for Syndrome of Inappropriate Antidiuretic Hormone. This is a condition in which excessive production of ADH (also known as vasopressin) by the PITUITARY GLAND results in water retention and low levels of sodium. The syndrome occurs in various serious diseases, especially cancer.
What does "adh" mean?
Abbrev. for Syndrome of Inappropriate Antidiuretic Hormone. This is a condition in which excessive production of ADH(also known as vasopressin) by the PITUITARY GLANDresults in water retention and low levels of sodium. The syndrome occurs in various serious diseases, especially cancer.
What is the syndrome of inappropriate antidiuretic hormone?
syndrome of inappropriate antidiuretic hormone (SIADH) a syndrome in which secretion of vasopressin (antidiuretic hormone) is not inhibited by hypotonicity of extracellular fluid and hyponatremia is produced. It occurs in conjunction with oat cell carcinoma of the lung and certain other malignant tumors and is caused by production ...
What is the syndrome of crocodile tears?
syndrome of crocodile tears spontaneous lacrimation occurring parallel with the normal salivation of eating. It follows facial paralysis and seems to be due to straying of the regenerating nerve fibers, some of those destined for the salivary glands going to the lacrimal glands. syndrome of inappropriate antidiuretic hormone (SIADH) ...
What is a combination of symptoms resulting from a single cause or so commonly occurring together as to constitute a?
a combination of symptoms resulting from a single cause or so commonly occurring together as to constitute a distinct clinical picture. For specific syndromes, see under the name, such as adrenogenital syndrome or reye's syndrome. See also disease and sickness.
Can reset osmostat be performed after SIADHare?
It should only be performed after other causes of SIADHare fully worked up and the diagnosis of reset osmostat is strongly suspected.
What are the different types of SIADH?
There are four types of SIADH: type A, B, C, and D . Type A occurs independently of plasma osmolality. There are high levels of ADH and urine osmolality. Type B is characterized by a constant release of ADH. Type C is characterized by a baseline plasma sodium concentration that is stable, but lower than normal. ...
Which genetic disorder is associated with SIADH?
Genetic syndromes such as nephrogenic syndrome and hypothalamic syndrome have been associated with SIADH. In nephrogenic syndrome, a gene mutation in the V2 receptor on the X chromosome, which is responsible for the reabsorption of water in the collecting ducts, is linked to SIADH.
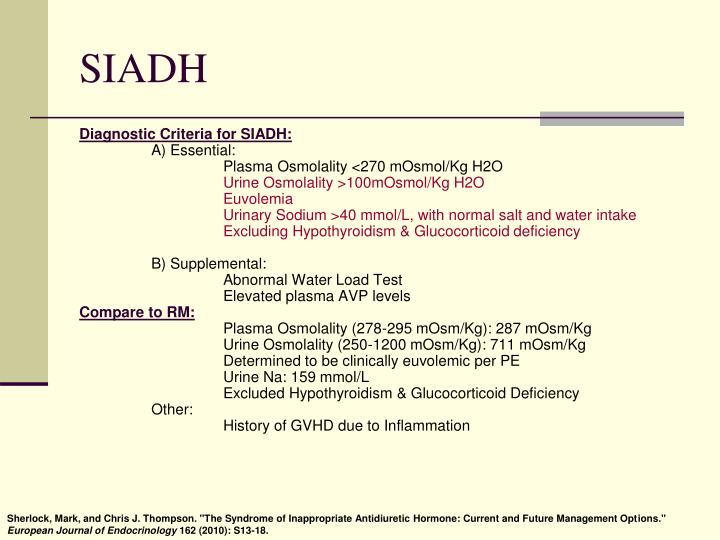
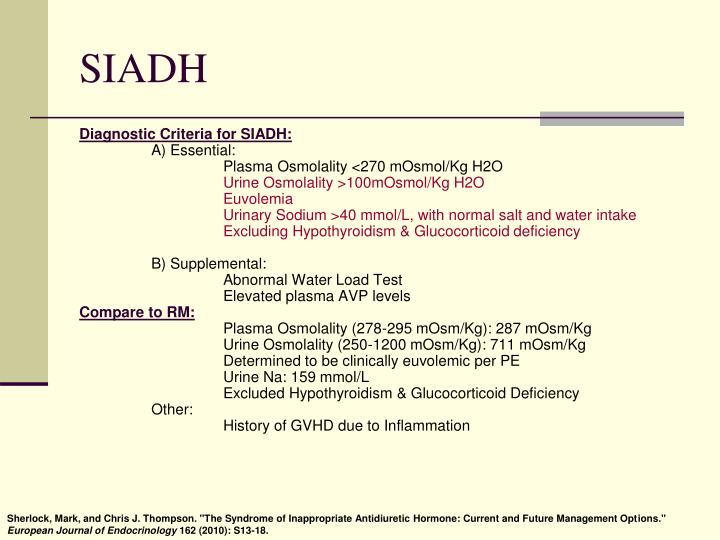
What are the criteria for SIADH?
A set of criteria was created in 1967 by William Schwartz and Frederic Bartter for the diagnosis of SIADH that are still in use today. These criteria are: 1 Serum sodium less than 135mEq/L 2 Serum osmolality less than 275 mOsm/kg 3 Urine sodium over 40 mEq/L 4 Urine osmolality over 100 mOsm/kg 5 No evidence of volume depletion 6 No evidence of other causes of low sodium levels, such as hyperthyroidism, cardiac failure, kidney disease, or pituitary gland problems 7 Sodium levels improve with fluid restriction.
What is the syndrome of inappropriate antidiuretic hormone secretion?
Syndrome of inappropriate antidiuretic hormone secretion (SIADH) is a condition in which there are high amounts of antidiuretic hormone (ADH) released from the pituitary gland or other sources. Image Credit: Yeexin Richelle/Shutterstock.com.
What causes low sodium levels in the blood?
Syndrome of inappropriate antidiuretic hormone secretion causes low sodium levels in the blood through excessive water retention. The extra water diluting the blood lowers the amounts of certain electrolytes in the blood and can cause serious symptoms such as seizures, coma, and psychological symptoms such as mood changes and hallucinations.
Where is antidiuretic hormone produced?
Antidiuretic hormone is also called arginine vasopressin (AVP). It is produced in the hypothalamus in the brain. ADH has been found to help to regulate the osmotic balance in the body, which refers to the amounts of electrolytes and non-electrolytes in the cells, tissues, and interstitial fluid. It also regulates sodium levels, blood pressure, ...
Why does dilute blood cause SIADH?
This leads to symptoms of SIADH, which occur because of the low levels of sodium in the blood.
What does SIADH cause?
SIADH makes it harder for your body to release water. Additionally, SIDAH causes levels of electrolytes, like sodium, to fall as a result of water retention. A low sodium level or hyponatremia is a major complication of SIADH and is responsible for many of the symptoms of SIADH. Early symptoms may be mild and include cramping, nausea, and vomiting. In severe cases, SIADH can cause confusion, seizures, and coma.
How to know if you have SIADH?
Early symptoms may be mild and include cramping, nausea, and vomiting. In severe cases, SIADH can cause confusion, seizures, and coma. Treatment usually begins with limiting fluid intake to prevent further buildup. Additional treatment will depend on the cause.
What is the next step after diagnosis of SIADH?
Following diagnosis of SIADH, the next step will be to identify the condition that caused it to occur.
What is the ADH test?
Blood tests, specifically one called an ADH test, can measure circulating ADH levels in the blood, but it’s very difficult to obtain an accurate level. According to the University of Rochester Medical Center, normal values for ADH range from 0-5 picograms per milliliter. Higher levels could be the result of SIADH. Most cases of SIADH are accurately diagnosed using serum and urine sodium and osmolality values as well as clinical presentation.
What is SIADH in the body?
Most commonly, SIADH occurs secondary to another disease process elsewhere in the body. Hereditary SIADH, also known as nephrogenic SIADH, has been ascribed to the gain of function mutation in vasopressin 2 (V2) receptors in the kidneys.
What is SIADH in education?
Continuing Education Activity. Syndrome of inappropriate antidiuretic hormone ADH release (SIADH) is a condition defined by the unsuppressed release of antidiuretic hormone (ADH) from the pituitary gland or nonpituitary sources or its continued action on vasopressin receptors. The condition was first detected in two patients with lung cancer by ...
How does ADH work?
A decrease in tonicity prevents ADH release and prevents water retention. An increase in tonicity causes ADH release, which acts on V2 receptors on the luminal surface of cortical and medullary collecting tubular cells. Under the influence of ADH, unique aquaporin-2 water channels are formed by the fusion of pre-formed cytoplasmic vesicles in the tubular cells, and water is absorbed down the concentration gradient. Once the water is absorbed, these channels are removed by endocytosis and returned to the cytoplasm. The osmoreceptors are extremely sensitive, responding to alterations in the plasma tonicity of as little as 1%.[6] The osmotic threshold for ADH release in humans is about 280 to 290 mOsmol/kg. There is little circulating ADH below this level, and the urine should be maximally diluted with an osmolality below 100 mOsmol/kg. Above the osmotic threshold, there is a relatively linear rise in ADH secretion. This system is so efficient that the plasma osmolality does not typically vary by more than 1% to 2%, despite wide water intake fluctuations. [7]
What is the name of the condition that is caused by the release of antidiuretic hormones?
Syndrome of inappropriate antidiuretic hormone ADH release (SIADH) is a condition defined by the unsuppressed release of antidiuretic hormone (ADH) from the pituitary gland or nonpituitary sources or its continued action on vasopressin receptors. The condition was first detected in two patients with lung cancer by William Schwartz and Frederic Bartter in 1967. They developed the classic Schwartz and Bartter criteria for the diagnosis of SIADH, which has not changed. SIADH is characterized by impaired water excretion leading to hyponatremia with hypervolemia or euvolemia.[1][2][3]
Why is SIADH more prevalent in hospitalized patients?
SIADH is also more prevalent in hospitalized, post-operative patients due to the administration of hypotonic fluids, drugs, and the body's response to stress.
Where is ADH stored?
ADH, also known as arginine vasopressin, is formed in the hypothalamus and stored in the posterior pituitary via a pituitary stalk. The main function of ADH is osmoregulation. However, a severe reduction in effective blood volume shifts the function of ADH to volume regulation, even at the expense of effective plasma osmolality or tonicity. "Plasma osmolality" should be differentiated from "effective plasma osmolality" or "plasma tonicity," as the latter is determined by effective osmoles in the extracellular fluid (ECF) such as sodium (which is not freely permeable across cell membranes), the main component of the ECF. Glucose and urea also increase the plasma osmolality, but these are ineffective osmoles as they are freely permeable across the cell membranes and do not take part in maintaining plasma tonicity.
Who discovered SIADH?
The condition was first detected in two patients with lung cancer by William Schwartz and Frederic Bartter in 1967. They developed the classic Schwartz and Bartter criteria for the diagnosis of SIADH, which has not changed. SIADH is characterized by impaired water excretion leading to hyponatremia with hypervolemia or euvolemia.[1][2][3] ...
What is the name of the condition where the body makes too much antidiuretic hormone?
Syndrome of inappropriate antidiuretic hormone secretion (SIADH) is a condition in which the body makes too much antidiuretic hormone (ADH). This hormone helps the kidneys control the amount of water your body loses through the urine. SIADH causes the body to retain too much water.
How to treat ADH?
Treatment depends on the cause of the problem. For example, surgery is done to remove a tumor producing ADH. Or, if a medicine is the cause, its dosage may be changed or another medicine may be tried.
What are the situations where ADH is released into the blood when it should not be produced?
Common situations when ADH is released into the blood when it should not be produced (inappropriate) include: Medicines, such as certain type 2 diabetes drugs, seizure drugs, antidepressants, heart and blood pressure drugs, cancer drugs, anesthesia. Surgery under general anesthesia. Disorders of the brain, such as injury, infections, stroke.
Can too much ADH cause low sodium?
This dilutes many substances in the blood such as sodium. A low blood sodium level is the most common cause of symptoms of too much ADH. Often, there are no symptoms from a low sodium level. The health care provider will perform a complete physical examination to help determine the cause of your symptoms.
What is SIADH?
SIADH is a syndrome of inappropriate antidiuretic hormone secretion. Things that cause SIADH include infections, asthma, brain inflammation, certain medications, hereditary factors and other factors.
What are the symptoms of SIADH?
What are the signs and symptoms of SIADH? 1 Irritability and restlessness 2 Loss of appetite 3 Muscle cramps 4 Muscle weakness 5 Nausea and vomiting 6 Mental confusion 7 Memory problems 8 Headache 9 Changes in personality 10 Depression 11 Tremors 12 Hallucinations (experiencing things that are not present) 13 Seizures 14 Stupor (a serious mental state where people don't respond to conversation and only to physical stimulation, such as to pain or rubbing on their chest) 15 Coma
What is the treatment and prognosis for SIADH?
The underlying medical conditions triggering SIADH would also be treated. The prognosis will depend on the cause of SIADH. If untreated, it can lead to respiratory failure, coma and death.
What is the name of the syndrome of inappropriate antidiuretic hormone secretion?
SIADH is the syndrome of inappropriate antidiuretic hormone secretion. It is a rare condition in which the body makes too much antidiuretic hormone (ADH), resulting in water retention in the body and decreased sodium levels in the blood. Antidiuretic hormone (ADH), also called vasopressin, is produced in the brain by the hypothalamus gland.
Why is ADH important?
ADH hormone helps kidneys conserve the correct amount of water in the body, hence regulating the way the body eliminates and conserves water. When ADH is produced in excess, it results in SIADH. SIADH can be due to a problem in the hypothalamus or other causes and triggers. It can occur at any age and is seen more often in children.
What is the condition of low sodium in the body called?
Water retention in the body leads to decreased levels of electrolytes, such as sodium. The condition of low sodium levels in the body is called hyponatremia. Hyponatremia is responsible for many of the symptoms of SIADH and can result in serious complications.
What is the name of the condition in which the immune system attacks the nerves?
Injury to the head. Hydrocephalus (fluid accumulation in the brain) Guillain-Barre syndrome (a condition in which the immune system attacks the nerves) Multiple sclerosis (a disease in which the immune system damages the protective covering of nerves)
What is the pattern of ADH in SIADH?
Several different observations have been made. First, the pattern of ADH secretion in SIADH may show variations that are independent of prevailing serum osmolality (type A) [Robertson, 2006], it may exhibit steady elevation regardless of serum osmolality (type B), or it may show a rather normal looking curve that is shifted to the left (type C, also termed ‘reset osmostat’) [Robertson, 2006; Hoorn et al. 2008]. The different patterns may not just be academic exercises. For example, when patients with reset osmostat (type C) have their hyponatremia corrected they can develop exceptional thirst and this in turn may become a therapeutic obstacle. However, patients with type C SIADH are able to suppress ADH secretion once they reach their left-shifted setpoint of osmolality; this will allow them to excrete water and hence their degree of hyponatremia will be limited to the value corresponding to the osmotic setpoint. The secretory patterns do not show any specific relationship to underlying pathology [Berl and Robertson, 2000].
What is the absence of edematous disease?
Absence of edematous disease (cardiac failure, liver cirrhosis, nephrotic syndrome) and of plasma volume depletion (i.e. absence of pathologic orthostatic changes, low internal jugular venous pulses, dryness of axillae)
Is SIADH missed?
Recent publications have indicated that the diagnosis of SIADH is often missed or made erroneously [Fenske et al. 2010; Hoorn et al. 2006; Huda et al. 2006]. One should carefully follow the steps of differential diagnosis (Figure 1). Clinicians must resist the temptation to take shortcuts because this may result in misdiagnosis. If clinical circumstances dictate an urgent intervention despite available data being incomplete, clinicians should go ahead but review their working diagnosis as soon as all lab data have been reported back.
Is there antidiuretic hormone in plasma?
Third, in scientific measurements of ADH obtained from patients with SIADH it was found that a small percentage showed no detectable antidiuretic hormone in the plasma. While one possible explanation for this may be related to technical limitations inherent in the available vasopressin assays, recent work has indicated another possible explanation. In some studies it was suggested that gain-of-function mutations of the renal hydro-osmotic vasopressin V-2 receptor exist in some patients, accounting for the clinical features of SIADH without ADH being instrumental in this abnormality [Decaux et al. 2007; Feldmann et al. 2005; Levtchenko and Monnens, 2010].
Is hyponatremia a clinical condition?
However, a much more common clinical situation is that of mild hyponatremia (arbitrarily defined as a serum sodium concentration of 128–134 mmol/liter), in which any associated symptoms may be modest, indistinct, and nonspecific. Many of these patients show symptoms such as forgetfulness, poor concentration, depressed mood, etc., but since they are often older patients the physician has great difficulty attributing the symptomatology to hyponatremia rather than to cerebral sclerosis, social depravation, clinical depression, poor general health, or similar common diagnoses. There are currently no bedside tests that would allow one to distinguish between hyponatremia and other etiologies causing such symptoms. This poses a frequent clinical dilemma. In my experience it is helpful in these cases to give a short trial of treatment to correct or improve hyponatremia. Patients’ symptomatology should be watched closely for any improvements – whether they become more alert and cooperative, concentrate better and are less confused, walk better and fall less, etc. – to appreciate the role of hyponatremia. They should be treated for 3 or 4 days using vaptan tablets or urea powder dissolved in orange juice (see below, section on treatment).
Does cyclophosphamide have low ADH?
Second, measurement of ADH in patients with SIADH receiving agents such as carbamazepine, cyclophosphamide or others [Gold et al. 1983] may yield low concentrations of ADH. This has been attributed to direct tubular actions of these drugs [de Braganca et al. 2010], resulting in enhancement of water reabsorption that is not exclusively mediated by ADH. In other words, such patients have typical features of SIADH, but they fail to exhibit inadequate ADH secretion.
Is hyponatremia asymptomatic or nonspecific?
Not only are hyponatremic symptoms often nonspecific and indistinct, there are other cases of mild hyponatremia that seem to be asymptomatic altogether. Renneboog and colleagues studied apparently asymptomatic patients using neurocognitive measurements. The tests were performed twice, once in hyponatremia and then again after it had been corrected [Renneboog et al. 2006]. It was found that chronic ‘asymptomatic’ hyponatremia (126–128 mmol/liter) caused significant reduction (by 10–20%) in the ability to concentrate, memorize, and calculate. In addition, balance and stability of gait were significantly better in normonatremia than in hyponatremia [Renneboog et al. 2006]. This work suggests that ‘asymptomatic hyponatremia’ causes more changes than we realize [Decaux, 2006]. However, in the absence of prospective interventional studies, it does not help to answer the question of whether ‘asymptomatic’ hyponatremia should be treated – or simply observed.
