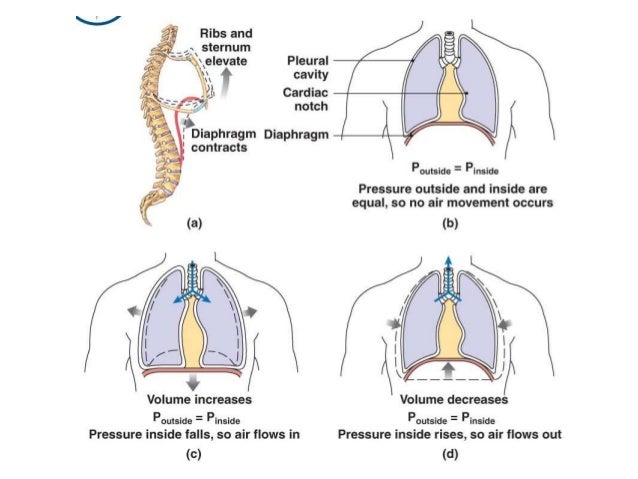
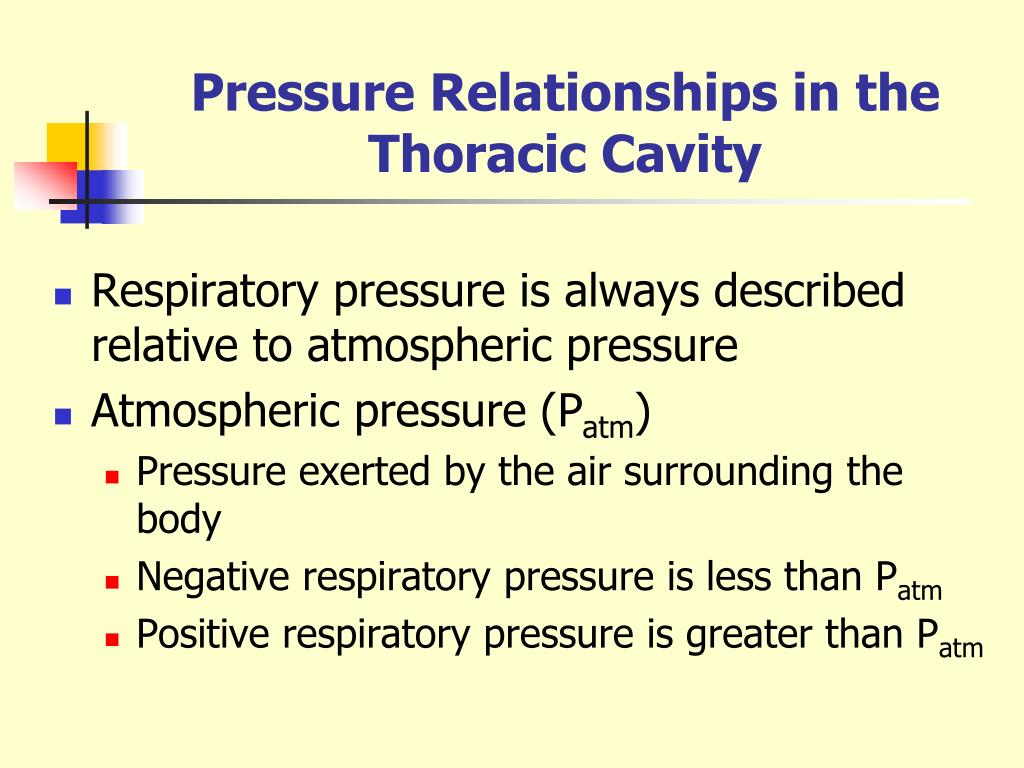
When you inhale, the diaphragm and muscles between your ribs contract, creating a negative pressure—or vacuum—inside your chest cavity. The negative pressure draws the air that you breathe into your lungs. What is negative pressure in the thoracic cavity? The diaphragm moves down at the same time, creating negative pressure within the thorax.
Why is there negative pressure in the lungs?
The lungs are held to the thoracic wall by the pleural membranes, and so expand outwards as well. This creates negative pressure within the lungs, and so air rushes in through the upper and lower airways. How is negative pressure created? .
Is intrapleural pressure positive or negative?
In physiology, intrapleural pressure refers to the pressure within the pleural cavity. Normally, the pressure within the pleural cavity is slightly less than the atmospheric pressure, which is known as negative pressure. Is normal breathing negative pressure? The pressure inside the lungs drops. The negative pressure sucks air in. For us humans, .
What is negative pressure breathing (NPB)?
The negative pressure breathing (NPB) is created by more hydrostatic pressure creating more transpulmonary pressure difference that results in NPB. NPB occurs generally at the time of swimming when the air pressure is lesser than the hydrostatic pressure around the thoracic region and abdominal cavity.
What is the normal intrathoracic pressure during obstructive apnea?
Negative intrathoracic pressures as high as 60 to 80 cm H 2 O may be generated during episodes of obstructive apnea. After central apnea, hyperpnea occurs, and relatively large negative pressure deflections, particularly in the presence of stiff lungs and chest wall, may also be observed.
Does the thoracic cavity have negative pressure?
There is always a slightly negative pressure within the thoracic cavity, which aids in keeping the airways of the lungs open. During inhalation, volume increases as a result of contraction of the diaphragm, and pressure decreases (according to Boyle's Law).
Why is negative pressure within the thoracic cavity important?
The negative pressure of the pleural cavity acts as a suction to keep the lungs from collapsing. Damage to the pleura could disrupt this system, resulting in a pneumothorax.
What occurs in response to negative pressure in the thoracic cavity?
The body generates negative-pressure in the chest cavity during breathing by the contraction of the diaphragm muscle (it pulls downward, expanding the thoracic cavity size and space for the lungs to fill), and the outward expansion of the ribcage (which also expands the thoracic cavity size and provides more space for ...
Which pressure within the thoracic cavity is always negative?
Intrapleural pressureIntrapleural pressure is always negative, which acts like a suction to keep the lungs inflated. The negative intrapleural pressure is due to three main factors: 1. The surface tension of the alveolar fluid.
Why is pressure more negative at the apex of the lung?
As a result of gravity, in an upright individual the pleural pressure at the base of the lung base is greater (less negative) than at its apex; when the individual lies on his back, the pleural pressure becomes greatest along his back.
Why is negative intrathoracic pressure important to breathing?
Negative intrathoracic pressure is also reflected in the perivascular space, decreasing the perivascular pressure. This increases extravascular lung water by favoring fluid transudation across pulmonary microvascular bed and by diminishing lymph outflow from the lungs.
What is negative and positive pressure in the lungs?
Rationale: Conventional positive-pressure ventilation delivers pressure to the airways; in contrast, negative pressure is delivered globally to the chest and abdomen.
Is exhalation positive or negative pressure?
Final answer: The Lungs Have Positive pressure during exhalation and Negative Pressure during inhalation.
What pressure is always negative and helps to keep the lungs inflated?
Intrapleural pressureIntrapleural pressure is the pressure within the pleural cavity. Intrapleural pressure is always negative, which acts like a suction to keep the lungs inflated.
What is negative and positive pressure?
Positive pressure is a pressure within a system that is greater than the environment that surrounds that system. Consequently, if there is any leak from the positively pressured system it will egress into the surrounding environment. This is in contrast to a negative pressure room, where air is sucked in.
What causes negative pleural pressure?
CAUSES OF NEGATIVE OF INTRAPLEURAL PRESSURE(IPP) 1-Lack of air in pleural cavity. 2-Elastic recoil of the lung which continuously pulls against the continuous tendency of relatively rigid chest wall to expand creates a continuous negative pressure. This negative pressure antagonizes the elastic recoil.
What is positive pressure in lungs?
Positive pressure ventilation describes the process of either using a mask or, more commonly, a ventilator to deliver breaths and to decrease the work of breathing in a critically ill patient.
Which pressure remains negative throughout the respiratory cycle?
The intrapleural pressure is negative, approximately -5cm H2O because the lungs and the chest wall act as opposing forces, meaning the lungs have a tendency to collapse during rest, while the chest wall has a tendency to expand.
When diaphragm contracts pressure in the thoracic cavity increases and we?
The correct answer is c): When the diaphragm contracts, it compresses the abdominal cavity. When the diaphragm contracts, the vertical dimensions of the thoracic cavity increase. The contraction of the diaphragm causes it to flatten out and thus increase the volume, and lower the pressure of the thoracic cavity.
Why is it important for the chest wall to expand?
Air (and fluids) move from areas of higher pressure to areas of lower pressure, so to drive air into the lungs, we need to make the pressure of air in the alveoli less than atmospheric pressure. This is achieved by expanding the volume of the lungs, since when a gas is expanded, its pressure drops.
What allows the thoracic cavity to increase in volume during normal inspiration?
During inspiration, the diaphragm and external intercostal muscles contract, causing the rib cage to expand and move outward, and expanding the thoracic cavity and lung volume.
What is the effect of intrathoracic pressure on the upper airway?
The negative intrathoracic pressure at the onset of inspiration generates a reflex response (increased activity) to the upper airway dilator muscles. During sleep, such reflex responses are decreased, making the upper airway susceptible to suction collapse. 179,180,240 This probably results from a decrement in the excitability of the upper airway motor neurons. In this connection, the observations of McNicholas et al. 241 of increased frequency of obstructive apneas and hypopneas in normal sleeping subjects after upper airway anesthesia and increased apnea index after upper airway anesthesia in snorers 242 support the importance of the upper airway reflexes in controlling the upper airway resistance and space. However, there is no clear indication of the impairment of upper airway reflex in OSA. Patients with OSA, in contrast to snorers and normal sleepers, do not show an increase in the apnea index after upper airway anesthesia. 243,244 Alcohol, benzodiazepines, and age 179,180,245 clearly cause a decrement in upper airway reflex response.
How does intrathoracic pressure affect cardiac output?
Intrathoracic pressure influences venous return and consequently cardiac output and arterial pressure. Inspiration drops intrathoracic pressure, dilates the thoracic vena cava, and acutely decreases atrial filling. Cardiac output falls, and consequently arterial pressure falls. The drop in arterial pressure reduces stretch on the arterial baroreceptors, causing a reflex increase in heart rate. Exhalation reverses the above steps. These cyclic changes in heart rate appear as a “normal sinus arrhythmia” on the ECG.
How does ITP affect ventricular systole?
During ventricular systole a decrease in ITP decreases the egress of blood from the thorax. In diastole the decrease in ITP reduces antegrade flow runoff, which increases thoracic arterial blood volume and increases the opposition to ejection after systole. In this manner LV ejection and SV are reduced. 179,193 This produces the decrease in systolic blood pressure in systole with spontaneous inspiration and is the mechanism of the exaggerated systolic drop in pulsus paradoxus. 178 In very negative ITP or with reduced LV function the adverse impact of respiration on LV afterload increases. If this state persists, an increase in catecholamines, SVR, and arterial blood pressure further increase LV afterload.
How does ITP affect LV afterload?
The degree to which ITP affects LV afterload is determined by the compliance of the LV and the P tm of the thoracic arterial vessels. 192 Peripheral arterial intravascular pressure is measured in relation to atmospheric pressure, but the thoracic aorta, due to its placement in the thorax, is subjected to changes in pleural pressure. Therefore the aorta P tm is the difference between aortic intravascular systolic pressure and pleural pressure. 157,192 In spontaneous respiration the ITP decreases, which increases the P tm of the thoracic arteries and therefore reduces the volume of the thoracic arterial system. The P tm is increased because the pleural pressure falls to a greater degree than the intravascular aortic pressure. The pressure of the thoracic arterial system is therefore lower relative to the extrathoracic arterial system ( Fig. 13.21 ). This produces higher LV afterload and decreases LV SV. 157,178
Why do intrathoracic pressures change during the respiratory cycle?
The changes in intrathoracic pressure during the respiratory cycle are mainly caused by the changes in the intrapleural pressure that is transmitted to all intrathoracic pressure values ( Boerrigter et al., 2014 ). It has been recommended that pressure measurements are performed at end expiration, during normal breathing, because intrathoracic pressure is closest to zero at this time point. An alternative may be a floating average of the pressure values over 3–4 respiratory cycles. This approach may enable better reproducible measurements particularly in patients with obstructive lung disease with large intrathoracic pressure changes during the respiratory cycle, and generally during exercise in all subjects ( Kovacs et al., 2014; Boerrigter et al., 2014 ).
What is the negative pressure of obstructive apnea?
Negative intrathoracic pressures as high as 60 to 80 cm H 2 O may be generated during episodes of obstructive apnea. After central apnea, hyperpnea occurs, and relatively large negative pressure deflections, particularly in the presence of stiff lungs and chest wall, may also be observed. However, pleural pressure changes are generally more pronounced in OSA than in CSA (see Figures 32-1 and 32-2 ). The increased negative pressure increases the transmural pressure (pressure inside minus pressure outside) of the intrathoracic vascular structures, including the aorta, pulmonary vascular bed, atria, and ventricles ( Figure 32-9 ).
What is the pleural space pressure?
Although the pleural space pressure is subatmospheric, gases do not accumulate there . The sum of all partial pressures of gases in capillary blood is approximately 700 mm Hg, or 60 mm Hg below atmospheric (P h2o = 47, P co2 = 46, P n2 = 570, and P o2 = 40 mm Hg). The subatmospheric pressure of dissolved gases in capillary blood helps to maintain the pleural space free of gas and facilitates absorption of any gas that does enter the pleural space. Of note, to increase the gradient favoring absorption of gas, one can lower the partial pressure of nitrogen in the blood by having a patient breathe increased concentrations of inspired oxygen. The oxygen displaces alveolar nitrogen, thereby lowering the partial pressure of nitrogen in capillary blood; because of the limited absorption of oxygen due to the plateau of the oxygen-hemoglobin dissociation curve, however, the increase in inspired oxygen does not add greatly to the partial pressure of oxygen in capillary blood.