Where is a PCOM aneurysm?
Posterior communicating artery (PCOM) aneurysms is considered a internal carotid artery aneurysm. Intracranial aneurysms arising from the posterior wall of the supraclinoid carotid artery are extremely common lesions.
How is PCOM aneurysm treated?
Treatment options of PCOM aneurysm include surgical clipping and endovascular techniques; surgical treatment is preferable in large aneurysm especially when it is causing mass effect on the oculomotor nerve, aneurysms with unfavorable fundus, and those associated with fetal PCOM artery origin [3, 4].
What is PCOM in brain?
The posterior communicating artery (PCOM) is a part of a group of arteries in the brain known as the circle of Willis. The artery connects the internal carotid and the posterior cerebral arteries. Its role is to provide blood supply to the brain.
How is PCOM aneurysm diagnosed?
Expert interpretation of modern noninvasive neuroimaging such as computed tomographic angiography (CTA) and magnetic resonance angiography (MRA), should detect nearly all aneurysms responsible for an isolated third nerve palsy.
What causes a posterior communicating artery aneurysm?
Suddenly, increased intracranial aneurysm blood flow and pressure during posterior circulation angiography continuous injection of contrast medium with high-pressure syringe might be another main cause of ruptured posterior communicating artery aneurysm hemorrhage.
What does PCOM mean in medical terms?
polycystic ovarian morphologyWith the advent of ultrasonography, follicle excess has become the main aspect of polycystic ovarian morphology (PCOM).
What neurological signs would you expect from a posterior communicating artery aneurysm?
While most unruptured PCOM aneurysms are asymptomatic, when symptoms do occur, clinical manifestations typically include severe headache (HA), visual acuity loss, and cranial nerve deficit.
What are the symptoms of posterior cerebral stroke?
Patients with a PCA stroke may present with only a headache and mild visual changes such as vision loss, diplopia, inability to see half of the view, or difficulty reading perceiving colors, or recognizing familiar faces. Mild symptoms in the setting of a PCA stroke may delay a patient from getting medical treatment.
How is aneurysm coiling done?
During endovascular coiling, a catheter is passed through the groin up into the artery containing the aneurysm. Platinum coils are then released. The coils induce clotting (embolization) of the aneurysm and, in this way, prevent blood from getting into it.
How do you stop an aneurysm from growing?
To prevent an aortic aneurysm or keep an aortic aneurysm from worsening, do the following:Don't smoke or use tobacco products. Quit smoking or chewing tobacco and avoid secondhand smoke. ... Eat a healthy diet. ... Keep your blood pressure and cholesterol under control. ... Get regular exercise.
How big does a brain aneurysm have to be for surgery?
the size of the aneurysm – aneurysms larger than 7mm often require surgical treatment. the location of the aneurysm – brain aneurysms located on larger blood vessels have a higher risk of rupture.
How serious is a 5 mm aneurysm?
Objective. Small unruptured aneurysms (<5 mm) are known for their very low risk of rupture, and are recommended to be treated conservatively. However, we encounter many patients with small ruptured aneurysms in the clinical practice.
Does everyone have a posterior communicating artery?
About 20% of adults retain PCA origin from the posterior communicating artery, and in turn, the internal carotid arteries.
What neurological signs would you expect from a posterior communicating artery aneurysm?
While most unruptured PCOM aneurysms are asymptomatic, when symptoms do occur, clinical manifestations typically include severe headache (HA), visual acuity loss, and cranial nerve deficit.
What are the symptoms of posterior cerebral stroke?
Patients with a PCA stroke may present with only a headache and mild visual changes such as vision loss, diplopia, inability to see half of the view, or difficulty reading perceiving colors, or recognizing familiar faces. Mild symptoms in the setting of a PCA stroke may delay a patient from getting medical treatment.
How is aneurysm coiling done?
During endovascular coiling, a catheter is passed through the groin up into the artery containing the aneurysm. Platinum coils are then released. The coils induce clotting (embolization) of the aneurysm and, in this way, prevent blood from getting into it.
Where does p-comm occur?
1. May occur at either end of p-comm; that is at the junction with the PCA, or more commonly at the junction with internal carotid artery (typically points laterally, posteriorly, and inferiorly). May impinge on the third cranial nerve in either case and cause oculomotor nerve palsy ( ptosis, mydriasis, “down and out” deviation) that, is not pupil sparing in 99% of cases.
What is the junction of the posterior communicating artery?
Posterior communicating artery aneurysm, may occur at either end of the posterior communicating artery; that is at the junction with the posterior cerebral artery , or more commonly at the junction with the carotid (typically points laterally, posteriorly, and inferiorly). May impinge on the third nerve in either case and cause third nerve palsy ( ptosis, mydriasis, “down and out” deviation) that is not pupil sparing in 99% of cases. Surgical clipping may be more advantageous than endovascular coiling to treat oculomotor nerve palsies caused by p-comm aneurysms 1) 2) .
Where is the PCOM located?
The PCOM is located in the back of the head at the back end of the circle of Willis. It is located on the left and right sides of the head and is relatively short. The posterior cerebral arteries branch off from the basilar artery. The left and right PCAs form the longest sections of the circle of Willis.
What is the location of an aneurysm?
Aneurysm. The posterior communicating artery is a potential location of aneurysms. An aneurysm is a bulging area in an artery. Although aneurysms in the circle of Willis most commonly occur in the anterior communicating artery, those in the posterior circulation account for 15% to 20% of all intracranial aneurysms. 1.
What is the role of the posterior communicating artery?
The artery connects the internal carotid and the posterior cerebral arteries. Its role is to provide blood supply to the brain. The posterior communicating artery is a location where aneurysms can potentially occur.
Which aneurysm is more likely to rupture?
PCOM aneurysms are more likely to rupture than those that occur elsewhere in the brain. 2 Aneurysms are classified by size and shape, with saccular aneurysms being the most common. Saccular aneurysms are those that bulge out from the artery like a berry attached by a stalk.
What is the term for a blockage of blood flow in the brain?
Stroke. A stroke occurs when there is an interruption of blood flow in an artery. This blockage keeps blood from reaching its destination in the brain, resulting in a loss of function in the affected region.
Can an aneurysm cause vision loss?
Symptoms do not always occur with aneurysms, especially if they haven’t ruptured. When they do occur, symptoms include headaches, stroke symptoms, seizures, vision changes, and loss of consciousness. Brain aneurysms generally develop without a known cause, but genetics may play a role. 3
What is the morbidity of a PComA aneurysm?
Relative to microsurgical treatment of aneurysms in other locations, neurologic morbidity from PComA aneurysms is the lowest. Wirth and co-workers report an operative morbidity of 5% compared to that associated with other anterior circulation aneurysms: MCA of 8%, ICA termination of 12%, and anterior communicating artery of 16%. 9,27
How to treat a PCA aneurysm?
The first step in treating PCoA aneurysms is to determine the nature of the vessel. In the case of a fetal PCoA, protrusion of a coil mass in the lumen may cause an infarct in the distal territory of the posterior cerebral artery (PCA). In a nonfetal configuration, treatment can be more aggressive with balloon- or stent-assisted coiling. In wide-necked PCoA aneurysms, stent-assisted coiling is an effective technique. The proximal location of the artery makes it easier to navigate and to use the stent to push a herniated coil back into the aneurysm or to pin it against the ICA. To stabilize the microcatheter during coiling, the catheter is advanced more distal to the stent before the stent is deployed. This strategy ‘jails’ the catheter.
What is the purpose of the sylvian fissure?
The arachnoid over the optic nerve, ICA, and medial aspect of the sylvian fissure is first dissected to allow for a wide surgical exposure. Opening the sylvian fissure allows the distal carotid artery at the bifurcation to be visualized. Further dissection along the proximal and distal carotid artery is essential to establish vessel control before further clipping the aneurysm. The plane between the optic nerve and the carotid artery is carefully dissected to establish the inferior and superior aspects of the aneurysm neck. The surgical clip is placed across the neck; a number of clip configurations can be utilized to obliterate the lesion while maintaining the patency of the carotid and posterior communicating artery vessels ( Fig. 67-14 ). After clipping, further dissection is imperative to ensure that the anterior choroidal artery (which may be duplicated), third nerve, thalamoperforators, and PCoA are not occluded or kinked by the blades of the clip. Occlusion of the anterior choroidal artery or perforators is poorly tolerated and leads to infarction. In contrast, occlusion of the PCoA segment may be unavoidable and is tolerated if there is collateral flow to the perforators from the posterior circulation; however, in most cases, the PCoA can be preserved.
What is the ACH in an aneurysm?
The posterior communicating artery (PCOM) and anterior choroidal artery (ACH) branch laterally from the communicating segment of the ICA, prior to its bifurcation into M1 and A1. They are intimately associated with each other. The location of the ACH is often immediately distal and adjacent to the takeoff of the PCOM and needs to be identified and protected with every PCOM aneurysm that is surgically explored and ligated. Although the most common site of origin of the ACH is from the ICA itself, normal variants of branching include origin from the PCOM, the proximal M1, or the ICA bifurcation itself. The course of the proximal ACH is posteromedial behind the ICA and is associated with the medial aspect of the uncus. The second anatomic consideration of the PCOM is the presence of a fetal PCOM, whereby the P1 is functionally absent and as such the fetal PCOM supplies not only the thalamoperforators along its course but also the ipsilateral P2–P4 segments. By losing the redundancy of the circle of Willis with this anatomic variant, the importance of preservation of a fetal PCOM becomes the highest priority.
What is a PCOMA?
Posterior communicating artery aneurysms (PComA) at the junction of the posterior communicating and internal carotid arteries are neurological emergencies that may present as isolated painful third nerve palsies. The nerve fibers that travel to the iris sphincter muscle run in the medial portion of the third nerve, ...
What is the diameter of the PCOA?
The PCoA arises 9.6 mm distal to the ophthalmic artery and 9.7 mm proximal to the carotid bifurcation and measures on average 1.4 mm in diameter and 12 mm in length. Perforators of the PCoA, 7.8 in number on average, travel superiorly and in decreasing order of frequency to the floor of the third ventricle, the posterior perforated substance, interpeduncular fossa, optic tract, pituitary stalk, and optic chiasm and reach the thalamus, hypothalamus, subthalamic nucleus, and internal capsule. They are also referred to as anterior thalamoperforators. The largest perforator adjacent to the mammillary body is referred to as the “premamillary” or “anterior thalamoperforating” artery ( Gibo et al., 1981 ).
Where does the PCOA originate?
The posterior communicating artery (PCoA) typically originates from the posterior or posterolateral surface of the carotid artery as it bends upward toward the bifurcation (Fig. 67-12 ). Posterior communicating aneurysms, however, can be divided into the following two subcategories: (1) aneurysms that project laterally and below the tentorial incisura and cause oculomotor nerve compression where the nerve enters the dura at the tentorial edge and (2) aneurysms that project laterally above the tentorium that can manifest as temporal lobe hematoma after they rupture. 46 Patients with ruptured PCoA aneurysms present with SAH and often ipsilateral third nerve paresis that may involve the pupil. As such aneurysms enlarge they may compress against the tentorial edge and reside partially above and below the tentorium. In these cases, great care is utilized in the microdissection of the neck and the dome of the aneurysm. At times, sharp dissection of the tentorium is needed to fully visualize the base of the aneurysm. During this dissection, one must take care to be aware of the fourth nerve, which runs in the fold of the tentorium.
Acronyms & Abbreviations
Get instant explanation for any acronym or abbreviation that hits you anywhere on the web!
A Member Of The STANDS4 Network
Get instant explanation for any acronym or abbreviation that hits you anywhere on the web!
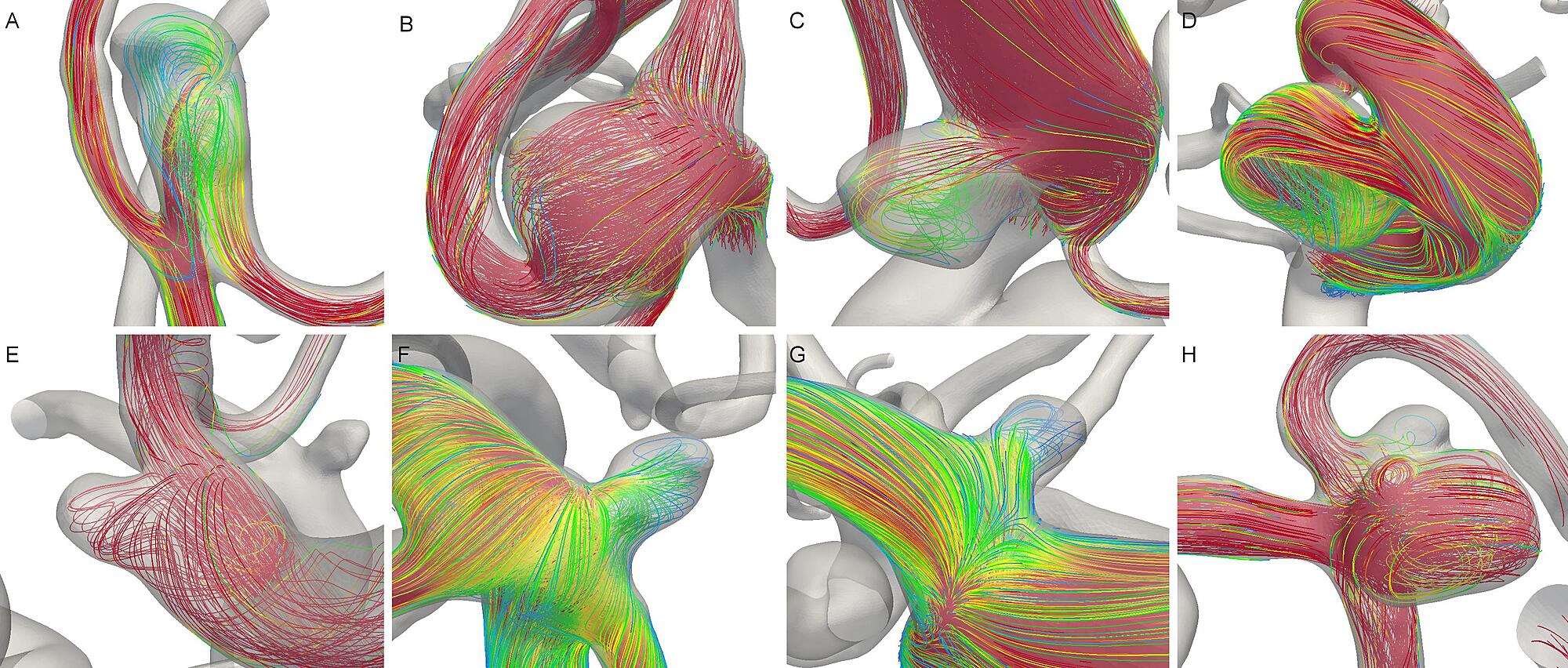
How to clip a PCOM aneurysm?
Clipping of PCOM aneurysms is typically done with a slightly curved clip, with the proximal blade being placed proximally along the PCOM and at the junction between the vessel and the aneurysm , visualizing this as much as possible during this maneuver, as well as advancing the distal blade between under direct visualization between the PCOM and the ACH. The slight curve of the clip helps eliminate a “dog-ear” adjacent to the ICA. A final rotation maneuver dropping the surgeon's hand toward the globe minimizes the likelihood that the distal blades will pinch the distal PCOM and will also make the clip more parallel to the ICA. The ACH and the distal blades should be inspected immediately. Exploration of the ventral surface of the ICA to ensure a remnant is not left that is obscured by the ICA is of paramount importance. ICGA will identify the distal PCOM and ACH, although intraoperative angiograms typically produce high-yield results in PCOM cases, particularly for fetal PCOM aneurysms.
What is the morbidity of a PComA aneurysm?
Relative to microsurgical treatment of aneurysms in other locations, neurologic morbidity from PComA aneurysms is the lowest. Wirth and co-workers report an operative morbidity of 5% compared to that associated with other anterior circulation aneurysms: MCA of 8%, ICA termination of 12%, and anterior communicating artery of 16%. 9,27
What is the origin of a PCOA?
Posterior communicating aneurysms most commonly incorporate the origin of the PCoA in their neck. Side wall aneurysms of the communicating segment of the ICA adjacent to the PCoA or aneurysms arising solely off the PCoA (so-called “true” PCoA aneurysms) are less common. The “true” PCoA aneurysms make up 13% of PCoA aneurysms in one series and were associated with larger posterior communicating arteries relative to the ipsilateral P1 segment and were smaller in size. They were just as likely to present with aSAH compared to all PCoA aneurysms ( He et al., 2010 ). A systematic review and meta-analysis published by the same group found that “true” PCoA aneurysms represented 6.8% of all PCoA aneurysms. Approximately 90% of included patients had a ruptured “true” PCoA aneurysm and there was no association of rupture status with patient age or saccular versus fusiform shape ( He, Gandhi, Quinn, Karimi, & Prestigiacomo, 2011 ).
What is the ACH in an aneurysm?
The posterior communicating artery (PCOM) and anterior choroidal artery (ACH) branch laterally from the communicating segment of the ICA, prior to its bifurcation into M1 and A1. They are intimately associated with each other. The location of the ACH is often immediately distal and adjacent to the takeoff of the PCOM and needs to be identified and protected with every PCOM aneurysm that is surgically explored and ligated. Although the most common site of origin of the ACH is from the ICA itself, normal variants of branching include origin from the PCOM, the proximal M1, or the ICA bifurcation itself. The course of the proximal ACH is posteromedial behind the ICA and is associated with the medial aspect of the uncus. The second anatomic consideration of the PCOM is the presence of a fetal PCOM, whereby the P1 is functionally absent and as such the fetal PCOM supplies not only the thalamoperforators along its course but also the ipsilateral P2–P4 segments. By losing the redundancy of the circle of Willis with this anatomic variant, the importance of preservation of a fetal PCOM becomes the highest priority.
What is the most common intracranial aneurysm?
Posterior communicating artery aneurysms are the most common of all intracranial aneurysms. Twenty percent to 61% of patients present with an ipsilateral third nerve palsy, which dilates the pupil. It is essential to recognize this disorder promptly because of the risk of subsequent, devastating subarachnoid hemorrhage. Importantly, the abnormal pupil is almost always accompanied by ptosis and ophthalmoplegia (i.e., full third nerve palsy, see Fig. 19-5 ): In reports of 332 aneurysms that give details of the third nerve paresis, 71% had dilated pupil and complete ophthalmoplegia, 25% had dilated pupil and partial ophthalmoplegia, 4% had sparing of the pupil with partial ophthalmoplegia, and only 1 patient had isolated involvement of the pupil. 43–51
What is PCOA in surgery?
Posterior communicating artery ( PCoA) aneurysms are the second most common type of aneurysms after those involving the ACoAs. They typically manifest with third cranial nerve palsy. Surgical clipping offers immediate relief compared to the relatively prolonged process involved with thrombosis and subsequent retraction of the aneurysm after coiling. Nonetheless, endovascular therapy has been used to treat this group of aneurysms.
How to treat a PCA aneurysm?
The first step in treating PCoA aneurysms is to determine the nature of the vessel. In the case of a fetal PCoA, protrusion of a coil mass in the lumen may cause an infarct in the distal territory of the posterior cerebral artery (PCA). In a nonfetal configuration, treatment can be more aggressive with balloon- or stent-assisted coiling. In wide-necked PCoA aneurysms, stent-assisted coiling is an effective technique. The proximal location of the artery makes it easier to navigate and to use the stent to push a herniated coil back into the aneurysm or to pin it against the ICA. To stabilize the microcatheter during coiling, the catheter is advanced more distal to the stent before the stent is deployed. This strategy ‘jails’ the catheter.
