What causes high peak pressures?
- Peak pressure: This is the pressure that is generated by the ventilator to overcome BOTH airway resistance AND alveolar resistance.
- Plateau pressure: This is the pressure that is essentially left over in the lung after the tidal volume has been delivered.
- High Peak pressures and normal plateau indicate an issue with elevated resistance
What does increases mean airway pressure?
Mean airway pressure improves oxygenation by allowing the re-distribution of oxygen from highly compliant alveoli (more stretchy) too less compliant alveoli (stiffer). When the ventilator delivers a breath, regardless of whether it’s a volume or pressure delivered breath, the mean airway pressure is increased and therefore improves oxygenation.
What is the normal range for peak pressure?
Some of the suggested lifestyle changes by the physicians are as follows:
- Quit smoking
- Lose weight
- Avoid alcohol or at least limit the intake
- Eat a low-sodium and low-fat diet such as the DASH diet
- Avoid too much of stress
- Eat foods rich in potassium, magnesium, and calcium such as bananas and milk
- Regular monitoring of blood pressure after reaching the age of 35 years
- Practice meditation and other stress-relieving exercises
What is normal mean airway pressure?
Ventilatory Values:
- Tidal Volume (VT): > 5 mL/kg
- Vital Capacity (VC): 65 – 75 mL/kg
- Minute Ventilation (VE): 5 – 8 L/min
- Mean Airway Pressure (MAP): 5 – 10 cmH2O
- Maximum Inspiratory Pressure (MIP): > -20 cmH2O
- Maximum Expiratory Pressure (MEP): > +40 cmH2O
- Rapid Shallow Breathing Index (RSBI): < 100
- Deadspace-to-Tidal-Volume Ratio (VD/VT): < 60%
What is a normal peak pressure on a ventilator?
Peak pressure is graphed as a summation of both initial airway resistance and lung compliance. In general, an acceptable maximum Ppeak is 40 cmH2O.
What is a normal mean airway pressure?
The normal value of 10–15 mmHg frequently exceeds 200 mmHg in the critically ill patient with respiratory failure. The alveolar partial pressure of oxygen is determined using Dalton's law which states that the gases in the closed space of the alveolus must equal barometric pressure (generally assumed to be 760 mmHg).
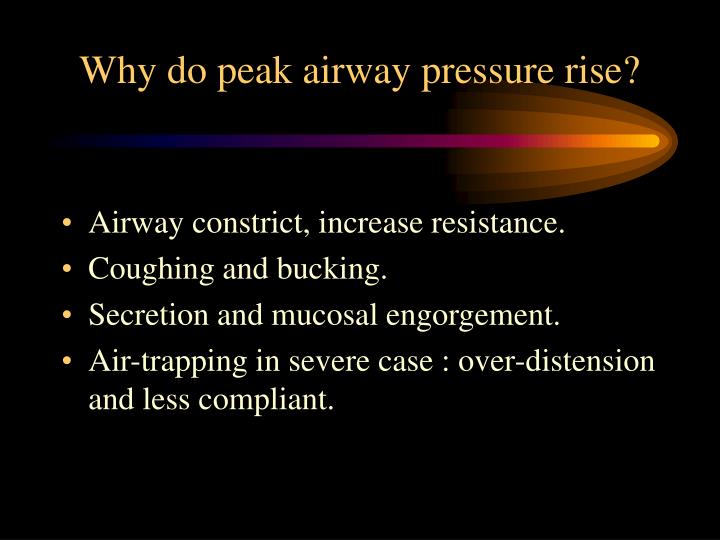
What does an increase in peak airway pressure mean?
Peak airway pressure increase is a late warning sign of partial endotracheal tube obstruction whereas change in expiratory flow is an early warning sign. Anesth Analg.
What is peak airway pressure and plateau pressure?
Peak pressure: This is the pressure that is generated by the ventilator to overcome BOTH airway resistance AND alveolar resistance. Plateau pressure: This is the pressure that is essentially left over in the lung after the tidal volume has been delivered.
What is PEEP and PIP?
PEEP improves gas exchange by increasing the functional residual capacity, reduces the respiratory effort, lowers requirements for respiratory mixture oxygen, and enables to decrease the peak inspiratory pressure (PIP) without decreasing the mean airway pressure.
What is a high PIP?
The peak inspiratory pressure (PIP) is the highest pressure measured during the respiratory cycle and is a function of both the resistance of the airways and the compliance of the respiratory system.
What is a normal PIP on ventilator?
Normal peak inspiratory pressure (PIP) is 25-30 cm H2O. Peak inspiratory pressure (PIP) should be kept below 20 to 25 cm H2O whenever positive-pressure ventilation is required, especially if pneumothoraces, or fresh bronchial or pulmonary suture lines, are present.
What causes low peak pressure on ventilator?
Some causes for low pressure alarms are: The patient becomes disconnected from the ventilator circuit. Inadequate inflation of the tracheostomy tube cuff. Poorly fitting noninvasive masks or nasal pillows/prongs. Loose circuit and tubing connections.
What is the difference between PPV and CPAP?
Unlike CPAP, in which air is delivered constantly via a machine, PEEP often refers to air that's manually delivered by a manual resuscitation bag (MRB). (MRBs are often used to help newborns breathe, and aren't typically used for sleep apnea therapy.)
What is IE ratio?
The I:E ratio denotes the proportions of each breath cycle devoted to the inspiratory and expiratory phases. The duration of each phase will depend on this ratio in conjunction with the overall respiratory rate. The total time of a respiratory cycle is determined by dividing 60 seconds by the respiratory rate.
How is mean airway pressure measured?
Mean airway pressure (Paw) is determined by PIP, the fraction of time devoted to the inspiratory phase (TI/Ttot, where Ttot is total respiratory cycle time), and PEEP.
What is the difference between NIV and CPAP?
While there are similarities with regard to the interface, NIV is not the same as continuous positive airway pressure (CPAP), which applies a single level of positive airway pressure throughout the whole respiratory cycle; CPAP does not deliver ventilation but is occasionally used in conditions also treated with NIV.
What is the airway pressure?
As the term suggests, ‘airway pressure’, is the pressure that occurs due to the resistance exerted by the airway. In the case of human beings, the airway refers to the respiratory tract (such as the trachea, bronchus, etc) and the alveoli of the lungs. In the case of the ventilators, the airway tract also includes the parts ...
What are the two types of airway pressure?
The airway pressure is further classified into two types. They are the peak pressure and the plateau pressure. Here we will be discussing these types of pressures in depth.
What is the highest level of ventilation pressure?
The value of PIP should never exceed 40 cm H2O in a normal condition. In the case of a ventilator, PIP also includes instruments for air supply such as an endotracheal tube and the breathing tube.
Why is my lungs low compliance?
Some of the reasons are as follows. Pneumonia :- It is a type of infection that inflames the air sac of one or both lungs. Pulmonary Edema :- It refers to the accumulation of fluid inside the tissues and the air sacs of the lungs.
Is lung compliance proportional to volume?
From the above equation, we can conclude that lung compliance is directly proportional to the change in volume and inversely proportional to the change in transpulmonary pressure. It is independent of airway resistance. If the lung compliance is low, more pressure is required to inflate the lungs and vice versa.
What is the plateau pressure?
More precisely, it’s the ‘transpulmonary Pplat’ that’s the most direct marker of lung stress, but that’s a discussion for another day. For determining lung stress, knowing the Pplat still brings you much closer to the truth than simply knowing PIP. From this discussion, it becomes clear that the higher the ratio of resistive and elastic loads, the greater would be the difference between PIP and Pplat. This can occur when resistance is high (e.g. asthma), and/or when inspiratory flow is set high on the vent.
Where is resistance pressure dissipated?
Resistive pressure is dissipated entirely in parts of the respiratory system that contribute to resistance (mainly small airways). On the other hand, elastic pressure is “spent” on the elastic structures: lung and chest wall. For simplicity, we will ignore the effect of chest wall for now.
What is the airway pressure used to augment inspiration?
The airway pressure used to augment inspiration is most commonly 30 cm H2 O , although some centers have used 20 cm H 2 O. Jacket inflation must be maintained until lung emptying is complete, and care is required to ensure that air is not forced into the stomach during inflation. The procedure is repeated until at least two technically satisfactory and repeatable maneuvers have been recorded, 17 with values generally being reported from the best curve (i.e., that with the highest product of forced vital capacity (FVC) and either forced expiratory volume in 0.5 second (FEV 0.5) or forced expiratory flow at 75% of expired FVC (FEF 75%) (discussed later). Figure 9-30 shows the relationship between a partial forced expiratory maneuver initiated from end-tidal inspiration and that recorded from the same infant after lung volume was raised with an inflation pressure of 30 cm H 2 O.
What happens if a ventilator does not release airway pressure?
If the ventilator does not release the airway pressure often enough, carbon dioxide concentrations would rise and cause predictable effects . Once the inspiratory time has been achieved, exhalation occurs, and airway pressure is released to a lower pressure (P low) for the time of exhalation (T e ).
What is the effect of distending airway pressure on hyaline membrane disease?
Application of distending airway pressure to the airway of patients with hyaline membrane disease brings about a prompt reduction in venous admixture. The reduction in venous admixture results from a decrease in intrapulmonary right-to-left shunting as well as a decrease in right-to-left shunting across the foramen ovale.
What is the PEEP in a patient?
The lower airway pressure is PEEP if the exhalation airway pressure is supra-atmospheric. However, if the exhalation pressure is equal to atmospheric pressure, it is the P low. To avoid confusion, the term P low is used to refer to the exhalation pressure. Carbon dioxide is removed from the patient’s lungs during exhalation.
What is APRV ventilation?
Airway pressure release ventilation (APRV) is a mode of mechanical ventilation that was introduced to improve oxygenation in spontaneously breathing patients (Figure 18-10 ). With APRV, the pressure in the ventilator circuit alternates between a high and a lower level (normally the high pressure level is of longer duration than the lower pressure level) and spontaneous breathing is allowed in any phase of the cycle. The high- and low-pressure levels, the rate of change between the two levels, the respiratory system compliance, and the airway resistance to flow are the main determinants of the “mechanical ventilation” portion with APRV, whereas the complementary “spontaneous breathing” portion mainly depends on the patient's respiratory drive. In contrast to continuous positive airway pressure (CPAP), APRV interrupts P VENT briefly to augment spontaneous minute ventilation and thereby increases alveolar ventilation and CO 2 removal without increasing the work of breathing. Spontaneous efforts during APRV are not actively assisted except for those breaths that happen to occur during the change from the lower to the upper pressure level. Total minute ventilation with APRV is the sum of the mechanical, pressure-controlled ventilation and the complementary spontaneous breathing. APRV without spontaneous breathing is essentially the same as PCV.
Is spontaneous breathing assisted during APRV?
Spontaneous efforts during APRV are not actively assisted except for those breaths that happen to occur during the change from the lower to the upper pressure level. Total minute ventilation with APRV is the sum of the mechanical, pressure-controlled ventilation and the complementary spontaneous breathing.
What is high peak inspiratory pressure?
High peak inspiratory pressures are associated with pneumothorax, whereas elevated mean airway pressures are associated with pneumothorax and reduction in cardiac output.73 It is not clear whether high peak inspiratory pressures are a primary or secondary phenomenon associated with the generation of pneumothorax.
What are the parameters of a ventilator?
Various parameters can be preset on most ventilators, including the respiratory rate, PIP, PEEP, inspiratory time, and gas flow rate . When adjusting these parameters it is necessary to consider the pathologic condition present in the lung. Infants with primary pulmonary hypertension have very compliant lungs that are easily overdistended. In these patients adequate minute ventilation may be achieved with low PIP and PEEP, a short inspiratory time, and a moderate respiratory rate. Conversely a child with ARDS has noncompliant lungs and may require a relatively high PIP and PEEP, a short inspiratory time, and a high respiratory rate to achieve adequate alveolar ventilation. Obstructive disorders such as meconium aspiration syndrome and asthma have a longer time constant and require ventilation at a slower rate. After determining the initial settings, however, the patient's response must be evaluated and adjustments must be made to stay abreast of dynamic changes in pulmonary compliance and resistance that occur over time.
What is a continuous flow ventilator?
For use in infants, ventilators were modified to provide continuous flow throughout the respiratory cycle. 14 A continuous flow device refers to a ventilator in which the flow of respiratory gas occurs throughout the respiratory cycle. Most infant ventilators are continuous flow devices (e.g., Infant Star, Baby Bird). In most continuous flow infant ventilators, inspiratory valves are lacking, and the cycling is controlled by the exhalation valve. Closure of the exhalation valve begins inspiration, and the flow of gas going through the circuit is diverted to the patient. If the inspiratory flow rate is low (1 to 3 L/kg) and if the PIP is not limited, the tidal volume delivered by the patient can be calculated from the inspiratory flow rate and the inspiratory time. This would result in a time-cycled, volume-regulated breath. For pressure-control ventilation, the flow rates used are usually higher (4 to 10 L/kg). Once the preset PIP is reached, the excess flow is vented through a pressure relief valve, and the lungs are maintained in inflation throughout the rest of inspiration. During exhalation, there is continuous flow of gas, allowing the patient to breathe from the circuit rather than open a demand valve. A demand flow ventilator refers to a ventilator that allows inspiratory flow of gas to the patient between ventilator breaths through a demand valve that is opened by the patient’s inspiratory efforts. Work of breathing is higher with a demand flow ventilator compared with a continuous flow device because of the effort required to open the demand valve.
What is PEEP in lung?
1. PEEP in part determines lung volume during the expiratory phase, improves ventilation-perfusion mismatch, and prevents alveolar collapse. 2. PEEP contributes to the pressure gradient between the onset and end of inspiration, and thus affects the tidal volume and minute ventilation.
What is the goal of assisted respiratory support?
The goal of assisted respiratory support, whether invasive (ETT) or less invasive (nasal CPAP, high-flow nasal cannula, NIPPV, BIPAP, or HFNV), is to keep the lung ventilation in the midportion of the PV curve. Expiratory flow is dependent on the elastic and resistive properties of the lung. On assisted ventilation, the slope of the expiratory waveform plays a role also. A too rapid (steep slope) decline of the expiratory wave may lead to air-trapping and movement away from the midportion of the PV curve. This can be especially true of the patient with established BPD or evolving BPD. Latzin et al. used time of peak tidal expiratory flow (tPTEF) divided by expiratory time (tE) to measure compliance ( Fig. 12-8 ). Patients with BPD had decreased tPTEF/tE suggestive of poorer lung compliance.
How does PIP affect ventilation?
Physiologic effects. 1. PIP in part determines the pressure gradient between the onset and end of inspiration and thus affects the tidal volume and minute ventilation. 2. During volume ventilation, an increase in tidal volume corresponds to an increase in PIP during pressure ventilation.
What is the most common complication of mechanical ventilation?
Barotrauma is the most commonly associated complication of mechanical ventilation, with the literature suggesting an incidence of between 7% and 25%. 75 Much of the difference depends on the case mix in a particular study as well as the definition of barotrauma used.
What are the variables that affect airway pressure?
Before you make changes to the ventilator, recall the variables that affect airway pressures. These can be divided into two categories; resistance and compliance . Resistance (∆ Pressure/Flow) is a measurement of air flow from the ventilator through the airways. Compliance (∆ Volume/ ∆ Pressure) describes the degree to which the lung and chest wall can stretch. The more pressure required to inflate the lung and expand the chest wall, the lower the compliance. A high airway pressure alarm is signaling a problem with resistance or compliance.
What does it mean when a ventilator has a high airway pressure alarm?
A high airway pressure alarm is signaling a problem with resistance or compliance . The first thing to do is turn up the upper limit on the alarm parameter to stop the alarm and ensure that the patient receives the set breath from the ventilator.
