
What does patchy lung mean? Pneumonia is an infection of the air sacs of the lungs that often produces a patchy or opaque appearance on X-rays. Pleural effusion is fluid in the layer between the lungs and chest wall, and it can cause a cloudy appearance on X-rays.
Full Answer
What does a patchy lung mean on a chest xray?
What does patchy lung mean? Pneumonia is an infection of the air sacs of the lungs that often produces a patchy or opaque appearance on X-rays. Pleural effusion is fluid in the layer between the lungs and chest wall, and it can cause a cloudy appearance on X-rays.
What is bronchopneumonia?
Bronchopneumonia. Bronchopneumonia is a type of pneumonia that mostly affects the bronchi and bronchioles. These are the system of tubes that bring air into your lungs. This type of pneumonia often spreads to other parts of the lungs if not treated effectively.
What is pneumonia and what causes it?
Pneumonia is a lung infection that’s caused by bacteria, viruses, or fungi. It ranges from mild to severe. Some cases of pneumonia occur as a complication of another infection, like influenza or COVID-19. It can affect the entirety of your lungs or only certain portions.
What is the difference between pneumonia and pneumonitis Quizlet?
Overview. Pneumonitis (noo-moe-NIE-tis) is a general term that refers to inflammation of lung tissue. Technically, pneumonia is a type of pneumonitis because the infection causes inflammation. Pneumonitis, however, is usually used by doctors to refer to noninfectious causes of lung inflammation.
What does COVID-19 pneumonia cause?
The pneumonia that COVID-19 causes tends to take hold in both lungs. Air sacs in the lungs fill with fluid, limiting their ability to take in oxygen and causing shortness of breath, cough and other symptoms.
Do all patients with COVID-19 get pneumonia?
Most people who get COVID-19 have mild or moderate symptoms like coughing, a fever, and shortness of breath. But some who catch the new coronavirus get severe pneumonia in both lungs. COVID-19 pneumonia is a serious illness that can be deadly.
Can COVID-19 give you pneunomia?
You're likely familiar with the common, mild symptoms of COVID-19 — including fever, dry cough and fatigue. But, in more severe cases, COVID-19 can also cause serious complications, including pneumonia.
Can COVID-19 pneumonia lead to acute respiratory distress syndrome (ARDS)?
As COVID-19 pneumonia progresses, more of the air sacs become filled with fluid leaking from the tiny blood vessels in the lungs. Eventually, shortness of breath sets in, and can lead to acute respiratory distress syndrome (ARDS), a form of lung failure.
What is the recovery time for the coronavirus disease?
Early research suggested that it could take 2 weeks for your body to get over a mild illness, or up to 6 weeks for severe or critical cases. Newer data show that recovery varies for different people, depending on things like your age and overall health.
Should I take antibiotics if I am sick with COVID-19?
No. Antibiotics do not work against viruses; they only work on bacterial infections. Antibiotics do not prevent or treat COVID-19, because COVID-19 is caused by a virus, not bacteria.
Can COVID-19 cause bilateral interstitial pneumonia?
Bilateral interstitial pneumonia is a serious infection that can inflame and scar your lungs. It's one of many types of interstitial lung diseases, which affect the tissue around the tiny air sacs in your lungs. You can get this type of pneumonia as a result of COVID-19.
What are some symptoms of the COVID-19 Omicron variant?
Omicron was first detected in November 2021 and has become the most dominant strain of COVID-19. Common symptoms are typically less severe than other variants and include cough, headache, fatigue, sore throat and a runny nose, according to the researchers.
Can COVID-19 affect the testicles?
"A significant percentage of men will experience testicular swelling or swelling of the epididymis after symptomatic COVID-19 infection," says Dr. Deibert. A recent review of male reproductive health estimates that "10% to 22% of men with acute COVID-19 infection develop orchitis or epididymo-orchitis.
What are some symptoms of COVID-19 Pneumonia?
COVID-19 Pneumonia Symptoms A fever, a dry cough, and shortness of breath are common early signs of COVID-19. You may also have: Fatigue. Chills.
What are some of the symptoms of Post-acute sequelae from COVID-19?
Those suffering from post-acute sequelae of COVID-19 frequently have difficulty concentrating and memory problems, sometimes called “brain fog.” This impairment is a common symptom in those with severe fatigue of any cause.
Which organ system is most often affected by COVID-19?
COVID-19 is a disease caused by SARS-CoV-2 that can trigger what doctors call a respiratory tract infection. It can affect your upper respiratory tract (sinuses, nose, and throat) or lower respiratory tract (windpipe and lungs).
What makes some people not get COVID-19?
Some studies have found a person's genetic profile, past exposure to other COVID-like viruses, allergies, and even drugs they take for other conditions may all provide some defense – even people who have not been vaccinated, don't use masks, or don't practice social distancing.
In what circumstances are ventilators needed for patients with COVID-19?
For the most serious COVID-19 cases in which patients are not getting enough oxygen, doctors may use ventilators to help a person breathe. Patients are sedated, and a tube inserted into their trachea is then connected to a machine that pumps oxygen into their lungs.
Does vitamin D affect COVID-19?
Vitamin D plays a role in the body's immune system and is known to enhance the function of immune cells. In this case, Vitamin D inhibits some of the inflammation that can make COVID-19 more severe.
Is shortness of breath an early symptom of Pneumonia due to COVID-19?
Breathlessness is caused by an infection in the lungs known as pneumonia. Not everyone with COVID-19 gets pneumonia, though. If you don’t have pneumonia, you probably won’t feel short of breath.
What happens when you have pneumonia?
Pneumonia and your lungs. Most pneumonia occurs when a breakdown in your body's natural defenses allows germs to invade and multiply within your lungs. To destroy the attacking organisms, white blood cells rapidly accumulate. Along with bacteria and fungi, they fill the air sacs within your lungs (alveoli).
How is pneumonia classified?
Pneumonia is classified according to the types of germs that cause it and where you got the infection.
Why is pneumonia so serious?
Hospital-acquired pneumonia can be serious because the bacteria causing it may be more resistant to antibiotics and because the people who get it are already sick. People who are on breathing machines (ventilators), often used in intensive care units, are at higher risk of this type of pneumonia.
What is a health care acquired pneumonia?
Health care-acquired pneumonia is a bacterial infection that occurs in people who live in long-term care facilities or who receive care in outpatient clinics , including kidney dialysis centers.
What is the most common cause of pneumonia?
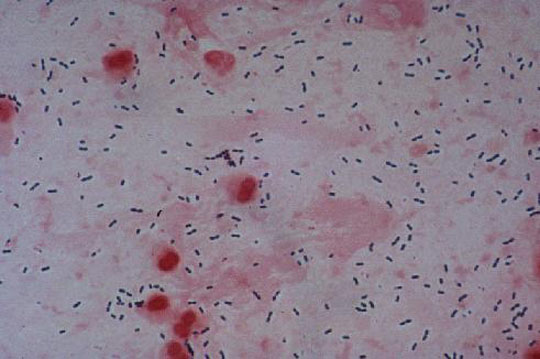
The most common cause of bacterial pneumonia in the U.S. is Streptococcus pneumoniae. This type of pneumonia can occur on its own or after you've had a cold or the flu. It may affect one part (lobe) of the lung, a condition called lobar pneumonia. Bacteria-like organisms.
How to prevent pneumonia?
Get vaccinated. Vaccines are available to prevent some types of pneumonia and the flu. Talk with your doctor about getting these shots. The vaccination guidelines have changed over time so make sure to review your vaccination status with your doctor even if you recall previously receiving a pneumonia vaccine.
What does it feel like to breathe and cough?
Chest pain when you breathe or cough. Confusion or changes in mental awareness (in adults age 65 and older) Cough, which may produce phlegm. Fatigue. Fever, sweating and shaking chills. Lower than normal body temperature (in adults older than age 65 and people with weak immune systems) Nausea, vomiting or diarrhea.
What percentage of pneumonia is caused by pleural effusion?
Pleural effusion: Pleural effusion or fluid around lungs is a common complication of pneumonia, occurs in 30-40% and a lot of time depends on what type of bacteria caus... Read More
Why does my lungs make a rattling sound?
Secretions: The rattling sound from lungs is generally due to vibrations produced by retained secretions (mucus/phlegm) in the airways (breathing tubes) in your l... Read More
Is it possible for an 8 month old to have pneumonia in both his lungs?
Yes.: Pneumonia can be localized affecting just a small portion of the lung or widely distributed. When widely distributed, this could be referred to as mul... Read More
Can kids' lungs heal after infection?
Most often no: Kids' lungs are quite resilient and a quite good at healing very well after infections. Even after severe infections. The vast majority of children re ... Read More
Are crackles in your lungs always pneumonia?
No: Not always. Other lung pathology can result in "crackles" when your doctor listens to your lungs.
What is the organization of pneumonia?
Organizing pneumonia is defined by the presence of buds composed of inflammatory cells, fibroblasts, and connective tissue within the lumen of distal air spaces. It may be secondary to various causes (such as infection or drug-induced reactions) or be cryptogenic.
What is secondary organizing pneumonia?
Secondary Organizing Pneumonia. When organizing pneumonia is secondary to another process, such as infection, drugs, malignancy, or connective tissue diseases, we refer to these cases as “secondary organizing pneumonia.”.
What is OP in pulmonary disease?
Initially described as the specific histopathologic pattern resulting from organization of an inflammatory exudate in the lumen of alveoli of unresolved pneumonia, OP is characterized by intraalveolar buds of granulation tissue with fibroblasts and myofibroblasts intermixed with loose connective matrix ( Figure 50-1 ). Similar lesions may be present within the lumen of the bronchioles—hence the formerly synonymous term bronchiolitis obliterans with organizing pneumonia (“BOOP”). The latter designation has been abandoned, however, because OP (rather than bronchiolitis) is clearly the major lesion, and furthermore, use of the older term was a potential source of confusion between this entity and bronchiolitis with airflow obstruction occurring, for example, after lung or hematopoietic stem cell transplantation. Although the condition is not strictly interstitial, COP is included in the American Thoracic Society/European Respiratory Society international consensus classification of the idiopathic interstitial pneumonias, because of its idiopathic nature and occasional similarities with interstitial pneumonias.
What is OP in medical terms?
Organizing pneumonia (OP) is a histopathologic diagnosis defined by a well-recognized pattern of changes underlying a characteristic clinical-pathologic entity. OP may occur in the absence of etiologic context, in which case it is known as cryptogenic organizing pneumonia (COP), or in association with a known causative agent or inflammatory disorder such as connective tissue disease, where it is called secondary organizing pneumonia.
What is diffuse pulmonary infiltrate?
The disease is in the form of diffuse or focal pulmonary infiltrates, migratory alveolar opacities, or dense nodules with or without air bronchograms. Organizing pneumonia induced by drugs expresses itself in a manner similar to organizing pneumonia from other causes or that occurs idiopathically.
Can organizing pneumonia relapse?
Organizing pneumonia responds well to drug therapy withdrawal and corticosteroid therapy, but the condition may relapse if corticosteroids are tapered too early or too swiftly, or if the causal drug is inappropriately continued. View chapter Purchase book. Read full chapter.
What causes multifocal pneumonia?
Multifocal pneumonia can also be caused by a bacteria like streptococcus pneumoniae or legionella pneumophila, or a fungus like pneumocystis pneumonia, coccidioidomycosis, or cryptococcus, Dr. Casciari says. "Having multifocal pneumonia doesn't automatically signify what's causing the pneumonia," he says. "We still have to investigate."
How is multifocal pneumonia treated?
Doctors like to try to catch pneumonia early so that they can treat it appropriately and catch it before it progresses too far, Dr. Gates says. But the actual treatment depends on what's causing the pneumonia in the first place. "You've got to find the cause," Dr. Casciari says.
How long does it take to recover from pneumonia?
A person's overall health matters with recovery from multifocal pneumonia. "Most healthy people with minimal underlying medical conditions usually recover from pneumonia with no issue over the course of several days," Dr. Sood says. "Patients who have underlying medical conditions still may have good recovery but it may take longer. In very severe cases, pneumonia can cause death."
What is the name of the infection that causes a person to cough and have a fever?
In the most general of terms, pneumonia is an infection in the lungs caused by inflammation of the air sacs, known technically as alveoli. Those alveoli fill up with fluid or pus, which leads to symptoms like coughing, fever, and chills.
Why is pneumonia considered a type of pneumonitis?
Technically, pneumonia is a type of pneumonitis because the infection causes inflammation. Pneumonitis, however, is usually used by doctors to refer to noninfectious causes of lung inflammation. Common causes of pneumonitis include airborne irritants at your job or from your hobbies.
What causes pneumonitis?
Pneumonitis causes may include: 1 Drugs. A variety of drugs can cause pneumonitis, including some antibiotics, several types of chemotherapy drugs and medications that keep your heartbeat regular. An overdose of aspirin can cause pneumonitis. 2 Molds and bacteria. Repeated exposure to some molds and bacteria can cause the lungs to become inflamed. Specific varieties of mold-related pneumonitis have received nicknames, such as "farmer's lung" or "hot tub lung." 3 Birds. Exposure to feathers or bird excrement is a common cause of pneumonitis. 4 Radiation treatments. Some people who undergo radiation therapy to the chest, such as for breast or lung cancer, may develop pneumonitis. Pneumonitis also can occur after whole-body radiation therapy, which is needed to prepare a person for a bone marrow transplant.
What causes air sacs to become inflamed?
Pneumonitis occurs when an irritating substance causes the tiny air sacs (alveoli) in your lungs to become inflamed. This inflammation makes it difficult for oxygen to pass through the alveoli into the bloodstream.
Why do hot tubs cause pneumonitis?
Hot tubs and humidifiers. Moldy conditions in hot tubs can trigger pneumonitis because the bubbling action makes a mist that can be inhaled. Home humidifiers are another common reservoir for mold.
What causes pneumonitis in farm workers?
Farming. Many types of farming operations expose workers to aerosolized mists and pesticides. Inhaling airborne particles from moldy hay is one of the most common causes of occupational pneumonitis. Mold particles also can be inhaled during harvests of grain and hay. Bird handling.
What are the symptoms of chronic pneumonitis?
Signs and symptoms of chronic pneumonitis include: Shortness of breath. Cough.
What is the most common symptom of pneumonitis?
Difficulty breathing — often accompanied by a dry (nonproductive) cough — is the most common symptom of pneumonitis. Specialized tests are necessary to make a diagnosis. Treatment focuses on avoiding irritants and reducing inflammation.
What is OP in a lung biopsy?
Organizing pneumonia (OP) is a histologic term characterized by patchy filling of alveoli and bronchioles by loose plugs of connective tissue. OP may be an incidental finding in lung biopsy specimens or may be found nearby areas of lung involved by other diseases. On other occasions, OP may be the primary cause for pulmonary dysfunction and/or ...
What is the definitive diagnosis of OP?
The definitive diagnosis of OP requires histology. Open lung biopsy or video assisted thoracoscopy is usually required to obtain specimens large enough for the diagnosis to be made. In some cases, transbronchial biopsy specimens may be adequate for the diagnosis.
Is OP a pulmonary disease?
On other occasions, OP may be the primary cause for pulmonary dysfunction and/or pulmonary symptoms. OP can be either idiopathic (cryptogenic organizing pneumonia, COP) or secondary to underlying disease (secondary organizing pneumonia, SOP).

Overview
Symptoms
- The signs and symptoms of pneumonia vary from mild to severe, depending on factors such as the type of germ causing the infection, and your age and overall health. Mild signs and symptoms often are similar to those of a cold or flu, but they last longer. Signs and symptoms of pneumonia may include: 1. Chest pain when you breathe or cough 2. Confusion or changes in mental aware…
Causes
- Many germs can cause pneumonia. The most common are bacteria and viruses in the air we breathe. Your body usually prevents these germs from infecting your lungs. But sometimes these germs can overpower your immune system, even if your health is generally good. Pneumonia is classified according to the types of germs that cause it and where you got the infection.
Risk Factors
- Pneumonia can affect anyone. But the two age groups at highest risk are: 1. Children who are 2 years old or younger 2. People who are age 65 or older Other risk factors include: 1. Being hospitalized.You're at greater risk of pneumonia if you're in a hospital intensive care unit, especially if you're on a machine that helps you breathe (a ventilator). 2. Chronic disease. You'r…
Complications
- Even with treatment, some people with pneumonia, especially those in high-risk groups, may experience complications, including: 1. Bacteria in the bloodstream (bacteremia).Bacteria that enter the bloodstream from your lungs can spread the infection to other organs, potentially causing organ failure. 2. Difficulty breathing.If your pneumonia is severe or you have chronic und…
Prevention
- To help prevent pneumonia: 1. Get vaccinated.Vaccines are available to prevent some types of pneumonia and the flu. Talk with your doctor about getting these shots. The vaccination guidelines have changed over time so make sure to review your vaccination status with your doctor even if you recall previously receiving a pneumonia vaccine. 2. Make sure children get va…