
What is the difference between Nug and ANUG?
Necrotizing ulcerative gingivitis, (NUG), or simply necrotizing gingivitis (NG), is a common, non-contagious infection of the gums. Acute necrotizing ulcerative gingivitis (ANUG) is the acute presentation of NUG, which is the usual course the disease takes.
What is the scientific name for Nug?
NUG has been recognized for centuries. It has been given many names: Vincent's disease, fusospirochetal gingivitis, trench mouth, acute ulcerative gingivitis, necrotizing gingivitis, and acute NUG.[1]
What is necrotizing ulcerative gingivitis (NUG)?
Necrotizing ulcerative gingivitis (NUG) is a typical form of periodontal diseases. It has an acute clinical presentation with the distinctive characteristics of rapid onset of interdental gingival necrosis, gingival pain, bleeding, and halitosis. Systemic symptoms such as lymphadenopathy and malaise could be also found.
What is trench mouth (Nug)?
Trench mouth, also known as necrotizing ulcerative gingivitis (NUG), is a severe form of gingivitis that causes painful, infected, bleeding gums and ulcerations.
How is ANUG dental treated?
Treating ANUG typically requires antibiotics and dental treatment. Irrigation of the mouth with salt water or peroxide solution often helps to relieve symptoms. Rest, a balanced diet, no smoking, and avoiding hot and spicy foods are also important.
How do you treat a patient with ANUG?
The treatment of NUG is based on combining mechanical removal of tartar with local and systemic delivery of antimicrobial agents. Adequate treatment usually prevent the progression of the disease and ulcer healing is expected in a few days.
How do you get ANUG?
Acute necrotizing ulcerative gingivitis (ANUG) occurs most frequently in smokers and debilitated patients who are under stress. Other risk factors are poor oral hygiene, nutritional deficiencies, immunodeficiency (eg, HIV/AIDS, use of immunosuppressive drugs), and sleep deprivation.
What are the symptoms of ANUG?
A person with ANUG may have:Fever.Red and swollen gums.Gums that bleed easily.Gum pain.Bad taste in the mouth or very bad breath.Gray buildup on the gums.Large sores or loss of gum in between teeth.
How long does it take ANUG to heal?
Taken together with chlorhexidine, a prescription antibacterial mouth rinse, and saline (mild saltwater) rinses, symptoms should subside within 24 to 48 hours. It is also important to treat the underlying conditions that led to the ANUG in the first place.
What causes NUG?
The predisposing factors play a main role on NUG by the downregulation of the host immune response facilitating bacterial pathogenicity, these factors include: psychological stress and insufficient sleep, poor diet, alcohol and tobacco consumption, inadequate oral hygiene, preexisting gingivitis, and systemic condition ...
How serious is ANUG?
Treatment of ANUG is by removal of dead gum tissue and antibiotics (usually metronidazole) in the acute phase, and improving oral hygiene to prevent recurrence. Although the condition has a rapid onset and is debilitating, it usually resolves quickly and does no serious harm.
Is ANUG contagious?
ANUG is a non-communicable disease characterized by rapid destruction of the gum tissue or gingival tissue and may prove a dangerous infection in the context of immunocompromised patients in which the host immune response is impaired as in systemic disorders and diseases.
Is ANUG reversible?
If caught early, though, ANUG is highly treatable and reversible. After determining you have ANUG and not another condition, our first step is to relieve the symptoms with non-steroidal anti-inflammatory drugs (NSAIDs) like ibuprofen to manage pain and reduce swelling.
How do you prevent ANUG?
Prevention of Trench Mouth or ANUG Maintain good oral hygiene . Regular dental check-up and cleans , preferably every six months. Reduce stress. Avoid irritants such as smoking and hot or spicy foods.
Is there bone loss with NUG?
Loss of attachment and bone are rare in NUG, but may be associated with multiple episodes over time or NUG may be superimposed upon existing periodontitis. NUG is an infectious disease most associated with a fusiform-spirochete bacterial flora.
Does ANUG affect the tongue?
Acute Necrotizing Ulcerative Gingivitis (ANUG) ANUG, also known as Vincent disease or trench mouth, has a sudden onset with gingiva showing punched-out crater-like ulcerations, covered with a whitish pseudomembrane, surrounded by a demarcated zone of erythema. Any area of the mouth can be affected.
How do you treat ANUG at home?
At home, people are instructed to rinse with salt water, a hydrogen peroxide solution (ordinary drugstore hydrogen peroxide mixed half-and-half with water), or chlorhexidine (an antiseptic). Rinsing may be recommended instead of brushing for the first few days because of the sensitivity of the gums.
Can you cure ANUG?
ANUG is very treatable and completely reversible if caught early. Most importantly, contact your dentist or a periodontist (a dentist specializing in the diagnosis and treatment of gum diseases), to confirm that this is indeed what you have.
What antibiotic is used for trench mouth?
In some cases, the gums may take on a gray hue. What antibiotics are used to treat trench mouth? The most commonly prescribed antibiotic for trench mouth is Flagyl (metronidazole).
How do you prevent ANUG?
Prevention of Trench Mouth or ANUG Maintain good oral hygiene . Regular dental check-up and cleans , preferably every six months. Reduce stress. Avoid irritants such as smoking and hot or spicy foods.
Is Acute Necrotizing Ulcerative Gingivitis Curable?
ANUG is curable. Debridement of the ulcerated gingiva, scaling, and root planing to remove calculus along with hydrogen peroxide mouth rinse, chlor...
Is Trench Mouth Serious?
Trench mouth is an extension of acute necrotizing ulcerative gingivitis. If left untreated, this necrotizing ulcerative periodontitis or trench mou...
Is ANUG Contagious?
Acute necrotizing ulcerative gingivitis is non-contagious, meaning it is not transmissible and does not spread from one person to another.
Does ANUG Cause Pain?
ANUG causes gum pain along with fever, bad breath, bleeding gums, and ulcerations.
Will My Trench Mouth Go Away?
The trench mouth is curable. Antimicrobials and painkillers are given to relieve the infection and pain. Ultrasonic deep scaling, root planing, wou...
What Does Trench Mouth Smell Like?
The trench mouth causes ulceration of the gums and the formation of yellowish to white or grayish pseudomembrane. All these, along with plaque and...
What Does Trench Mouth Look Like?
Trench mouth is characterized by bad breath, altered taste, pus in the gums, bleeding gums, ulcerated gums, yellow or grayish membrane on the affec...
Does Gingivitis Occur Suddenly?
Usual gingivitis due to plaque build-up and poor oral hygiene is a slow, gradual process. In conditions like acute necrotizing ulcerative gingiviti...
Do Thrush and Trench Mouth Mean the Same?
Oral thrush and trench mouth are different. Oral thrush is caused due to fungal infection; typically, a candidal infection and trench mouth are cau...
Which Body Part Gets Affected by Acute Necrotizing Ulcerative Gingivitis?
ANUG affects the gingiva, especially the gum that is present in between two teeth. If left untreated, it progressively affects the underlying bone,...
What is NUG in dentistry?
NUG is a specific acute periodontal disease. The diagnosis seems evident according to the three typical clinical features as papilla necrosis, bleeding, and pain on the one hand and the identification of risk factors that alter the host response on the other hand. Treatment should be organized on successive steps, and the acute phase treatment should be provided immediately to prevent sequelae and craters in soft tissues that will lead to new relapses. Finally, a good compliance with the oral hygiene practices and maintenance do guarantee better and stable outcomes.
What is a NUG patient?
Necrotizing ulcerative gingivitis (NUG) is a typical form of periodontal diseases. It has an acute clinical presentation with the distinctive characteristics of rapid onset of interdental gingival necrosis, gingival pain, bleeding, and halitosis. Systemic symptoms such as lymphadenopathy and malaise could be also found. There are various predisposing factors such as stress, nutritional deficiencies, and immune system dysfunctions, especially, HIV infection that seems to play a major role in the pathogenesis of NUG. The treatment of NUG is organized in successive stages: first, the treatment of the acute phase that should be provided immediately to stop disease progression and to control patient's feeling of discomfort and pain; second, the treatment of the preexisting condition such as chronic gingivitis; then, the surgical correction of the disease sequelae like craters. Moreover, finally, maintenance phase that allows stable outcomes. This case report describes the diagnosis approach and the conservative management with a good outcome of NUG in a 21-year-old male patient with no systemic disease and probable mechanism of pathogenesis of two predisposing factors involved.
What is a NUG?
Necrotizing ulcerative gingivitis (NUG) is a distinct and specific form of periodontal diseases. It has an acute clinical presentation with the distinctive characteristics of rapid onset of gingival pain, interdental gingival necrosis, and bleeding.[1]
What is the diagnosis of a nug?
The diagnosis of NUG must be made fundamentally according to the presence or absence of primary clinical symptoms; the interproximal gingival necrosis often described by “punched out,” gingival bleeding with little or no provocation, and intensive pain which is a hallmark of this gingival lesion,[1,3,6] However it was found in an old data (Barnes et al1973) that 14% of cases of acute NUG had no pain and another 40% suffered only mild pain. (Barnes et al. 1973).[9] Fetid breath or “fetor ex ore” and pseudomembrane formation may be secondary diagnostic features.[1,3,6,10] Systemic signs and symptoms as lymphadenopathy, fever, and malaise have been also reported to occur in NUG.[1,6,10] However, lymphadenopathy is an infrequent finding. Its presence is probably related to the severity of the disease since it is usually observed in advanced cases.[1] In this case report, all primary, secondary, and systemic clinical symptoms are present except lymphadenopathy, and this indicates the less severity of the case. The typically clinical appearance of NUG is related to its histopathological aspect. Four different layers have been described from the most superficial to the deepest layers of the lesion (Listgarten et al. 1965):
What are the factors that contribute to NUG?
Other factors such as tobacco smoking, [3] preexisting gingivitis, and trauma have been reported as predisposing factors of NUG.[1,6]
Is NUG a sign of HIV?
Hence, authors (Rowland, 1999) reported that NUG may be the first sign of HIV infection .[1,2,3]
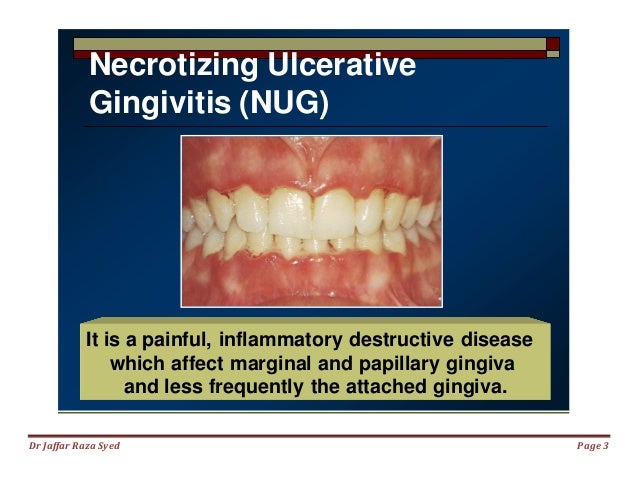
Necrotizing Ulcerative Gingivitis (NUG)
Acute infection of the gingiva characterized by gingival necrosis, bleeding and pain. NUG is diagnosed at the onset of specific clinical signs and symptoms. NUG is different from other periodontal diseases in that it presents with interdental necrosis, “punched out” ulcerated papillae, gingival bleeding and pain.
Presentation
Ulcerated and necrotic papillary and marginal gingiva and cratering (punched out) of papillae ( Figs. 1 and 2)
Treatment
Untreated, the infection may lead to rapid destruction of the periodontium (necrotizing ulcerative periodontitis) and can even spread, as necrotizing stomatitis or noma, into neighbouring tissues in the cheeks, lips or the bones of the jaw.
THE AUTHORS
Dr. Atout is an assistant professor in periodontology, division of periodontics, department of dental diagnostic and surgical sciences, faculty of dentistry, University of Manitoba, Winnipeg, Manitoba.
What is anug in ecstasy?
Drug addiction. ANUG is a problem that appears often in users of methamphetamine and ecstasy. Meth mouth is a condition which combines Acute Necrotizing Ulcerative Gingivitis with aggressive tooth decay.
How to treat acute necrotizing gingivitis?
Oral hygiene. Following a proper daily oral hygiene routine is essential for the treatment of Acute Necrotizing Ulcerative Gingivitis. Teeth should be brushed gently with a soft toothbrush at least twice a day after very meal and flossed at least once a day. If the gums feel very painful for brushing, an antiseptic mouthwash may be used for a few days for the home treatment of ANUG, until the pain subsides enough to allow brushing and flossing. Salt water rinses and hydrogen peroxide mouthwashes can also help soothe the pain of sore gums.
What Causes Acute Necrotizing Ulcerative Gingivitis?
The main cause of Acute Necrotizing Ulcerative Gingivitis is the excessive growth of certain harmful bacteria in the mouth, resulting in severe infection of the gums.
How to treat acute necrotizing ulcerative gum disease?
The main goals of the treatment of Acute Necrotizing Ulcerative Gingivitis are to stop the infection, relieve the symptoms and restore the damaged gum tissue using: Antibiotics and Pain Relief Medications. Dentists often prescribe antibiotics in order to fight the bacterial growth and prevent infection from spreading.
What causes trench mouth?
Several factors can increase the risk of developing trench mouth by disrupting the normal balance of bacteria in the mouth : Lack of dental care and overall poor dental hygiene allows the build-up of dental plaque on the gums and contributes to the development of ANUG.
What is the grayish film on the gums?
Grayish film on the gums, created by decomposed gum tissue, is one of the most characteristic symptoms of trench mouth.
Is trench mouth disease rare?
Although it can lead to serious complications if left untreated, treatment of trench mouth disease is, in most cases, simple and effective. It is now rare in developed countries, affect ing mostly people with a weakened immune system.
What is anug necrosis?
The hallmark sign of ANUG is necrosis and cratering of the interproximal papillae, referred to as “pun ched-out papillae.". Image courtesy of Craig Fowler, DDS. Often, ANUG can manifest without a significant odor, and it also may manifest as a localized condition.
How to treat anug?
Treatment of ANUG consists of gentle debridement with a hand scaler or ultrasonic device. Debridement is done over several days. The patient uses a soft toothbrush or washcloth to wipe the teeth.
What causes acute necrotizing ulcerative gingivitis?
Other risk factors are poor oral hygiene, nutritional deficiencies, immunodeficiency (eg, HIV/AIDS, use of immunosuppressive drugs), and sleep deprivation. Some patients also have oral candidiasis.
What is the progression of NUP into tissue beyond the mucogingival junction?
Progression of NUP into tissue beyond the mucogingival junction characterizes necrotizing stomatitis, which has many features in similar with cancrum oris.
Why does Anug occur in developing countries?
In developing countries, ANUG occurs mostly in malnourished children. Due to shared predisposing factors in a population (e.g. students during a period of examinations, armed forces recruits) ANUG is known to occur in epidemic-type patterns.
What is a NP?
Necrotizing ulcerative periodontitis (NUP, or simply necrotizing periodontitis, NP) or acute necrotizing ulcerative periodontitis (ANUP) is where the infection leads to attachment loss (destruction of the ligaments anchoring teeth in their sockets), but involves only the gingiva, periodontal ligament and alveolar ligament. Usually this spectrum of diseases result in loss of attachment, and therefore many ANUG diagnoses may be technically termed NUP, although ANUG is the term in most common use. NUP may be an extension of NUG into the periodontal ligaments, although this is not completely proven. In the meantime, NUG and NUP are classified together under the term necrotizing periodontal diseases.
What is a necrotizing periodontal disease?
Necrotizing periodontal diseases are a type of inflammatory periodontal (gum) disease caused by bacteria (notably fusobacteria and spirochaete species). The diseases appear to represent different severities or stages of the same disease process, although this is not completely certain. These diseases usually have a sudden onset, ...
Is NUP a periodontal disease?
NUP may be an extension of NUG into the periodontal ligaments, although this is not completely proven. In the mean time, NUG and NUP are classified together under the term necrotizing periodontal diseases.
What is anug in dentistry?
Acute necrotizing ulcerative gingivitis (ANUG) is a painful infection of the gums, causing fever, sometimes foul-smelling breath, and feeling ill. If the normal bacteria in the mouth overgrow, the gums can become infected. The gums hurt, and people sometimes have extremely bad breath. A professional cleaning, sometimes followed by hydrogen peroxide ...
What is the National Institute of Dental and Craniofacial Research?
National Institute of Dental and Craniofacial Research: This government site covers a wide variety of topics related to oral and dental health (in English and Spanish), including definitions of common terms and the latest information on clinical trials related to oral and dental diseases.
What is trench mouth?
Did You Know... Acute necrotizing ulcerative gingivitis (ANUG) used to be called trench mouth, a term that comes from World War I, when many soldiers in the trenches developed the infection. The infection is caused by an abnormal overgrowth of the bacteria that normally exist harmlessly in the mouth. Poor oral hygiene usually contributes ...
How long does it take to clean anug?
Treatment of acute necrotizing ulcerative gingivitis (ANUG) begins with a gentle, thorough, professional cleaning done over several days.
What is mouth health?
Mouth Healthy: This general resource provides information on oral health, including nutrition and guidance on selecting products that carry the American Dental Association's seal of approval. There is also advice on finding a dentist and how and when to see one.
Is ulcerative gingivitis contagious?
Acute necrotizing ulcerative gingivitis is not contagious.
Why is gingivitis important?
It's important to take gingivitis seriously and treat it promptly. Gingivitis can lead to much more serious gum disease called periodontitis and tooth loss. The most common cause of gingivitis is poor oral hygiene.
How does plaque cause gingivitis?
Here's how plaque can lead to gingivitis: Plaque forms on your teeth. Plaque is an invisible, sticky film composed mainly of bacteria that forms on your teeth when starches and sugars in food interact with bacteria normally found in your mouth. Plaque requires daily removal because it re-forms quickly. Plaque turns into tartar.
What is the name of the disease that causes redness and swelling in the gums?
Gingivitis is a common and mild form of gum disease (periodontal disease) that causes irritation, redness and swelling (inflammation) of your gingiva, the part of your gum around the base of your teeth. It's important to take gingivitis seriously and treat it promptly. Gingivitis can lead to much more serious gum disease called periodontitis ...
Can anyone develop gingivitis?
Gingivitis is common, and anyone can develop it . Factors that can increase your risk of gingivitis include:

Necrotizing Ulcerative Gingivitis
Presentation
- Population 1. Usually young adults (age 18-30) Signs 1. Can be localized or generalized with rapid/sudden onset and intense pain 2. Acute clinical presentation with distinctive characteristics of rapid onset of: 2.1. Ulcerated and necrotic papillary and marginal gingiva and cratering (punched out) of papillae (Figs. 1 and 2) 2.2. Intense gingival pain 2.3. Bleeding gingiva with littl…
Investigation
- Thorough medical history, including nutrition and health habits
- Medical consult if immunosuppressive disease is suspected
- Dental history; pain (constant, intense onset)
- Extraoral examination; look for lymphadenopathy of the head and neck
Diagnosis
- Based on the clinical examination, a diagnosis of NUG is determined. Differential Diagnosis 1. Primary herpetic gingivostomatitis 2. Desquamative gingivitis 3. Agranulocytosis 4. Cyclic neutropenia 5. Leukemia 6. Ascorbic acid deficiency and gingivitis
Treatment
- Common Initial Treatments 1. Perform debridement under local anesthesia 2. Remove pseudomembrane using cotton pellet dipped in chlorhexidine 3. Provide patient with specific oral hygiene instructions to use a prescription antibacterial mouthwash: chlorhexidine 0.12% twice daily 4. Control pain with analgesics: ibuprofen 400-600 mg 3 times daily 5. Patient counselling …