Explore
Using a booted (or padded) clamp, begin at the dressing and clamp the drainage tubing momentarily. Look at the water-seal/air leak meter chamber. Keep moving the clamp down the drainage tubing toward the chest drainage system, placing it at 20 to 30 cm intervals. Each time you clamp, check the water-seal/air leak meter chamber.
How to measure chest tube drainage?
The mean duration of CT insertion was 45.2 hours (SD 26.7), and total drainage volume was 1300.6 mL (SD 763.8). Drainage volumes plateau to 31 mL per hour, 8 hours after surgery. From 24 to 48 hours, the mean drainage was 21 mL per hour. Drainage volumes varied between genders.
How much drainage is normal after open heart surgery?
• If air leak is in the chest drainage system, replace the system 2. System Air Leak • Continue the clamping process down the tubing at 8–12 in. (20–30 cm) intervals until you find the origin of the leak • Tighten all connections • Tape connection between patient drainage tube and thoracic catheter For proper connection between patient drainage
How to troubleshoot air leaks in chest tube systems?
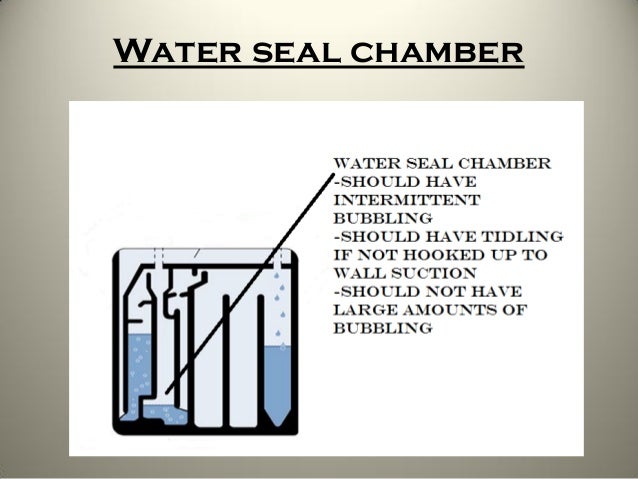
- Check the water-seal level every shift and maintain the proper level to ensure that the system is being used properly and to maintain the patient’s safety.
- Check for fluctuation in the water-seal chamber as the patient breathes. ...
- Check for intermittent bubbling in the water-seal chamber. ...
How to drain chest tube?
What is normal chest tube drainage per hour?
Pediatric: 3 mL/Kg/hour in a 3 hour period or 5 to 10 mL/Kg in any 1 hour period. NURSING ALERT: Adult patients with a chest tube who are stable may be transported without being accompanied by a nurse. Nurse must assess that patient is being transported safely.
How many mL of drainage is a normal chest tube?
Acceptable air flows for chest tube removal are below 20 mL/min for 8–12 hours when no suction is applied, or less than 40 mL/min for 6 hours in accordance with other authors5,31.
What is too much drainage from chest tube?
Drainage that is red and free-flowing indicates a hemorrhage. A large amount of drainage, or drainage that changes in colour, should be recorded and reported to the primary health care provider. Drainage that suddenly decreases may indicate a blood clot or obstruction in the chest tube drainage system.
How is chest tube drainage measured?
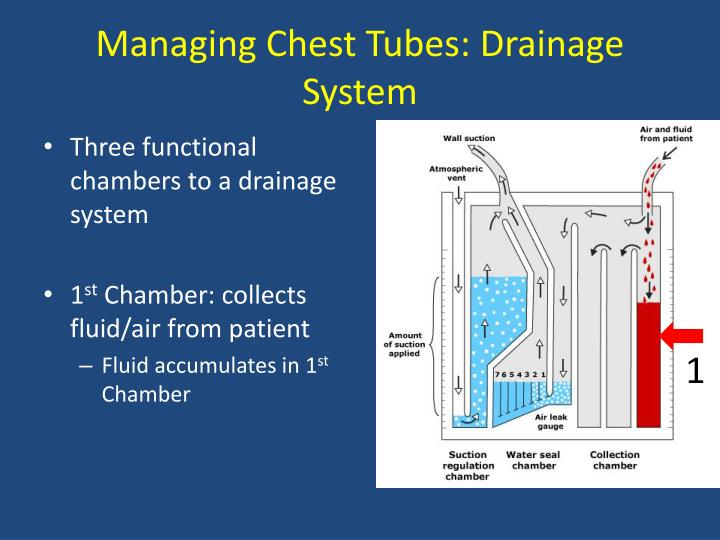
Collection chamber: The chest tube connects directly to the collection chamber, which collects drainage from the pleural cavity. The chamber is calibrated to measure the drainage. The outer surface of the chamber has a “write-on” surface to document the date, time, and amount of fluid.
How much pleural fluid is drained?
Pleural fluid drainage should to be started immediately and up to 1500 mL of fluid can be removed. After removing the pleural fluid, a chest radiograph or postprocedural CT scan should be obtained to confirm the appropriate position of the pigtail catheter and evaluate possible complications including pneumothorax.
What should chest tube suction be set at?
The chest tube should initially be set to continuous suction at -20 mmHg to evacuate the air. Once the air leak has stopped, the chest tube should be placed on water seal to confirm resolution of the pneumothorax (water seal mimics normal physiology).
How can you tell if a chest tube has an air leak?
Determination of the Presence of an Air Leak To quantify the amount of air leak in a patient connected to a chest tube, the patient is asked to cough, and the water column and the water seal column in the chest tube drainage system are observed. If there are no air bubbles, the pleural cavity is devoid of air.
What is the nurse's priority assessment when caring for a patient with a chest tube?
What are the nursing responsibilities when caring for a client with a chest tube to a drainage system? Look at the client first- (color, level of consciousness, airway patency, respiratory rate, depth, rhythm, chest movement- symmetry, lung sounds, lips/ nailbeds).
What does bubbling in chest tube mean?
Air LeakAir Leak (bubbling) Continuous bubbling of this chamber indicates large air leak between the drain and the patient. Check drain for disconnection, dislodgement and loose connection, and assess patient condition. Notify medical staff immediately if problem cannot be remedied.
What size pleural effusion should be drained?
The recommended limit is 1000-1500 mL in a single thoracentesis procedure. Preventive strategies include monitoring pleural pressure with a manometer. Larger amounts of pleural fluid can be removed if pleural pressure is monitored by pleural manometry and is maintained above -20 cm water.
What color should fluid drained from lungs be?
Normally, this area contains about 20 milliliters of clear or yellow fluid. If there's excess fluid in this area, it can cause symptoms such as shortness of breath and coughing. An excess of pleural fluid, known as pleural effusion, will show up on a chest X-ray, CT scan, or ultrasound.
How much water should be in the water seal chamber?
2 cm.LEVEL OF WATER IN WATER SEAL CHAMBER The water level should be at 2 cm. Water may need to be added due to evaporation. Add as needed through short suction tube. Water may need to be withdrawn if chamber is overfilled.
How much drainage is normal after open heart surgery?
Drainage volumes plateau to 31 mL per hour, 8 hours after surgery.
How much water should be in the suction control chamber?
Water seal should be maintained at 2cm line and suction control chamber should bubble gently when connected to suction. Adjust stopcock or suction source as needed to increase or decrease suction control bubbling. patient when kept in an upright position.
What color should fluid drained from lungs be?
Normally, this area contains about 20 milliliters of clear or yellow fluid. If there's excess fluid in this area, it can cause symptoms such as shortness of breath and coughing. An excess of pleural fluid, known as pleural effusion, will show up on a chest X-ray, CT scan, or ultrasound.
How can you tell if a chest tube has an air leak?
Determination of the Presence of an Air Leak To quantify the amount of air leak in a patient connected to a chest tube, the patient is asked to cough, and the water column and the water seal column in the chest tube drainage system are observed. If there are no air bubbles, the pleural cavity is devoid of air.
Why should tubing be secured to patient bed?
Tubing should be anchored to the patient’s skin to prevent pulling of the drain. In PICU and NICU tubing should also be secured to patient bed to prevent accidental removal. Ensure the unit is securely positioned on its stand or hanging on the bed. Ensure the water seal is maintained at 2cm at all times.
What is the valve effect of pneumothorax?
Tension Pneumothorax: One way valve effect which allows air to enter the pleural space , but not leave. Air builds up and forces a mediastinal shift. This leads to decreased venous return to the heart and lung collapse/compression causing acute life-threatening respiratory and cardiovascular compromise. Ventilated patients are particularly high risk due to the positive pressure forcing more air into the pleural space . Tension pneumothorax can result in rapid clinical deterioration and is an emergency situation
Why do we need an underwater seal?
The underwater seal also prevents backflow of air or fluid into the pleural cavity. Appropriate chest drain management is required to maintain respiratory function and haemodynamic stability.
Where is chest drain recorded?
Ensure that Chest Drain is recorded in the EMR under the LDA flowsheet
Why can't clamps be used on patients?
Clamps must not be used on the patient for transport because of the risk of tension pneumothorax
What is an under water seal drain?
Under Water Seal Drain (UWSD): Drainage system of 3 chambers consisting of a water seal, suction control and drainage collection chamber. UWSD are designed to allow air or fluid to be removed from the pleural cavity, while also preventing backflow of air or fluid into the pleural space
How to collect fluid from a tubing?
Procedure: Wait for the fluid to collect in a loop of the tubing. Perform hand hygiene, then don gloves & eye protection. Clean the sampling port, or for smaller sampling volumes you can use the patient tube, with an alcohol wipe and leave to dry for 20 seconds. Clamp the tubing above where the fluid has collecte.
What is the best chest tube size for pleural disease?
However, the Therapeutic Interventions in Malignant Effusion (TIME1) randomized controlled trial found that 12F chest tubes were associated with a higher pleurodesis failure than 24F chest tubes (30% vs. 24%) in 100 patients with malignant effusions, suggesting that chest tube size matters for pleurodesis efficacy12. Moreover, even though the smaller chest tubes resulted in significantly less pain than the larger ones, the difference was not likely clinically significant (mean visual analog scale of 22 vs. 26.8)12. Based upon expert opinion, use of chest tubes ≥20F is recommended in the following situations2,3,5,13: (1) there is clinical concern for the presence of an on-going air leak (or significant risk of it, as in traumatic pneumothorax or bronchial dehiscence), (2) iatrogenic pneumothorax from barotrauma (mechanical ventilation), (3) hemothoraces, and (4) postoperative drainage of the chest cavity.
How big is a 12f chest tube?
Thus, a 12F tube is 4 mm in diameter. Chest tube sizes usually range between 8F and 36F (Figure 1).
How is SBCT placed?
SBCT are commonly placed using the catheter-over-guide wire (Seldinger) technique, in which a guide wire is inserted into the pleural space through an introducer needle; the wire should pass without resistance. Then, the needle is removed and dilators are threaded over the wire using a slight twisting action. Afterwards, the chest tube is threaded over the guide wire and into the pleural space, where remains14,17. In cases of pneumothorax, SBCT are directed toward the apex, but for pleural effusions they are directed both inferiorly and posteriorly into the diaphragmatic recess. A silk or synthetic monofilament suture (number 1) along with an adhesive dressing secure the tube in position. An attached 3-way stopcock connects the tube with the drainage system. A chest radiography to confirm the chest tube position is mandatory.
What is a chest tube?
Chest tube insertion is a common procedure usually done for the purpose of draining accumulated air or fluid in the pleural cavity. Small-bore chest tubes (≤14F) are generally recommended as the first-line therapy for spontaneous pneumothorax in non-ventilated patients and pleural effusions in general, with the possible exception of hemothoraces and malignant effusions (for which an immediate pleurodesis is planned). Large-bore chest drains may be useful for very large air leaks, as well as post-ineffective trial with small-bore drains. Chest tube insertion should be guided by imaging, either bedside ultrasonography or, less commonly, computed tomography. The so-called trocar technique must be avoided. Instead, blunt dissection (for tubes >24F) or the Seldinger technique should be used. All chest tubes are connected to a drainage system device: flutter valve, underwater seal, electronic systems or, for indwelling pleural catheters (IPC), vacuum bottles. The classic, three-bottle drainage system requires either (external) wall suction or gravity (“water seal”) drainage (the former not being routinely recommended unless the latter is not effective). The optimal timing for tube removal is still a matter of controversy; however, the use of digital drainage systems facilitates informed and prudent decision-making in that area. A drain-clamping test before tube withdrawal is generally not advocated. Pain, drain blockage and accidental dislodgment are common complications of small-bore drains; the most dreaded complications include organ injury, hemothorax, infections, and re-expansion pulmonary edema. IPC represent a first-line palliative therapy of malignant pleural effusions in many centers. The optimal frequency of drainage, for IPC, has not been formally agreed upon or otherwise officially established.
What is the purpose of a chest tube placement?
Chest tube placement (also called tube thoracostomy) is a common procedure in daily clinical practice which is performed to drain fluid, blood, or air from the pleural cavity. It also serves as a route to instill antibiotics (post-pneumonectomy empyemas), sclerosing agents (pleurodesis), as well as fibrinolytics, DNAse, and/or saline (complicated parapneumonic effusions and empyemas). On the other hand, indwelling pleural catheters (IPC) are becoming a first-line palliative therapy for symptomatic malignant and persistent benign pleural effusions.
Why does my chest tube keep bubbling?
Intermittent or constant bubbling within the water-seal chamber is indicative of an air leak, which is often more apparent when the patient coughs. Causes of bubbling other than a visceral pleural tear include a migrated tube with drainage holes outside the skin, or an inadequate closure of the chest tube insertion site. Moreover, patency of the chest tube is verified by observing respiratory fluctuations of the fluid in the water-seal chamber when the patient is on gravity drainage; no fluctuation indicates that either the tube is occluded or the lung is completely expanded and has blocked the holes of the chest tube inside the chest cavity. Swinging of the fluid in the collecting tube during respiratory cycles (“tiding”) is also characteristic of a correctly placed chest tube.
What are the indications for an intercostal chest drain?
The most common include pneumothoraces, complicated parapneumonic effusions or empyemas, hemothoraces, bedside pleurodesis, and following cardio-thoracic surgery or thoracoscopic procedures to allow for appropriate lung re-expansion2. Moreover, IPC provide symptomatic relief in patients with large malignant effusions, benign effusions resistant to medical therapies, effusions which failed following an attempted pleurodesis, and effusions associated with unexpandable lungs2.
What is a chest tube?
A chest tube, also known as a thoracostomy tube, is a flexible tube that can be inserted through the chest wall and into the pleural space. This activity reviews the indications, contraindications, and technique involved in placing a chest tube and highlights the role of the interprofessional team in the care of patients undergoing this procedure.
What is the best way to manage a chest tube?
Depending on the indication for the placement of the thoracostomy tube, the overall concept of how to manage one is based on the favorable opposition of the visceral and parietal pleura. The three options of how to manage a chest tube are suction, water seal, and clamping.
What is a small thoracostomy tube?
Small thoracostomy tubes (such as Wayne catheters) are meant to treat pneumothorax over hemothorax or effusion secondary to the risk of clogging. Larger chest tubes, usually 28 French or larger, are needed for drainage of blood or pus in adults.
How to stop a pneumothorax after discontinuation?
Discontinuation: Upon removal, try to avoid discontinuing the tube upon inspiration because this develops a pressure gradient inside the chest that can have air track intrathoracic and cause a persistent/recurrent pneumothorax after discontinuation. There are several tricks to prevent this from occurring. One is to time the discontinuation and synchronizes with the patient's breathing. Another trick is to have the patient hold their breath or make a seal and blow on their thumb like blowing up a balloon. An occlusive dressing with vaseline or xeroform gauze is preferred or placing a U-stitch around the incision site and tightening when the tube is discontinued is another option. [4][5]
What is a thoracostomy tube made of?
Thoracostomy tubes are commonly made from PVC or silicone. They range in from 6 French to 40 French. The majority are fenestrated along the sides of the insertion end, and the tubes have a radiopaque stripe. After placement, the distal end of the tube is connected to a pleura-evac system. There are three chambers of a pleura-evac: suction chamber, water seal chamber, and the collection chamber. The water seal chamber acts as a one-way valve allowing air to escape from gravity, but not to re-enter the thoracic cavity. [1][2][3]
How many cc is a thoracotomy tube?
If the thoracostomy tube is placed for traumatic hemothorax, the indications for a thoracotomy include an initial sanguineous output of 1500 cc or an average of 200 cc/hr over 4 hours consecutive hours.
What are the factors that make a patient high risk for persistent air leak?
Factors that make a patient high-risk for persistent air leak include steroid use, emphysematous lungs, re-operation with extensive scar tissue, or significant trauma to the lungs.
How much chest tube drainage is normal?
When compared to a daily amount of drainage of 150 ml, removing the chest tube at 200 ml/day is safe and may even result in a shorter hospital stay. Chest tubes are usually removed when they are empty or if there is evidence that the patient's lung is healing.
How long should a chest tube stay in?
Your doctor will discuss with you how long the drain should be in place. Depending on how well you respond to therapy, this might range from one day to one to two weeks. Several chest X-rays may be required during this period to determine how much fluid or air remains.
What is another name for a chest tube?
A chest tube (also known as a thoracic catheter, thoracostomy tube, or intercostal drain) is a flexible plastic tube that is introduced through the chest wall and into the pleural space or mediastinum. The purpose of this procedure is to remove air and other material that have accumulated in the pleural cavity or pericardial sac.
What to do if chest tube becomes dislodged?
What to do if chest tube becomes dislodged? Cover the site with a sterile dressing, and tape on three sides (this allows air to escape and prevent tension pneumothorax) and notify physician immediately.
Why do we need mediastinal tubes?
Mediastinal chest tubes are usually placed after cardiac surgery to help drain blood from the pericardial space (placed under the sternum) which prevents fluid from compressing the heart which can lead to cardiac tamponade. Pleural space: a small space that surrounds the lungs that contains a small amount of serous fluid.
Why does my pleural space bubble?
There may be intermittent bubbling, which is expected as air is drained from the pleural space, especially for treatment of a pneumothorax. Remember that a pneumothorax is an AIR leak between the lung and chest wall….therefore air can escape into the water seal chamber causing intermittent bubbles.
What is the space that surrounds the lungs?
Pleural space : a small space that surrounds the lungs that contains a small amount of serous fluid. This small space is surrounded by the parietal and visceral pleurae. These two layers glide over each other which creates a negative pressure. Therefore, if air or extra fluid enters into the pleural space the lungs are severely affected and can collapse.
What are the different types of pleural effusions?
Types of Pleural Effusions : Hemothorax: blood enters in the pleural space and causes lung to collapse (trauma to the chest, disease TB, blood clotting issue) Empyema (infection in the pleural space) Chylothorax (lymphatic fluid in pleural space),
What is the purpose of chest x-rays after lung removal?
Note: the patient will have chest x-ray (ordered by the physician) to assess lung expansion after removal.
How to keep tubing from kinking?
Tubing: Keep it free from kinks and make sure it is draining freely (not clots or stagnate fluid) and that all connections are sealed
