| Pulmonary function test | Normal value (95 percent confidence interval) |
|---|---|
| FVC | 80% to 120% |
| Absolute FEV1 /FVC ratio | Within 5% of the predicted ratio |
| TLC | 80% to 120% |
| FRC | 75% to 120% |
What is the normal range for vital capacity?
Vital capacity (VC), the volume of exhaled air after maximal inspiration, normally is 60 to 70 mL/kg and in normal persons is determined primarily by the size of the thorax and lungs. Reduction of VC to 30 mL/kg is associated with weak cough, accumulation of oropharyngeal secretions, atelectasis, and hypoxemia.
What is normal vital capacity for a female?
Vital capacity is the maximum amount of air that can be exhaled after a maximum inhalation. It can be dependent on age, sex, height etc and it falls as it grows. male: vital capacity(ml)=(27.63−0.112×age)×height(cm) female: vital capacity(ml)=(21.78−0.101×age)×height(cm)
What is "normal" efficiency?
Efficiency (statistics) In the comparison of various statistical procedures, efficiency is a measure of quality of an estimator, of an experimental design, or of a hypothesis testing procedure. Essentially, a more efficient estimator, experiment, or test needs fewer observations than a less efficient one to achieve a given performance.
What is normal mean cell volume?
Mean corpuscular volume (MCV) is a value related to your red blood cells. An average MCV score is between 80 and 95. If the MCV goes up to an extreme of 125, it may indicate vitamin B12, folate deficiencies, or cold agglutinin disease. A higher MCV value indicates that the red blood cells are larger than the average size.

What is a good FVC?
The normal value for the FEV1/FVC ratio is 70% (and 65% in persons older than age 65). When compared to the reference value, a lower measured value corresponds to a more severe lung abnormality.
What is normal FVC in liters?
Forced Vital Capacity (FVC) Forced vital capacity is the total amount of air that can be exhaled following a deep inhalation in an FVC test. Thenormal FVC range for an adult is between 3liters and 5liters.
What is a normal FVC in mL?
For FEV1 and FVC, the best two values should be within 5% or 150 mL of each other, whichever is greater. If FVC is <1.0 L, then the values should be within 100 mL. The best FEV1 and FVC can be taken from different manoeuvres.
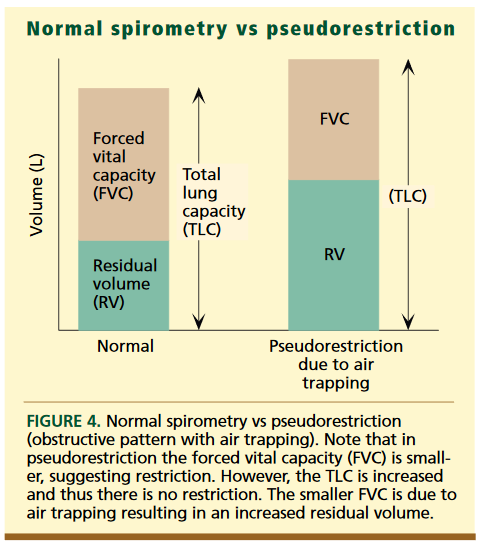
What is an abnormal FVC?
FVC measurement An “abnormal” FVC could be due to restrictive or obstructive lung disease, and other types of spirometry measurements are required to determine which type of lung disease is present.
Is an FVC of 1.78 normal?
Average normal values in healthy males aged 20-60 range from 5.5 to 4.75 liters, and average normal values for females aged 20-60 range from 3.75 to 3.25 liters.
What is FVC in COPD?
A COPD diagnosis requires a calculation involving both FEV1 and another breathing measurement called FVC, or forced vital capacity. FVC is a measurement of the greatest amount of air you can forcefully breathe out after breathing in as deeply as you can.
What is a good lung capacity?
Lung capacity or total lung capacity (TLC) is the volume of air in the lungs upon the maximum effort of inspiration. Among healthy adults, the average lung capacity is about 6 liters.
What value indicates a lung problem?
The ratio of FVC and FEV1 can help doctors diagnose the specific type of lung disease a person has. To calculate this ratio, a doctor divides the FVC reading by the FEV1 result. When the value of FEV1 is less than 70% of an FVC in adults or below 85% in those aged 5–18 years, an obstruction may be present.
What is normal lung capacity by age?
Did you know that the maximum amount of air your lungs can hold—your total lung capacity—is about 6 liters? That is about three large soda bottles. Your lungs mature by the time you are about 20-25 years old. After about the age of 35, it is normal for your lung function to decline gradually as you age.
What is FEV1 FVC in asthma?
Obstruction of airflow is defined by a reduced FEV1 (forced exhalation volume in one second) to FVC (forced vital capacity). This is a result in a relatively greater decrease in FEV1 compared to FVC, whereas in restrictive disease these 2 parameters decrease proportionally and the FEV1/FVC ratio does not change.
What percentage of lung function is needed to live?
Answer. 30 percent lung capacity, as you may have guessed, is not great. It means your lungs are functioning only a third as well as a healthy person's. This will be determined by Pulmonary Function Tests (PFTs), which are used to assess lung size and air flow.
How can I strengthen my lungs?
Follow these nine tips and to help improve your lung health and keep these vital organs going strong for life:Diaphragmatic breathing. ... Simple deep breathing. ... 'Counting' your breaths. ... Watching your posture. ... Staying hydrated. ... Laughing. ... Staying active. ... Joining a breathing club.More items...
What is the FVC range?
Thenormal FVC range for an adult is between 3liters and 5liters.
What is FVC in spirometry?
Measuring forced vital capacity (FVC) is part of a spirometry or pulmonary function test that is conducted to assess lung health, airflow, and help in disease diagnosis and effectiveness of medical treatment. Forced vital capacity is the amount of air that can be forcibly exhaled from your lungs after inhaling as deeply as possible.
What is Forced Vital Capacity?
Forced vital capacity is a measurement of lung size (in liters) and represents the volume of air in the lungs that can be exhaled following a deep inhalation.
What is the VC of air?
Vital capacity (VC) refers to the maximal volume of air that can be expired following maximum inhalation. It is the total of tidal volume, inspiratory reserve volume, and expiratory reserve volume:
What are the three key spirometry measurements?
The three key spirometry measurements (FVC, FEV1 and FEV1/FVC ratio) for a given individual are compared to reference values.
What is the FEV1/FVC ratio?
The reality is that for an FEV1/FVC ratio between 100% of predicted and say, the LLN, there is a continuum of probabilities that a patient does or does not have airway obstruction. The other reality is that humans do not do well with shades of gray and prefer black and white. So choose a cutoff that makes clinical sense to you but at ...
What is the difficulty in creating an evidence-based cutoff?
This does not mean however, that a subject that has not been hospitalized, is not on medication and appears healthy is actually “normal” and this has to be part of the reason why population studies show bell-shaped curves.
Is FEV1 a factor in airway obstruction?
It should also be remembered that the FEV1/FVC ratio is not the sole factor in diagnosing airway obstruction. A 10% decrease (or even increase) in a patient’s FEV1 from one visit to another would be considered to be a significant change and clinically would likely be taken as an indication of underlying airway obstruction. A patient that had baseline spirometry that was WNL but showed a significant increase in FEV1 following a bronchodilator or a significant decrease in FEV1 during a methacholine challenge would also likely to be considered to have airway obstruction or at least the clinical potential for it. Finally, there is a small fraction of asthmatics that show a symmetrically decreased FVC and FEV1 with a normal FEV1/FVC ratio (and often a normal peak flow!) during exacerbations who in a sense aren’t even on the radar in this discussion.
What is the normal FVC ratio?
If your FVC is decreased but the ratio of FEV1/FVC is normal, this indicates a restrictive pattern. A normal ratio is 70% to 80% in adults and 85% in children. 1
What is FVC in breathing?
FVC, forced vital capacity, is the full amount of air that can be exhaled with effort in a complete breath. 1
How does spirometry measure FEV1?
In measuring FEV1/FVC via spirometry, the amount of air you exhale in one second is recorded, as well as the total amount of air you are able to exhale. A normal result is based on your age, weight, and sex. This is called the predicted value.
How long does it take to get a FEV1?
FEV1/FVC is just one of several measurements taken when using a spirometer. The test can be done in your doctor's office and takes about 45 minutes. What to Expect From a Spirometry Test.
Why do you need to measure FEV1?
Measuring your FEV1/FVC ratio at regular intervals can help assess how well treatment is working or how your condition is progressing.
Does smoking affect FEV1?
Yes. Research has shown that FEV1 and FVC levels are worsened by smoking, especially among people who have smoked for a longer period of time and/or have smoked more cigarettes overall. 6
What is the measurement of FVC?
One of the primary spirometry measurements is FVC, which is the greatest total amount of air you can forcefully breathe out after breathing in as deeply as possible. If your FVC is lower than normal, something is restricting your breathing.
What is the result of FVC?
For adults: FVC. Result. is greater than or equal to the lower limit of normal. normal. is less than the lower limit of normal. abnormal. An abnormal FVC could be due to restrictive or obstructive lung disease, and other types of spirometry measurements are required to determine which type of lung disease is present.
What is normal on a blood test?
Your result is considered “normal” if your score is 80 percent or more of the predicted value.
What percentage of a test is normal?
Once you’ve done the test, they look at your test score and compare that value to the predicted value. Your result is considered normal if your score is 80 percent or more of the predicted value. You can get a general idea of your predicted normal value ...
How do you find out your COPD stage?
If you are showing symptoms of COPD, you should contact a doctor. If your doctor thinks you may have COPD, they will recommend breathing tests. These tests measure how healthy your lungs are and how well you can breathe. 1
What tests are used to determine your COPD Stage?
A COPD stage is determined with results from 2 breathing tests called spirometry tests. These tests are used to measure how well your lungs are working. 3
What happens during the spirometry tests?
The same machine is used for the FVC and FEV1 tests, and the tests use the same basic technique. This machine is called a spirometer. The spirometer has an attached mouthpiece to blow into during the tests and a sensor to measure the air you blow.
What do the test results mean?
Your doctor will use your spirometry test results and information about your symptoms to determine your COPD stage. One result from the test is the ratio of FEV1/FVC. This ratio combines both test results and is reported as a percentage or a decimal. The lower this value is, the less efficiently the lungs are working. 1,4
What other factors impact your COPD stage?
In the past, COPD stage was decided only based on spirometry test results. These test results do give important information on how well your lungs are working. But they do not determine everything about someone’s COPD. Two people could have similar spirometry test results but have different symptoms and challenges. 1
What are pulmonary function tests?
Pulmonary function tests (PFT’s) are non-invasive breathing tests employed for diagnosing and monitoring lung diseases. They are also commonly referred to as lung function tests. The most commonly performed PFT’s include spirometry, plethysmography, and diffusion studies.
Why has my physician ordered pulmonary function tests for me?
Your physician may order PFT’s for you if you have the signs or symptoms of a lung disorder.
What do pulmonary function tests detect?
Pulmonary function tests are used to assess how well your lungs are functioning. They measure lung volumes, lung capacity, rates of flow of gases, and the efficiency of gas exchange.
Are there any risks involved?
A pulmonary function test is a non-invasive, painless and relatively safe procedure. Complications arise rarely.
What are the contraindications of undergoing a pulmonary function test?
It is not advisable to go for a PFT if- – You have undergone an abdominal or chest surgery recently. – You have had eye surgery in the recent past (2 weeks)- there is a risk of increasing the pressure inside the eyes during forced expiration. – You are suffering from an active pulmonary infection including tuberculosis. – You have been diagnosed with an aneurysm (ballooning of a major blood vessel). – You suffer from a pneumothorax (air between your lungs and the chest wall). – You have a history of recent myocardial infarction or unstable angina pectoris..
Is it safe for me to undergo a pulmonary function test if I am pregnant or lactating?
Yes, it is safe to undergo a PFT if you are pregnant or breastfeeding your child. Regular monitoring of pulmonary function tests may prove to be of great value in pregnant females as the presence of a lung disorder can be detected early and can be managed accordingly.
How should I prepare for a pulmonary function test?
Spirometry, the most commonly performed PFT is carried out as an outpatient procedure. No sedation is given, and you will be conscious during the procedure.
What is the FEV1/FVC threshold?
A percent of predicted, which for the FEV1/FVC ratio is most commonly either 95% or 90% of predicted has frequently been used as a threshold. This approach is not supported by any official group and has its roots in the ITS Snowbird workshops in the early 1970’s and NIH recommendations around that time.
What is the bottom 5th percentile of a study population?
The primary decision behind the LLN is that the bottom 5th percentile of any study population has a high probability of being abnormal. This concept is frequently used in biological research and appears to have a significant level of statistical relevance.
Why is the bottom 5% of the population abnormal?
Because it is dependent upon a specific study it will be different depending on which reference equations are in use. The decision that the bottom 5% of the population is abnormal is somewhat arbitrary and may underestimate the presence of airway obstruction.
Is FEV1/FVC arbitrary?
To some extent any threshold value for the FEV1/FVC ratio is arbitrary and there are limitations to any approach. At this time however, the preponderance of evidence and opinion is in favor of the LLN so the recommendation has to be for those interpreting pulmonary function tests to use the LLN for all reference values, including the FEV1/FVC ratio, unless there are clear and overwhelming reasons not to. At the same time it is also important to remember there is a certain amount of overlap between normal and abnormal in pulmonary function results and for this reason individuals on the borderline are not clearly one or the other without accompanying symptoms.
Is normalcy a conditional starting point?
In the final analysis each approach is relatively arbitrary to one degree or another and none are supported by clear clinical correlations. The concept of normalcy however, is not easily pinned down and all approaches should be considered a conditional starting point for the interpretation of pulmonary function results.
Is FEV1/FVC ratio dependent on FVC?
In addition, the accuracy of the FEV1/FVC ratio is dependent on the individual accuracy of the FVC and FEV1 measurements and this places a limitation on the accuracy of any FEV1/FVC ratio threshold.
What is flow volume shape?
The flow-volume shape can take on a few distinguishable shapes that correspond to a certain type of pathology: normal spirometry. pathological spirometry. obstructive lung disease. restrictive lung disease. mixed lung disease.
What is the peak of a flow volume loop?
After the starting point the curve rapidly mounts to a peak: Peak (Expiratory) Flow.
What happens after the PEF curve?
After the PEF the curve descends (=the flow decreases) as more air is expired. A normal, non-pathological F/V loop will descend in a straight or a convex line from top (PEF) to bottom (FVC).
Why is FET higher?
The FET ( Forced Expiratory Time) will be higher due to the lower flow but equal volume.
How many different shapes of flow-volume loops can be distinguished?
Three different shapes of flow-volume loops can be distinguished.
Is FEV1 ratio a percentage?
This is true for all parameters except the ratios, like FEV1-ratio (or Tiffeneau index). Since FEV1 ratio is a percentage (FEV1/FVC%) it did not make sense to compare this value to a predicted value, in stead it was said FEV1 ratio was too low if it was less than 70%.
Do FEV1 and FVC come from the same test?
This means that FEV1, FVC and all other parameters do not necessarily come from the same test. Consider the following situation:

Risks and Contraindications
- FVC requires your cooperation and effort, but it is safe. However, be sure to have medical supervision the first time you use a spirometer, the device used to measure your FVC. You could potentially use a spirometer the wrong way, exhausting yourself. Afterward, you may be instruct…
Before The Test
- Before your FVC test, your healthcare provider may give you instructions regarding your medication. You may also be directed to use your inhaler (or another treatment) so your medical team can assess how well it is working. A lung infection or exposure to cigarette smoke can affect your results, too. It's important that you discuss these issues with your healthcare provide…
During The Test
- When you arrive for your test, you will be asked to sign in and provide your paperwork. You will meet a medical team, which may include a technician, nurse, and/or doctor.
Interpreting Results
- Your total FVC volume can be compared with the standard FVC for your age, sex, height, and weight. Your FVC can also be compared with your own previous FVC values. This can determine whether your pulmonary condition is progressing or if your lung function is improving under treatment. Forced vital capacity will be reported in two ways: 1. As an absolute value, reported a…
Follow-Up
- You may need to have further testing after your FVC is done or after your FVC/FEV1 ratio is calculated. For example, respiratory symptoms with a normal FEV1/FVC ratio suggest a restrictive pattern. You may need to have full pulmonary function tests and imaging tests, such as a chest/lung computerized tomography (CT). If the FEV1/FVC ratio is low, it suggests obstructive l…
Summary
- An FVC test helps evaluate your lung function. It measures how much air you can forcibly exhale after taking a deep breath. This helps determine whether you have an obstructive lung condition, which makes it hard to exhale, or a restrictive condition, which makes it hard to inhale. When you take the test, your doctor will ask you to breathe into a tube. You'll take a deep breath and then bl…
A Word from Verywell
- While FVC is a valuable measurement in evaluating lung disease, it is important to remember that it is just a number. Your healthcare provider will look at your medical condition, your general health, and other findings. That will help them understand how your FVC measurement fits into the big picture of your health.
Purpose of FEV1/FVC Test
Risks and Contraindications
Interpreting Results
Follow-Up
Summary
- The FEV1/FVC ratio indicates how much air you can forcefully exhale. It's measured by spirometry, a test used to diagnose or monitor lung conditions. The FEV1 measures how much air you can exhale in one second. The FVC measures the total amount of air you can exhale forcefully in one breath. Your healthcare provider can use the FEV1/FVC ratio to he...
A Word from Verywell