Neuropathic arthropathy (Charcot joint) can be defined as bone and joint changes that occur secondary to loss of sensation and is most often associated with diabetes, syphilis, syringomyelia, spina bifida, traumatic spinal cord injury, and leprosy.
What is if it helps neuropathic pain?
Tricyclic antidepressants ease neuropathic pain separate to their action on depression. It is thought that they work by interfering with the way nerve impulses are transmitted. There are several tricyclic antidepressants but amitriptyline is the one most commonly used for neuralgic pain.
What is involved in peripheral neuropathy treatment?
- Acupuncture. Inserting thin needles into various points on your body might reduce peripheral neuropathy symptoms. ...
- Alpha-lipoic acid. This has been used as a treatment for peripheral neuropathy in Europe for years. ...
- Herbs. Certain herbs, such as evening primrose oil, might help reduce neuropathy pain in people with diabetes. ...
- Amino acids. ...
What is mild sensory peripheral neuropathy?
Sensorimotor polyneuropathy is a condition that causes a decreased ability to move or feel (sensation) because of nerve damage. Neuropathy means a disease of, or damage to nerves. When it occurs outside of the central nervous system (CNS), that is, the brain and spinal cord, it is called a peripheral neuropathy.
What is diabetic peripheral neuropathic pain?
What is diabetic peripheral neuropathic pain? Diabetic peripheral neuropathy is a common nerve problem in people with diabetes. It usually affects the feet and legs. It may cause a loss of feeling...
What causes neuropathic arthropathy?
The neurotraumatic theory states that Charcot arthropathy is caused by an unperceived trauma or injury to an insensate foot. The sensory neuropathy renders the patient unaware of the osseous destruction that occurs with ambulation. This microtrauma leads to progressive destruction and damage to bone and joints.
What is neuropathy arthropathy?
Neuropathic arthritis, also known as Charcot's joint or neurogenic arthropathy, is a severe form of arthritis where the cartilage between bones has been completely worn down and the joint has been severely damaged from continued friction.
What is the most common cause of neuropathic joint?
Diabetes is the foremost cause in America today for neuropathic joint disease, and the foot is the most affected region. In those with foot deformity, approximately 60% are in the tarsometatarsal joints (medial joints affected more than lateral), 30% Metatarsophalangeal joints and 10% have ankle disease.
How is Charcot arthropathy treated?
Treatment of Charcot arthropathy has been primarily nonoperative. Treatment is carried out in two phases: an acute phase and a postacute phase. Management of the acute phase includes immobilization and reduction of stress (see Medical Therapy below).
Is arthritis and arthropathy the same?
Arthropathy is a joint disease, of which arthritis is a type. Arthropathies can be associated with a hematologic (blood) disorder or an infection, such as Lyme disease.
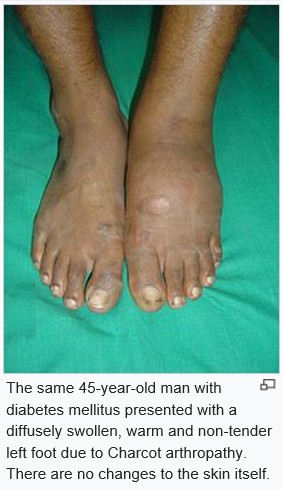
Is Charcot arthropathy painful?
Symptoms. Although patients with Charcot arthropathy typically will not have much pain, they may have other symptoms. The earliest sign of Charcot is swelling of the foot, which can occur without an obvious injury. The first thing you may realize is that you have difficulty fitting into your shoes.
What is the meaning of neuropathic?
(noor-AH-puh-thee) A nerve problem that causes pain, numbness, tingling, swelling, or muscle weakness in different parts of the body. It usually begins in the hands or feet and gets worse over time. Neuropathy may be caused by cancer or cancer treatment, such as chemotherapy.
How common is Charcot arthropathy?
How common is Charcot Foot? According to Foundation for Peripheral Neuropathy, Charcot Foot affects approximately 1 in every 2,500 Americans, totaling roughly 125,000 people. Over time, it can cause painful sores and change the shape of your foot.
What nerves Does neuropathy affect?
Overview. Peripheral neuropathy, a result of damage to the nerves located outside of the brain and spinal cord (peripheral nerves), often causes weakness, numbness and pain, usually in the hands and feet. It can also affect other areas and body functions including digestion, urination and circulation.
Does Charcot ever go away?
As many as 2.5 percent of patients with diabetes can develop Charcot foot, and it can recur in as many as five percent of cases. Fortunately, your doctor can help you in treating Charcot foot, largely reversing the damage it causes.
What is the difference between neuropathy and arthritis?
Background: Rheumatoid arthritis (RA) is an autoimmune disorder characterized by involvement of multiple small and large joints with multisystem extra-articular manifestations. Peripheral neuropathy is known extra-articular manifestation of RA with the incidence of around 39.19% as per previous studies.
What is diabetic neuropathic arthropathy?
Diabetic neuropathic arthropathy is also called diabetic osteoarthropathy. A variety of other musculoskeletal conditions have also been associated with diabetes mellitus, including specific arthropathies of the hand and shoulder, limited joint mobility, and spontaneous infarction of skeletal muscle.
What nerves Does neuropathy affect?
Overview. Peripheral neuropathy, a result of damage to the nerves located outside of the brain and spinal cord (peripheral nerves), often causes weakness, numbness and pain, usually in the hands and feet. It can also affect other areas and body functions including digestion, urination and circulation.
Can neuropathy cause joint pain?
Peripheral Neuropathy This is the most common form of diabetic joint and nerve pain. It can affect your legs, arms, hands, feet, fingers, and toes. With ongoing diabetes, joints can no longer respond like they should to the strain and stress placed on them.
What is neuropathic arthropathy?
Neuropathic arthropathy is a relatively painless, progressive, destructive arthropathy caused by a neurologic deficit. The first description was probably by William Musgrave (1655-1721), a physician from the West of England, but it was the French neurologist Jean-Martin Charcot (1825-1893)1 who gave his name to the condition. In 1868 he described “l'arthropathie des ataxiques” in a French soldier with tertiary syphilis who had been marching 25 km each day. He thought that the “bag of bones” represented spontaneous fractures as a result of nerve degeneration and bone atrophy. Sir James Paget named the condition after Charcot in 1881, but in this chapter the term neuropathic arthropathy is used throughout. In 1917 Eloesser assessed the role of trauma in the development of neuropathic arthropathy by cutting the posterior roots of the spinal cord in cats, which resulted in analgesia, anesthesia, and ataxia. His work was used to support the neurotraumatic theory of pathogenesis. In 1936 Jordan 2 gave the initial description of neuropathic arthropathy associated with diabetes. Diabetes is now the most common cause of neuropathic arthropathy, accounting for two thirds of all cases in the lower limb. 3 Leprosy 4 is a common cause in endemic areas of the disease.
What is a neuropathic foot?
Neuropathic arthropathy is a relatively painless, progressive, and degenerative arthropathy of single or multiple joints caused by the underlying neurologic deficits. The most frequent sites of involvement include the tarsometatarsal joints (60%), metatarsophalangeal joints (61%), and ankle joint (9%). On examination, the foot is grossly deformed with a typical rocker bottom subluxation of the midtarsal region or subluxations of the metatarsophalangeal joints and a high arch with cocked-up toes. The foot is erythematous, warm to the touch, and anhidrotic. The exact mechanism is unknown; however, it is hypothesized that hyperemia from autonomic neuropathy results in ligament laxity and osteolysis. With continued microtrauma due to sensory neuropathy, the bone and joint surfaces are destroyed. Loss of normal protective mechanisms subjects joints to extreme ranges of motion, resulting in capsular and ligamentous stretching, joint laxity with eventual dislocation, fracture, and bone and joint destruction. This process occurs in the presence of bounding pulses and elevated ABIs. The hyperemia or increased blood supply promotes resorption of the normal bone, creating a vicious cycle.
What is Charcot's disease?
In 1868, Jean-Martin Charcot first described the neuropathic joint changes associated with tabes dorsalis, believing them to be a secondary effect of the neurologic deficit related to tertiary syphilis. In 1936, Jordan first described neuropathic arthropathy in diabetics, and in 1947 the Joslin Clinic published the first series of cases. Today diabetes is the most common cause of Charcot joints, which occur in 1:680 diabetic feet. Charcot neuroarthropathy of the foot is one of the most devastating consequences of diabetes, occurring in patients with an average duration of diabetes of 12 to 18 years; 18% of cases are bilateral. The radiographic findings are characterized by a severely destructive form of degenerative arthritis with simultaneous bone destruction, joint destruction, subluxation or dislocation, and fragmentation in addition to hypertrophic periosteal reaction.
What is the difference between osteomyelitis and neuropathic arthropathy?
The distinction between neuropathic joint arthropathy and osteomyelitis is based on distribution of disease, the association with an ulcer, and the MRI signal characteristics of the bone marrow. Neuropathic arthropathy usually affects the Lisfranc, metatarsophalangeal, and subtalar joints. Osteomy elitis can affect any bone, but it is usually associated with contiguous spread from an ulcer and abnormal adjacent soft tissues. STIR sequences are very sensitive to edema in bones, whether the edema is due to osteomyelitis or to neuropathic/osteoarthritic changes. Because bone edema is not specific for bone infection, STIR images may lead to false-positive diagnoses of osteomyelitis, and the finding of bone edema must be interpreted in light of other MRI findings. Postgadolinium images are also helpful in evaluating edema versus cellulitis.
What is a combination of sensory, motor, and autonomic dysfunction?
Neuropathic arthropathy results from a combination of sensory, motor, and autonomic dysfunction.
What is the discriminator for neuropathic arthropathy?
One possible discriminator is called “ghost sign”; bones that appear vanished on T1-weighted images but are better delineated on T2-weighted and contrast-enhanced imaging and show a diffusely abnormal marrow signal are likely to contain osteomyelitis despite underlying neuropathic arthropathy. 6
What is Charcot joint?
That neuropathic arthropathy (Charcot joints) may be associated with loss of pain sensation has been known for a long time. This complication is encountered in tabes dorsalis, diabetic neuropathy, syringomyelia, and various sensory neuropathies. The affected joint may demonstrate fractures and bone fragmentation, subluxation, dislocation, effusion, and bone resorption. We have chosen to use the name “neuropathic arthropathy” or “neurogenic arthropathy” rather than “neurotropic arthropathy” because we assume that the joint dissolution is due, in some nerves, to insensitivity (a neuropathy) and use and abuse, rather than to lack of a tropic influence.
What is neuropathic arthropathy?
neuropathic arthropathy chronic progressive degeneration of the stress-bearing portion of a joint, with hypertrophic changes at the periphery; it is associated with neurologic disorders involving loss of sensation in the joint. Called also Charcot's arthropathy.
What type of arthropathy is progressive with multiple joint involvement in the upper extremity?
Neuropathic arthropathy progressing with multiple joint involvement in the upper extremity due to syringomyelia and type I Arnold-Chiari malformation.
What is joint disease?
Joint disease caused by diminished proprioceptive sensation, with gradual destruction of the joint by repeated subliminal injury, commonly associated with tabes dorsalis or diabetic neuropathy.
What is chondrocalcific arthropathy?
chondrocalcific arthropathy progressive polyarthritis with joint swelling and bony enlargement, most commonly in the small joints of the hand but also affecting other joints, characterized radiographically by narrowing of the joint space with subchondral erosions and sclerosis and frequently chondrocalcinosis.
What is the term for clubbing of the fingers and toes?
osteopulmonary arthropathy clubbing of fingers and toes, and enlargement of ends of the long bones, in cardiac or pulmonary disease.
Is glenohumeral joint neuropathic?
Neuropathic arthropathy of the glenohumeral joint is very rare , with sparse evidence available to help guide treatment.
What conditions cause neuropathy?
Diabetes mellitus- foot and ankle are most affected. Tertiary syphilis (tabes dorsalis) - the knee is the most affected joint. Syringomyelia – shoulder is the most affected joint. Trauma.
What is Charcot arthropathy?
Sometimes, the resulting joint deformity increases the risk of amputation. Charcot arthropathy is a specific manifestation of peripheral neuropathy, also known as Neuropathic Joint Disease. It is named after Jean-Martin Charcot, who recognized that peripher al neuropathy could lead to neuropathic joints. Any condition resulting in decreased ...
What is a complication of peripheral neuropathy that results in fractures, dislocations, subluxations?
Neuropathic arthropathy (Charcot arthropathy) is a complication of peripheral neuropathy that results in fractures, dislocations, subluxations. It has an increased risk of progressive deformity of the affected joint. Sometimes, the resulting joint deformity increases the risk of amputation.
What is Charcot arthropathy?
Charcot arthropathy, also known as Charcot neuroarthropathy or Charcot foot and ankle, is a syndrome in patients who have peripheral neuropathy, or loss of sensation, in the foot and ankle. Patients may experience fractures and dislocations of bones and joints with minimal or no known trauma.
How long does it take to diagnose Charcot arthropathy?
Diagnosis. The time between the start of symptoms and a diagnosis may be several weeks or months. Often Charcot arthropathy is misdiagnosed initially because symptoms can mimic those of an injury or infection. Diagnosis is based on a high likelihood for this problem in patients with neuropathy.
Why is it common for there to be a delay between onset of signs and diagnosis of Charcot foot?
Why is it common for there to be a delay between onset of signs and diagnosis of Charcot foot?#N#The initial signs of Charcot foot are non-specific and typically are seen in other more common conditions such as infections and rheumatologic conditions. Many patients do not have pain or have pain from neuropathy that was pre-existing. Physicians who are not specialists in orthopaedic foot and ankle problems may see a Charcot foot very few times in an entire career, less frequently than other conditions such as septic arthritis, gout, rheumatoid arthritis and other inflammatory arthropathies.
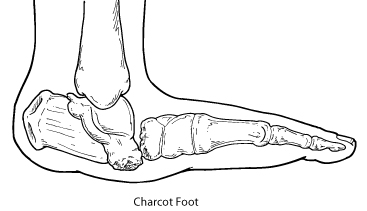
What is the name of the fracture in the foot?
Later, when fractures and dislocations occur, there may be severe deformities of the foot and ankle, including collapse of the midfoot arch (often called rocker bottom foot) or instability of the ankle and hindfoot. The syndrome progresses through three general stages:
What are the deformities of the midfoot?
Deformities may occur in any part of the foot and ankle and result in ulcers from bony pressure against the shoe or ground; ulcers may become infected, and infections may be limb- and life-threatening. Some Charcot joints, such as the ankle, may heal with fibrous tissue (non-union) and this may result in gross instability (“floppy foot”) that may predispose to ulcers and may be difficult to support with braces.
Can microtrauma cause fractures?
Repetitive microtrauma that exceeds the rate of healing may cause fractures and dislocations. Changes in circulation may cause resorption of bone, weakening of the bone, and increasing susceptibility to fracture and dislocation. Charcot arthropathy may affect any part of the foot and ankle. Multiple regions may be involved.
What is neurogenic arthropathy?
Neurogenic arthropathy is a rapidly destructive arthropathy due to impaired pain perception and position sense, which can result from various underlying disorders, most commonly diabetes and stroke. Common manifestations include joint swelling, effusion, deformity, and instability. Pain may be disproportionately mild due to ...
When should neurogenic arthropathy be diagnosed?
The diagnosis of neurogenic arthropathy should be considered in a patient with a predispos ing neurologic disorder who develops a destructive but unexpectedly painless arthropathy, usually several years after the onset of the underlying neurologic condition. If neurogenic arthropathy is suspected, x-rays should be taken.
How long does it take for arthropathy to develop?
Arthropathy does not usually develop until years after onset of the neurologic condition but can then progress rapidly and lead to complete joint disorganization in a few months. Pain is a common early symptom. However, because the ability to sense pain is commonly impaired, the degree of pain is often unexpectedly mild for the degree of joint damage. A prominent, often hemorrhagic, effusion and subluxation and instability of the joint are usually present during early stages. Acute joint dislocation sometimes occurs also.
How does proprioception affect the joint?
Impaired deep pain sensation or proprioception affects the joint’s normal protective reflexes, often allowing trauma (especially repeated minor episodes) and small periarticular fractures to go unrecognized. Increased blood flow to bone from reflex vasodilation, resulting in active bone resorption, contributes to bone and joint damage.
Why is pain so mild?
However, because the ability to sense pain is commonly impaired, the degree of pain is often unexpectedly mild for the degree of joint damage. A prominent, often hemorrhagic, effusion and subluxation and instability of the joint are usually present during early stages. Acute joint dislocation sometimes occurs also.
What causes bone and joint damage?
Increased blood flow to bone from reflex vasodilation, resulting in active bone resorption, contributes to bone and joint damage. Each new injury sustained by the joint causes more distortion as it heals. Hemorrhagic joint effusions and multiple small fractures can occur, accelerating disease progression.
Where are osteophytes found in the spine?
Rarely, calcification and ossification occur in the soft tissues. Large, bizarrely shaped osteophytes may be present at the joint margins or within joints. Large curved (parrot’s beak) osteophytes frequently develop in the spine in the absence of clinical spinal disease.
What is neuropathy in the nervous system?
Neuropathy is a disturbance of function or a change in one or several nerves. Diabetes is responsible for about 30% of neuropathy cases.
What causes neuropathic pain?
Neuropathic Pain. About 30% of all nerve pain (neuropathic pain) happens because of diabetes, but other diseases like alcoholism and shingles can cause neuropathic pain. Treatment might include medicines, physical therapy, psychological counseling, and even surgery. Appointments & Access. Contact Us.
What is the nerve that causes pain in the body?
You can feel pain from any of the various levels of the nervous system—the peripheral nerves , the spinal cord and the brain. Together, the spinal cord and the brain are known as the central nervous system. Peripheral nerves are the ones that are spread throughout the rest of your body to places likes organs, arms, legs, fingers and toes.
How to diagnose neuropathy?
Your healthcare provider will take a medical history and do a physical exam. If your provider knows or suspects you have nerve injury, they will recognize typical neuropathic pain symptoms. Your provider will then try to find the underlying cause of the neuropathy and trace the symptoms.
Can opioids be used for neuropathic pain?
Opioid analgesics are less effective in treating neuropathic pain, and negative effects may prevent their long-term use. The pain can also be treated with nerve blocks given by pain specialists, including injections of steroids, local anesthetics, or other medicines into the affected nerves.
Is neuropathic pain life threatening?
Neuropathic pain is difficult to treat completely but is usually not life-threatening. You’ll get the best results from combining rehabilitation with support for your emotional, social and mental wellbeing.
What is neuropathic pain?
Neuropathic pain is a pain condition that’s usually chronic. It’s usually caused by chronic, progressive nerve disease, and it can also occur as the result of injury or infection. If you have chronic neuropathic pain, it can flare up at any time without an obvious pain-inducing event or factor. Acute neuropathic pain, while uncommon, can occur as ...
How does neuropathic pain affect your life?
Neuropathic pain can negatively impact your life if you don’t take steps to treat it and prevent worsening symptoms. Over time, this can lead to serious disability and complications, including depression, problems sleeping, anxiety, and more.
How many people have neuropathic pain?
Neuropathic pain tends to get worse over time. About 1 in 3 Americans experience chronic pain. Of those, 1 in 5 experience neuropathic pain. A 2014 study estimated that as many as 10 percent of Americans experience some form of neuropathic pain.
Why aren't neuropathic pain pills effective?
However, many people find these medicines aren’t effective for neuropathic pain because they don’t target the source of the pain.
Can a back injury cause nerve damage?
Likewise, back, leg, and hip problems or injuries can cause lasting damage to nerves. While the injury may heal, the damage to the nervous system may not. As a result, you may experience persistent pain for many years after the accident. Accidents or injuries that affect the spine can cause neuropathic pain, too.
Can a physical therapist help with neuropathic pain?
For example, some people with neuropathic pain may experience increased symptoms after sitting for several hours. This might make desk jobs difficult to perform. A physical therapist or occupational therapist can teach you techniques for sitting, stretching, standing, and moving to prevent pain.
Can neuropathic pain be a sign of illness?
Acute neuropathic pain, while uncommon, can occur as well. Typically, non-neuropathic pain ( nociceptive pain) is due to an injury or illness. For example, if you drop a heavy book on your foot, your nervous system sends signals of pain immediately after the book hits.
What is arthropathy?
Arthropathy is a joint disease, of which arthritis is a type. Arthropathies can be associated with a hematologic (blood) disorder or an infection, such as Lyme disease.
Diagnosis
Diagnosis requires careful clinical evaluation to determine the cause of the symptoms.
Treatment
Medicines and physical therapy can help maintain motion and ease pain and swelling.
Clinical significance
Symptoms
- Neuropathic arthropathy in the diabetic foot is often difficult to differentiate from osteomyelitis. Neuropathic arthropathy, a progressive, degenerative process of the foot and ankle, presents with similar symptoms to osteomyelitis including erythema, tenderness, and edema. MRI may show similar subchondral bone marrow signal abnormalities, and soft tissue changes with periosteal r…
Diagnosis
- Nuclear scintigraphy is a frequently used tool in the diagnosis of infection versus diabetic neuropathy. Indium-labeled leukocyte scans demonstrate areas of infection; however, they are not reliable alone because the uninfected neuropathic joint also demonstrates uptake of labeled leukocytes. Inflammation, bone remodeling, and hematopoietically active marrow explain why w…
Research
- Positron emission tomography (PET) has more recently been studied as an accurate method in the evaluation of infection in patients with diabetic neuroarthropathy and superimposed osteomyelitis. One study demonstrated that PET imaging using 18F-FDG is able to localize the precise anatomic site of increased uptake and accurately identify osteomyelitis of the diabetic f…
Definition
- A Charcot arthropathy, or neuropathic arthropathy, is a process of chronic, noninfective, painless joint destruction. Charcot first described this condition associated with tabes dorsalis in 1868. Approximately 0.1% to 0.5% of diabetic patients will develop a neuroarthropathic joint. Two theories explain the development of a Charcot joint. The neur...
Signs and symptoms
- The presenting symptoms of a Charcot foot include the spontaneous onset of a warm, swollen foot that is associated with no pain or vague pain. The midfoot is most commonly involved, followed by the hindfoot and ankle. The midfoot will lose its arch over time, and the forefoot will dorsiflex and abduct, producing a rocker-bottom foot deformity. The patient is then predisposed …
Epidemiology
- Eleven percent of the cases reported by Newman23 had spontaneous fractures and dislocations. These cases presented the greatest therapeutic problems compared with other noninfective diseases of bone. Newman stressed the importance of recognizing these conditions and distinguishing them from osteomyelitis. Holmes93 reported on a series of diabetic patients wh…
Prognosis
- Autonomic neuropathy with loss of vasomotor control and increased peripheral blood flow to bone, coupled with an inflammatory hyperemia of the soft tissues, results in resorption of bone with further weakening. Atrophic bone is easily fractured or fragmented. Frequent spontaneous fractures in neuropathic patients have led some authors45,51,71,76,86 to believe that intrinsic b…
Symptoms
- Initially, there may be swelling, redness and increased warmth of the foot and ankle. Later, when fractures and dislocations occur, there may be severe deformities of the foot and ankle, including collapse of the midfoot arch (often called rocker bottom foot) or instability of the ankle and hindfoot. The syndrome progresses through three general stages: 1. Stage 1 (acute, developme…
Causes
- Charcot foot occurs in patients with peripheral neuropathy resulting from diverse conditions including diabetes mellitus, leprosy, syphilis, poliomyelitis, chronic alcoholism, or syringomyelia. Repetitive microtrauma that exceeds the rate of healing may cause fractures and dislocations. Changes in circulation may cause resorption of bone, weakening the bone and increasing susce…
Diagnosis
- The time between the start of symptoms and a diagnosis may be several weeks or months. Often Charcot arthropathy is misdiagnosed initially because symptoms can mimic those of an injury or infection. Diagnosis is based on a high likelihood for this problem in patients with neuropathy. Increased redness, swelling, and warmth may be the only early sig...
Treatments
- Non-surgical:Non-surgical treatment includes a protective splint, walking brace, orthosis or cast. Early weightbearing is allowed in stage one by 41 percent of specialists and in stage two by 49 percent of specialists, and other specialists recommend non-weightbearing. After stable healing is noted in stage three, treatment includes accommodative footwear with protective orthoses. S…
Recovery
- Healing may take several months. Healing times after surgery may be twice the usual duration than for a non-diabetic foot. With Charcot foot and ankle, healing after fusion may require six months of protection and orthoses. Charcot foot and ankle may recur or flare up. Also, it is common for both feet to be affected, which can make impairment permanent. Patients use prot…
Risks and Complications
- Severe deformities may include collapse of the midfoot arch (called rocker bottom foot) with associated plantar midfoot ulcer. Deformities may occur in any part of the foot and ankle and result in ulcers from bony pressure against the shoe or ground; ulcers may become infected, and infections may be limb- and life-threatening. Some Charcot joints, such as the ankle, may heal wi…
FAQs
- Why is it common for there to be a delay between onset of signs and diagnosis of Charcot foot? The initial signs of Charcot foot are non-specific and typically are seen in other more common conditions such as infections and rheumatologic conditions. Many patients do not have pain or have pain from neuropathy that was pre-existing. Physicians who are not specialists in orthopae…