What is a necrotizing granuloma?
Necrotizing granuloma. A granuloma is a clump of cells that forms when the immune system tries to fight off a harmful substance but cannot remove it from the body. A necrotizing granuloma is an area of inflammation in which tissue has died. Necrotizing means dying or decaying.
What is the study of non-necrotizing granulomatous inflammation?
The study of Non-necrotizing Granulomatous Inflammation has been mentioned in research publications which can be found using our bioinformatics tool below. Researched pathways related to Non-necrotizing Granulomatous Inflammation include Granuloma Formation, Hypersensitivity, Pathogenesis, Immune Response, Cytokine Production.
What is granulomatous inflammation?
Granulomatous inflammation is a distinctive pattern of chronic inflammatory infiltrate in which the predominant cell type is an activated macrophage. A granuloma is a microscopic focus of inflammation characterized by a collection of modified epithelial-like (epithelioid) macrophages (Figure 84.3 ).
What is the prevalence of non-necrotizing epithelioid granulomas?
Granulomatous inflammation is observed in many drug-associated injuries92 ( Table 12.10 ). Non-necrotizing epithelioid granulomas were seen in about 5% of cases from the DILIN series. 50 Granulomas may be seen alone or associated with other types of hepatic injury ( Fig. 12.10 ), including acute and chronic hepatitis, cholestasis and steatosis.

How do you treat necrotizing granulomatous inflammation?
Treatment may include continuous antibiotic therapy, such as trimethoprim and sulfamethoxazole combination (Bactrim, Sulfatrim Pediatric) to protect against bacterial infections, and itraconazole (Sporanox, Tolsura) to prevent fungal infection.
Is granulomatous inflammation cancerous?
A granuloma is a tiny cluster of white blood cells and other tissue that can be found in the lungs, head, skin or other parts of the body in some people. Granulomas are not cancerous. They form as a reaction to infections, inflammation, irritants or foreign objects.
What does granulomatous inflammation mean?
Granulomatous inflammation is a histologic pattern of tissue reaction which appears following cell injury. Granulomatous inflammation is caused by a variety of conditions including infection, autoimmune, toxic, allergic, drug, and neoplastic conditions.
What diseases have granulomatous inflammation?
Granulomatous inflammation of muscle is usually associated with sarcoidosis but can also be seen in infectious disease, inflammatory bowel disease, foreign body reactions, thymoma, lymphoma, and myasthenia gravis. It may also occur without any evidence of systemic disease.
Can granulomas turn cancerous?
Calcified granulomas are almost always benign. However, less commonly, they can become surrounded by a cancer tumor.
How serious is granulomatous disease?
Chronic granulomatous disease, or C-G-D, is a rare disease that about 20 children are born with every year in the United States. People with CGD have an immune system that doesn't work properly, so they are at more of a risk of getting serious, life-threatening infections that lead to hospitalization.
Can granulomatous inflammation be cured?
Researchers don't know the exact cause, but they think granulomas form when your immune system tries to fight off harmful infections, chemicals, or sometimes your body's own proteins. There's no cure, but you can usually manage it with little or no treatment.
Can you live with granulomatous disease?
Survival rates are variable but improving; approximately 50% of patients survive to age 30-40 years. Infections are less common in adults than in children, but the propensity for severe life-threatening bacterial infections persists throughout life.
What doctor treats granulomatous disease?
Chronic granulomatous disease (CGD) specialists, usually immunologists, infectious disease physicians, hematologists, and oncologists, have expertise in treating CGD.
What bacteria causes granulomatous inflammation?
Mycobacteria and fungi are commonly associated with granulomatous infection, and in particular,tuberculosis is the most common cause of granulomas worldwide. However, all mycobacteria can be associated with granulomas.
What autoimmune diseases cause granulomas?
One of the most important evidence of the autoimmune inflammation in sarcoidosis is the formation of granulomas, mainly in the lungs and the mediastinal lymph nodes as well as in the skin and liver of patients.
Can granulomas go away?
In most cases, skin granulomas will go away on their own without treatment. Sometimes, though, they might come back. Underlying health conditions can also cause granulomas. When this is the case, doctors will focus on treating the underlying cause of the lumps.
Are granulomas benign?
A granuloma is a small area of inflammation. Granulomas are often found incidentally on an X-ray or other imaging test done for a different reason. Typically, granulomas are noncancerous (benign). Granulomas frequently occur in the lungs, but can occur in other parts of the body and head as well.
Is a granuloma a lesion?
Granuloma annulare is a skin condition that causes a raised rash or bumps (lesions) in a ring pattern, usually on the hands and feet. Granuloma annulare (gran-u-LOW-muh an-u-LAR-e) is a skin condition that causes a raised rash or bumps (lesions) in a ring pattern.
What is positive malignancy?
A “positive” or “involved” margin means there are cancer cells in the margin. This means that it is likely that cancerous cells are still in the body. Lymph nodes. The pathologist will also note whether the cancer has spread to nearby lymph nodes or other organs.
What does negative for malignancy mean?
A Pap test finding that means no cancer cells or other abnormal cells have been found on the surface of or in the tissue that lines the cervix. Cell changes that suggest inflammation or infection may be included in this finding.
Is necrotizing vasculitis infectious?
These need to be distinguished from other granulomatous processes such as Wegener’s granulomatosis (WG). Although there may be histological overlap between these different processes, the identification of a true necrotizing vasculitis is specific to WG in the context of necrotizing granulomas. Otherwise, the combination of histological features should lead to a specific diagnosis. Despite a thorough histological examination and assessments of special stains, a significant proportion of necrotizing granulomas will appear infectious with no obvious infectious etiology. There are only few clinically available ancillary tests that can be performed on paraffin-embedded tissue and include real-time PCR for tuberculous mycobacteria. Despite correlation with clinical, serological and other microbiological studies, some necrotizing granulomas remain unexplained. Patients with such granulomas appear not to require any additional treatment and do experience a favorable outcome.
Do granulomas require additional treatment?
Patients with such granulomas appear not to require any additional treatment and do experience a favorable outcome. AB - Necrotizing granulomas are commonly encountered in surgically resected specimens. The majority will be proven infectious with special stains for microorganisms.
What is a necrotizing granuloma?
Necrotizing granulomas are commonly encountered in surgically resected specimens. The majority will be proven infectious with special stains for microorganisms. These need to be distinguished from other granulomatous processes such as Wegener's granulomatosis (WG). Although there may be histological overlap between these different processes, ...
What is the significance of necrotizing granuloma that looks infectious but in which no organism is identified?
To answer this question, one needs to first answer the following: what is the significance of finding necrotizing granulomas in a resected lung specimen? Ulbright and Katzenstein 1 looked at 86 consecutive necrotizing granulomas presenting as single nodules. They found that 61 (71%) were proven infectious, 3 (3%) were diagnosed as WG (1) and hyalinizing granuloma (2), and 22 (26%) remained unexplained after clinical, radiological and microbiological correlation. In our practice (data not published), about half of necrotizing granulomas with negative special stains for microorganisms are infectious in etiology, 13% have another specific diagnosis and the number of unexplained necrotizing granulomas remains high at 39% (series of 132 patients). This leads us to pose the second question.
What features are most helpful in separating infectious granulomatous disease from other lesions such as WG?
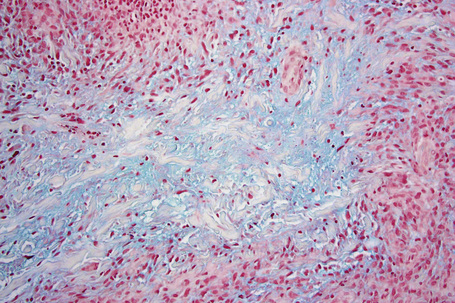
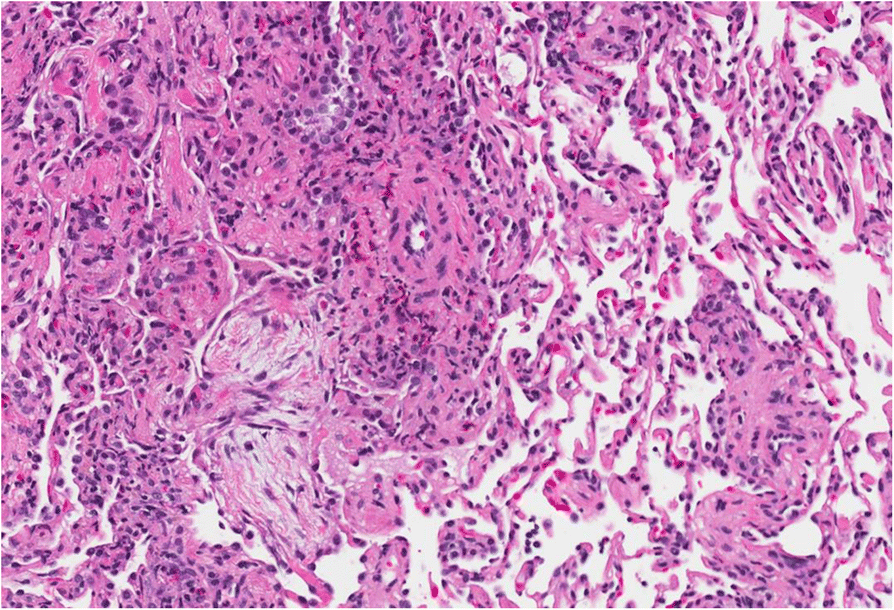
There are features that distinguish infectious granulomas from these other entities. However, overlapping features may cause diagnostic challenge and it is the combination of multiple histological findings that typically leads to the final diagnosis 2 ( Table 1 ). Infectious necrotizing granuloma usually has regular contours with mostly eosinophilic necrosis, surrounded by a rim of epithelioid histiocytes, often with multinucleated giant cells 2 ( Figure 1 ). However, in some cases, the contour of the necrosis may be more irregular ( Figure 2a ). Furthermore, the necrosis may take on different morphological aspect. It may be suppurative and rich in neutrophils, which may become necrotic and necrosis appear ‘dirty’ as seen in WG ( Figure 2a) or it may be coagulative and mimics the necrosis seen in arterial infarcts ( Figure 2b ). Vascular inflammation (‘vasculitis’) can be seen in infectious granulomas, usually chronic inflammatory cells with or without granulomas ( Figure 3 ). However, a true necrotizing vasculitis characterized by fibrinoid necrosis of the media associated with necrotic neutrophils is not seen and is a specific feature of a true vasculitis such as WG. In contrast, WG is described by geographic necrosis, ie necrosis with irregular contours, and necrosis that is ‘dirty’ due to the intense necrosis of neutrophils with nuclear debris 3 ( Figure 4a ). The necrosis is surrounded by a rim of palisading histiocytes and giant cells are common, often scattered, with hyperchromatic nuclei ( Figure 4b ). Furthermore, true necrotizing vasculitis is a distinctive feature ( Figure 4c ). Vessels located within the center of necrotic areas will exhibit true necrosis of their wall, however, these findings are seen in any necrotic process and are not diagnostic of a necrotizing vasculitis. In order to make this diagnosis, vessels more peripheral to the necrosis need to be assessed and an elastic stain such as Verhoeff von Gieson may be helpful. Features that can also assist in distinguishing infectious necrotizing granulomas from WG are the presence of non-necrotizing granulomas and lymph node involvement by granulomatous inflammation seen in infection and typically not in WG. NSG is a rare entity, considered as a variant of sarcoidosis 4 ( Figure 5 ). It shares overlapping features with infectious granulomas and WG. Indeed, parenchymal necrosis is typical of NSG and the morphological appearance is variable, usually described as eosinophilic but may also be basophilic with nuclear debris. However, this necrosis occurs in a background of non-necrotizing granulomas as seen in sarcoidosis with granulomas displaying a lymphangitic distribution and being well-formed, composed predominantly of epithelioid histiocytes and giant cells with few intervening lymphocytes or other inflammatory cells. In NSG, these granulomas tend to be confluent and prominently involve vessels but without resulting in a true necrotizing vasculitis. As infectious necrotizing granulomas may exhibit coagulative type necrosis, another important differential diagnosis is arterial infarct ( Figure 6 ), particularly in a small biopsy specimen where sampling may be an issue. 5 Furthermore, infarcts as they organize may be surrounded by a rim of fibroblasts and inflammatory cells which can mimic granulomatous inflammation and described as ‘pseudo granulomatous’. In a study of wedge resection specimens, arterial thrombosis was seen in all cases of infarcts, a feature that would distinguish infarct from infectious necrotizing granuloma. 5
Is necrotizing vasculitis a characteristic feature?
Furthermore, true necrotizing vasculitis is a distinctive feature ( Figure 4c ). Vessels located within the center of necrotic areas will exhibit true necrosis of their wall, however, these findings are seen in any necrotic process and are not diagnostic of a necrotizing vasculitis.
Is necrotizing granuloma irregular?
Infectious necrotizing granuloma usually has regular contours with mostly eosinophilic necrosis, surrounded by a rim of epithelioid histiocytes, often with multinucleated giant cells 2 ( Figure 1 ). However, in some cases, the contour of the necrosis may be more irregular ( Figure 2a ). Furthermore, the necrosis may take on different morphological ...
Can fungi be detected with high magnification?
Detect ing these rare fungi requires more than a cursory scanning at low power and confirmation often needs to be performed at high magnification. Re-examination of stains is also useful and can increase detection of Histoplasma in up to 90% of cases. 1 Mycobacteria are also often few and difficult to find.
Can fungi be seen on H&E slides?
Many fungi such as Cryptococcus, Blastomyces, Coccidioides and Aspergillus can be seen on H&E, preferentially in the area of necrosis rather than the surrounding viable area. 6 When assessing special stains, necrosis should be present on the slides, as this is the area where organisms are likely to be.
What is necrotizing granulomas?
Granulomatous inflammation with (usually central) necrosis is referred to as necrotizing. This term is not precisely synonymous with caseating, although it is often used as such. If used accurately, the term “caseous” applies only to the gross pathologic cheeselike appearance of several necrotic lesions, including granulomas or neoplasms. There is no defined microscopic appearance that corresponds to the gross appearance of caseation; however, it usually has an eosinophilic granular quality and tends to destroy the underlying parenchymal architecture. Most necrotizing granulomas are caused by infection. Cultures should be sent at the time of surgery (either by the surgeon or by the pathologist after identification of a gross lesion). When confronted by necrotizing granulomas, staining for fungus and staining for acid-fast bacilli should be performed. Grocott methenamine silver stain is preferred for fungi because the periodic acid–Schiff stain tends not to stain two common lung pathogens: Pneumocystis jiroveci and Histoplasma capsulatum. In a study of solitary necrotizing granulomas, El-Zammar and Katzenstein 23 noted that in cases of tuberculosis (as well as histoplasmosis) the organisms were identified only in the central necrotic portions of the granuloma. In other fungal diseases, the organisms were more randomly distributed throughout the granuloma. This information is helpful, as the biggest deterrent to identification of microorganisms on special stains is time. If the lesions appear suspect for infection, two or more blocks should be stained for microorganisms; however, pathologists should not perform stains on more blocks than they have time to carefully examine. The absence of identifiable organisms is not equivalent to the absence of infectious disease, and all cases should be correlated with clinical data and microbiologic cultures.
What is granulomatous inflammation?
Granulomatous inflammation is a type of chronic inflammation characterized by immunologically modified macrophages that are better suited to containment of organisms and large-particle phagocytosis than to intracellular killing and that tend to occur when there is absence of efficient intracellular killing of microorganisms.47 The term granuloma is used to describe the aggregation of these modified macrophages into nodular aggregates. Lymphocytes and plasma cells are also seen, usually at the periphery of granulomas. In cytologic preparations, the transformed macrophages of granulomas have elongate oval to boomerang-shaped nuclei and abundant, finely granular cytoplasm that is pink in H&E-stained slides and cyanophilic in Papanicolaou. The cytoplasmic borders are not well defined, and adjacent cells blend into one another. The cells bear some resemblance to epithelial cells and are called epithelioid macrophages. Multinucleated giant cells are often seen but not essential for the diagnosis of granuloma. Two FNA preparations showing noncaseating granulomatous inflammation are illustrated in Figure 4-23. The Papanicolaou-stained sample derives from a cervical lymph node in a 33-year-old man who had sarcoidosis. The Romanovski-stained preparation was taken from a lymph node FNA in a woman with tuberculosis and widespread lymphadenopathy. Noncaseating granulomas found in a lymph-node or visceral-organ FNA from an asymptomatic young person frequently indicates sarcoidosis; however, one must not be complacent. One cannot distinguish between sarcoidosis and infectious causes of noncaseating granulomas on the basis of morphology. Always culture the sample, and be sure that the clinician is aware of the patient's clinical and radiologic findings. Figure 4-24 is taken from a tonsil biopsy of the man with sarcoid. It is easy to see why the term “epithelioid cells” is appropriate!
How are granulomas formed in sarcoidosis?
The granulomas of sarcoidosis are well formed in that the epithelioid and giant cells are compact with sharp circumscription from the surrounding tissue. The granulomas usually exhibit a uniform appearance suggesting formation at a single point in time. Early, cellular granulomas become replaced by more fibrotic, hyalinized lesions as the disease progresses. Small central foci of amorphous granular debris (necrosis) may be seen in up to one-third of open lung biopsies in patients with sarcoidosis. Collections of neutrophils (suppuration) and confluent foci of necrosis are usually absent. Abundant necrosis is very unusual for typical sarcoidosis and should alert the clinician to exclude infection. The terms “caseating” and “noncaseating” are often used to describe granulomatous inflammation. Caseation refers to the white, cheesy gross appearance of tissue necrosis most commonly seen in foci of tuberculous infection. Caseation has been used interchangeably with the microscopic description of necrosis and, as described above, should be absent in sarcoidosis.
Is granulomatous sarcoidosis a systemic disease?
Granulomatous inflammation of muscle is usually associated with sarcoidosis but can also be seen in infectious disease,148 inflammatory bowel disease, foreign body reactions, 149 thymoma, 150 lymphoma, 151 and myasthenia gravis. It may also occur without any evidence of systemic disease.
Is granulomatous inflammation necessary for sarcoidosis?
Granulomatous inflammation is necessary to establish a diagnosis of sarcoidosis in most cases; however, the finding of granulomas is not sufficient for the diagnosis of sarcoidosis (Fig. 66-10 ). 1,64 Meticulous histologic examination with appropriate staining of all biopsy specimens should be performed to search for known causes of granulomatous inflammation, such as mycobacteria, fungi, parasites, and foreign material (e.g., talc).
Is necrosis absent in sarcoidosis?
Collections of neutrophils (suppuration) and confluent foci of necrosis are usually absent. Abundant necrosis is very unusual for typical sarcoidosis and should alert the clinician to exclude infection. The terms “caseating” and “noncaseating” are often used to describe granulomatous inflammation.
Is uveal inflammatory or non-inflammatory?
The uveal tract usually shows a reactive, chronic nongranulomatous inflammatory reaction . Sometimes, however, the same trauma that ruptures the lens and sets off the PE initiates a sympathetic uveitis and results in a diffuse, chronic, granulomatous inflammation.
What is Granulomatous Inflammation?
A granuloma refers to a benign inflammatory condition that is composed of small, organized collections of activated macrophages or histiocytes and multinucleated giant cells which take on a squamous cell-like manifestation. This distinctive pattern is so organized in a tight, ball-like structure that the margins of the individual cells are hard to outline. It is not a granuloma when macrophages are slackly diffused. This massing of macrophages bordered by the lymphocytes looks like epithelial cells, thus the term epitheloid cells.
How to treat granulomatosis?
For localized inflammation with no systemic association, lesions can be dealt by applying conservative surgical removal and reconstruction. Before the operation, the patient is given with a number of drugs with unpredictable outcomes. Some of these include intralesional and systemic steroidal medications, radiotherapy in low dose, and sulfasalazine.
How to manage granulomatous disease?
To successfully manage the granulomatous disease, the mainstay of the disease management consists of aggressive neurosurgical measures to surgically eliminate Aspergillus abscesses and granulomatous inflammations, modification to decrease the effect of predisposing and precipitating factors, administration of amphotericin B in conjunction with flucytosine, and treatment of the cause of infection.
Why are granulomas formed?
The distinction of granulomas from other types of inflammation is the concept that the former is formed because the causative agents are impervious to the first line of special defense cells including the neutrophils and eosinophils. Most frequently, the inciting antigen involved in the development of granulomas is an infectious microorganism or an inorganic material extraneous to the body. In some cases however, such as in sarcoidosis, the main culprit which stimulates the antibody production is not yet recognized.
What is the massing of macrophages bordered by the lymphocytes?
This massing of macrophages bordered by the lymphocytes looks like epithelial cells, thus the term epitheloid cells. This characteristic lesion is formed the moment the immune system tries to isolate an infectious or non-infectious substance which is distinguished as foreign but is not capable of getting rid of it.
How small is granulomatous mass?
Symptoms. In general; The mass of granulation tissue is classically small, 1 to 2-millimeter-lesion. The amount of pain is influenced by the location of the granulomatous inflammation. In a few instances, affected individuals do not experience pain at all or even any physical indications of inflammation. Below are some of the familiar causes of ...
Is granuloma asymptomatic or asymptomatic?
Characteristically, a granuloma takes in merely a trivial segment of the body tissue. On the whole, affected individuals are asymptomatic. In point of fact, most of the granuloma cases are identified by chance via an x-ray performed for a different purpose. Oftentimes, when discovered in an x-ray, these inflammations are being confused with cancer.
Non-necrotizing Granulomatous Inflammation Bioinformatics Tool
Laverne is a handy bioinformatics tool to help facilitate scientific exploration of related genes, diseases and pathways based on co-citations. Explore more on Non-necrotizing Granulomatous Inflammation below! For more information on how to use Laverne, please read the How to Guide.
Top Research Reagents
We have 2526 products for the study of Non-necrotizing Granulomatous Inflammation that can be applied to Chromatin Immunoprecipitation, Chromatin Immunoprecipitation (ChIP), Flow Cytometry, Immunocytochemistry/Immunofluorescence, Immunohistochemistry, Western Blot from our catalog of antibodies and ELISA kits.