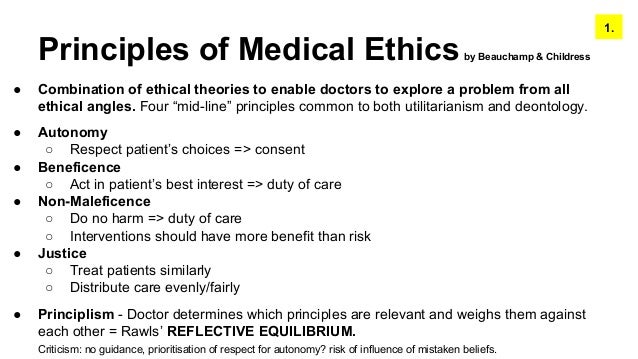
Principlism. Principlism is a commonly used ethical approach in healthcare and biomedical sciences. It emphasises four key ethical principles of autonomy, beneficence, non-maleficence, and justice, which are shared by most ethical theories, and blends these with virtues and practical wisdom.
What are the principles of principlism in healthcare?
Using this principle, the healthcare providers have a responsibility to consider the pain experienced by the patients in their decisions. The theory replaces the moral theory and rules with principles that are one of the greatest weaknesses of the principlism theory.
What is principlism in ethics?
principlism(Noun) A system of ethics based on the four moral principles of autonomy, beneficence, nonmaleficence, and justice. Freebase(5.00 / 4 votes)Rate this definition: Principlism is a system of ethics based on the four moral principles of: 1. Autonomy--free-will or agency, 2. Beneficence--to do good, 3.
What are the principles of Health and social care?
Keeping to the principles of health and social, the worker must keep all information relevant to the service user private, any information that may violated users’ privacy will need the consent of the service user. Care worker must have empathy and make ensured that decisions about patients are informed choice of the user.
What are the principles of support in nursing?
1.1 The principles of support are applied to ensure that individuals are cared for in care setting. The responsibility and duty of health and social practice is to provide support for the service users. In health care setting, the providers of health and social care must ensure that service users wellbeing and right are not violated.

What is virtue ethics in health and social care?
By contrast, virtue ethics sees good practice as practice that results from the virtuous moral character of the doctor. As a distinctive approach to medical ethics, virtue ethics investigates how the doctor's good moral character enables them to promote the good for the patient.
What are the 4 principles of principlism?
Principlism, the bioethical theory championed by Tom Beauchamp and James Childress, is centered on the four moral principles of beneficence, non-maleficence, respect for autonomy, and justice.
What is an example of principlism in health and social care?
Moral Conflicts and Their Resolution. In principlism, moral problems arise because of conflicts of prima facie duties. Classic examples are problems of paternalism where physicians seek to provide health benefits by overriding a patient's autonomous choice.
What is meant by principlism?
Principlism is a normative ethical framework designed for decision making in health care. It is a common-morality approach relying on four mid-level principles: respect for autonomy, nonmaleficence, beneficence, and justice.
What are the 4 principles of healthcare?
Moreover, these four principles, plus attention to their scope of application, encompass most of the moral issues that arise in health care. The four prima facie principles are respect for autonomy, beneficence, non-maleficence, and justice.
Which of the following most accurately describes principlism?
Which of the following most accurately describes principlism? Principlism is the view that a case can be analyzed using a set of principles and the most important principle can vary depending on the case. Since ethical analysis must consider the context of each case, one principle may not always take priority.
What are the 4 ethical principles in health and social care?
Beneficence, nonmaleficence, autonomy, and justice constitute the 4 principles of ethics.
How does the principle of ethical principlism apply to nursing practices?
Ethical Principles in Nursing Autonomy means that the patients are able to make independent decisions. This means that nurses should be sure patients have all of the needed information that is required to make a decision about their medical care and are educated. The nurses do not influence the patient's choice.
What is beneficence in principlism?
Beneficence. This principle describes an obligation to act for the benefit of others. Acting in this way might involve preventing or removing harm, or it might involve the active promotion of some good (e.g., health). The aim of beneficent action is to produce the "best" one can out of a range of possibilities.
What are the 5 P's in ethics?
Norman and I shaped our thinking around what we called The Five P's of Ethical Power: purpose, pride, patience, persistence and perspective.
Who developed the principlism theory?
Principlism, the bioethical theory championed by Tom Beauchamp and James Childress, is centered on the four moral principles of beneficence, non-maleficence, respect for autonomy, and justice.
What is autonomy in health and social care?
In medical practice, autonomy is usually expressed as the right of competent adults to make informed decisions about their own medical care. The principle underlies the requirement to seek the consent or informed agreement of the patient before any investigation or treatment takes place.
What are the 4 ethical dimensions?
This framework approaches ethical issues in the context of four moral principles: respect for autonomy, beneficence, nonmaleficence, and justice (see table 1). This framework has been influential because the values it espouses seem to align with our moral norms.
Who came up with the 4 ethical principles?
Beauchamp and ChildressThe four standard principles proposed by Beauchamp and Childress [2] were used in the new measure, as well as two other principles; confidentiality and truth-telling, which are within the Beauchamp and Childress [2] framework embedded within the principle of autonomy.
What are the four 4 domains of bioethics?
The four main moral commitments are respect for autonomy, beneficence, nonmaleficence, and justice. Using these four principles and thinking about what the physicians' specific concern is for their scope of practice can help physicians make moral decisions.
What is beneficence in principlism?
Beneficence. This principle describes an obligation to act for the benefit of others. Acting in this way might involve preventing or removing harm, or it might involve the active promotion of some good (e.g., health). The aim of beneficent action is to produce the "best" one can out of a range of possibilities.
What is the purpose of the principle of support?
1 (a) Explanation of the principles of support are applied to ensure that individuals are cared for in health and social care practice
Why is the organizing principle important?
Employees need to follow to ensure the smooth running of the system , the organizing principle of the organization is important. To reduce misunderstanding and misinterpretation , it is necessary to organizational policies are clear and blunt.
Why are care workers contradictory?
Care workers to maintain the organizational policies and wellbeing of clients all the time, but in some situations the rules they are not able to implement it to the essential. Moral dilemmas are built these kinds of situations. Sometimes conflicts between care workers and service user’s views, beliefs and cultures may arise. Health and social care services could be hampered by the conflict and may be affected by the quality of health and social care.
What is organizational policy?
Organization policy – law, practice policies, rules, regulations, and codes are important present. Providing guidelines it says that Policy and law, institutions will have to practice. Without reference to the law and the law of the organization, legal, health and social care center for which it is really difficult to formulate policy. Any violation of the rights of the individual, organizational policy, Law and practice in an organized, competent and ethical work environment, service users and staff will be made. The organizing principle of the organization without any serious conflict, it is very easy to use. It is the employee to work in accordance with the law to respect the law and acclimate employee’s helps. An employee fines or even anyone who breaks the law and regulations, will not leave him in his work. An employee is an employee of any laws and regulations to be confused about, then you can ask his superiors, and they will help him to get out of the dilemma. Both employers and employees and the respective authority is obliged to obey and follow the rules and regulation and correct them or even anyone to take immediate steps to punish those who break the law.
What are the services and support people are entitled to in Wales?
Today, in Wales, services and support people are entitled to include home care help things like cleaning and shopping, insufficient tools and adaptations to your house, day centre’s to give you the least care at their best, day care for your children if either you or them are not able to look after them .
What is the Maslow hierarchy of needs?
Service users, physical, spiritual, social, emotional, and mental fitness to promote healthy lifestyles and to achieve a high level, the theory helps to develop a plan. Maslow hierarchy of needs state that theory of health and social care. his theory, human needs are classified into different levels, and basic needs are put first. According to his theory, the bottom level is not met, a man to go to the next level. Physiological or physical demands of this theory are considered to be the most basic needs. Safety and security, love and belonging, self-esteem and self actualization is the next level. While planning for the care and services to a service user of this theory is applied. Other well-known theory of human growth and development, Help and Care is needed in a variety of different levels. Age, growth and development, the care and services is changing.
Is socialization a form of support?
Person’s health is another type of support which is related to the Social support and co-ordination. The effect of socialization works is a main and sometimes slighted cause for the success of psychotherapy and it is the most the most integral matter. On certain just having the feelings that there is someone to communicate andrelyon can help people overcomes their situation and it is more than effective than any other treatment. Having a greater social communication system, whether family, friends and neighbors make an immense of effective situation.
Which of the four principles of health care ethics is the most commonly prioritized?
Of the four principles of health care ethics, non-maleficence is the one that is generally the one most commonly prioritized.
What are the four principles of ethics in healthcare?
These principles are autonomy, beneficence, non-maleficence, and justice. Each of these principles has a unique objective, but the four come together to empower you as a health care ...
What is beneficence in nursing?
At its core, beneficence is an essential principle of health care ethics and ethical selfishness. The principle encourages health care workers to consciously invest the time ...
Why is autonomy important in healthcare?
The practice of autonomy prevents health care professionals from potentially coercing or persuading the patient to take a specific action or treatment plan that might not be in their best interest.
What is the act of kindness or mercy?
Beneficence is the act of showing kindness or mercy. The actions of any health care provider should always bring positivity. Beneficence should not be confused with the closely related ethical principle of non-maleficence, which states that one should do no harm to patients.
Why is it important for a health care professional to take control of a patient?
So it’s a health care professional’s responsibility to help empower each patient to take control of their own health care.
Why do people choose health care?
Most people who choose health care as a profession do so because they want to help other people, and part of the profession is seeking out every way that you can help make a patient’s treatment experience a little bit better, safer, and more effective. Even the smallest positive change can have a big impact on a patient’s wellbeing.
What is the problem with Principlism?
Finally, the greatest problem with principlism, especially regarding the purposes of this chapter, is that it fails to include appropriate provisions for individuals who are unable to exercise independent autonomy and therefore is inadequate for anyone interested in a bioethic that considers individuals who are disabled, especially if their disability affects their cognition. “People or potential people with intellectual disability are most likely to be rendered, even on biological determination alone, profoundly irrelevant or disqualified within bioethical conversations because they are deemed incapable of being rational, competent, independent beings” ( Clapton, 2002 ). Clearly, this is inadequate, yet it has its roots in Beauchamp and Childress: “Personal autonomy, [which] is, at a minimum, self-rule that is free from both controlling interference by others and from limitations. The autonomous individual acts freely in accordance with a self-chosen plan, analogous to the way an independent government manages its territories and sets its policies” ( Beauchamp and Childress, 2001 ).
What is the Principlist approach to ethics?
The principlist approaches to the ethics of carebots identified by Vandemeulebroucke and colleagues are viewed by the authors as “practical translations of the deontological approach” (20)—these analyses take essentially deontological arguments about carebots and provide practical suggestions to address the stated concerns. Principlism is an established approach in biomedical ethics, based on a set of values that medical professionals can refer to in the case of confusion or conflict, which include (1) respect for autonomy, (2) beneficence, (3) nonmaleficence (and in this context safety), and (4) justice (Beauchamp & Childress, 2009 ). The principlist approach may be seen as more optimistic, recognizing the potential benefits of carebots and suggesting practical solutions to the legitimate ethical concerns.
What is the dominant paradigm in bioethics?
The rise to preeminence of principlism as the dominant paradigm is due in large part to its clarity and ease of use in communication (to other professionals, students, and the general public). In addition, its deductive nature suggests its similarity to empiric sciences, and therefore it is often seen as “more true” than inductive or “softer” sciences. Most important, it is often tremendously helpful in confused situations with many conflicting actors with divergent views of “what is important” and several important outcomes in the balance. The ethical paradigm in medicine that immediately precedes principlism is now often referred to as benevolent paternalism, a term usually with negative connotations. Principlism has supplanted paternalism and now is the primary method that is currently taught at professional schools for health care clinicians. The most influential text used for teaching the system, Principles of Biomedical Ethics by Beauchamp and Childress (2001), has certainly evolved with time and in response to critics. However, the central claims remain the same: “The common morality contains a set of moral norms that includes principles that are basic for biomedical ethics. Most classical ethical theories include these principles in some form, and traditional medical codes presuppose at least some of them. The four clusters [of moral principles] are (1) respect for autonomy (a norm of respecting the decision-making capacities of autonomous persons), (2) non-malfeasance (a norm of avoiding the causation of harm), (3) beneficence (a group of norms for providing benefits and balancing benefits against risks and costs), and (4) justice (a group of norms for distributing benefits, risks, and costs fairly).”
What is the difference between beneficence and care based ethics?
Whereas beneficence focuses on the physician–patient relationship, care-based ethics incorporates the complex web of relationships in which the patient is embedded and considers the perspectives of all those who truly care for the patient. Indeed, the connection among family members (broadly defined) ordinarily supersedes the connection between patient and physician and, furthermore, the burden and gratification of caring for the patient fall most heavily on the family. Thus, from the perspective of care-based ethics, the family has a much stronger interest and responsibility for decisions about the patient’s care than typically understood in more traditional ethics – such as either a principlism or beneficence-focused perspective.
What is principled ethics?
The principled ethics analysis begins with an ethical principle such as autonomy or beneficence and then applies it to the case. This principlism is theoretical and can be rather abstract. For example, Tom Beauchamp and James Childress, in their Bioethics in 2001 emphasize the essential middle level ethical principles of (1) autonomy, the patient's independence in deciding what is best; (2) nonmaleficence, avoiding harm to the patient; (3) beneficence, doing good for the patient; (4) justice, fairness to the patient; and (5) professional-patient relationship.
What are the principles of principled ethics?
The principled ethics analysis begins with an ethical principle such as autonomy or beneficence and then applies it to the case. This principlism is theoretical and can be rather abstract. For example, Tom Beauchamp and James Childress, in their Bioethics in 2001 emphasize the essential middle level ethical principles of (1) autonomy, the patient's independence in deciding what is best; (2) nonmaleficence, avoiding harm to the patient; (3) beneficence, doing good for the patient; (4) justice, fairness to the patient; and (5) professional-patient relationship.
What is the ethical paradigm of medicine?
The ethical paradigm in medicine that immediately precedes principlism is now often referred to as benevolent paternalism, a term usually with negative connotations. Principlism has supplanted paternalism and now is the primary method that is currently taught at professional schools for health care clinicians.
What is Principlism in health care?
Principlism is a normative ethical framework that was designed for practical decision making in health care . Its basic approach is an attempt to bypass intractable disagreements at the level of normative ethical theory and the resulting lack of agreement about how to proceed. Instead, the authors focus on what people generally do agree upon, in the form of general, mid-level principles. They observe that “often little is lost in practical moral decision making by dispensing with general moral theories. The rules and principles shared across these theories typically serve practical judgment more adequately (as starting points) than the theories” (Beauchamp & Childress, 1994, p. 17). They say that this is because “theories are rivals over matters of justification, rationality and method but they often converge on mid-level principles” (Beauchamp & Childress, 1994, p. 102). Due to this general convergence on principles, they call principlism a common-morality approach.
What is Principlism in philosophy?
Approaching the work from a strongly theory-based perspective, the authors claim that principlism lacks a sufficient theoretical foundation . For them, since principlism lacks a “moral theory that ties the ‘principles’ together, there is no unified guide to action which generates clear, coherent, comprehensive and specific rules for action nor any justification of those rules” (Clouser & Gert, 1990, p. 227). Others point out that these authors have different expectations of moral “theory” and that they cannot but arrive at incompatible conclusions about what works or about what is acceptable (e.g., Davis, 1995), whether in terms of foundations, methodologies, justification, etc. Proponents of a principlist approach do not expect or wait for general agreement upon something that could satisfy these theoretical aspirations. Instead of debating those issues, they focus (and depend) on the mid-level principles where a certain degree of agreement is said to exist already.
Why do clinicians start with mid level principles?
Starting with mid-level principles allows clinicians to “get straight to work” on ethical deliberation without becoming enmeshed in theoretical debates and without the need to specialize in theories and their justificatory mechanisms, their nuances, etc.
What is the normative framework for health care?
Principlism is a normative ethical framework designed for decision making in health care. It is a common-morality approach relying on four mid-level principles: respect for autonomy, nonmaleficence, beneficence, and justice. The normative force of the principles arises from a
What are the tools used in public health?
In public health, the tools used for applying ethics in practice generally take the form of ethical frameworks. Since about 2001, numerous frameworks have been developed to guide ethical decision making in diverse areas of practice, with early influential examples including Kass (2001), Upshur (2002) and Childress et al. (2002), and with more recent examples including Willison et al. (2012), ten Have, van der Heide, Mackenbach, & de Beaufort (2012), and Marckmann et al. (2015). To date, the field of public health ethics has produced a diversity of frameworks for various purposes, which is a dramatically different landscape from the more monolithic terrain of medical ethics in which principlism dominates.
What are the 4 principles of principlism?
Principlism, the bioethical theory championed by Tom Beauchamp and James Childress, is centered on the four moral principles of beneficence, non-maleficence, respect for autonomy, and justice.
What is principlism and frameworks in public health ethics?
Part one – What is principlism? Principlism is a normative ethical framework that was designed for practical decision making in health care. Its basic approach is an attempt to bypass intractable disagreements at the level of normative ethical theory and the resulting lack of agreement about how to proceed.
What is principlism medical ethics?
Principlism is a normative ethical framework designed for decision making in health care. It is a common-morality approach relying on four mid-level principles: respect for autonomy, nonmaleficence, beneficence, and justice.
What is the principlism approach?
Principlism. Principlism is a commonly used ethical approach in healthcare and biomedical sciences. It emphasises four key ethical principles of autonomy, beneficence, non-maleficence, and justice, which are shared by most ethical theories, and blends these with virtues and practical wisdom.
What is an example of principlism?
Moral Conflicts and Their Resolution. In principlism, moral problems arise because of conflicts of prima facie duties. Classic examples are problems of paternalism where physicians seek to provide health benefits by overriding a patient’s autonomous choice.
What is Principlism in medicine?
Principlism aims to provide a framework to help those working in medicine both to identify moral problems and to make decisions about what to do. For it to meet this aim, the principles included within it must express values that all morally serious people share (or ought to share), and there must be no other values that all morally serious people share (or ought to share). This paper challenges the latter of these claims. I will argue that as a descriptive claim about what values morally serious people do in fact share, principlism is inadequate; more principles would be needed to make this claim true. Furthermore, I will argue that while, taken as a claim about what principles we ought to share, principlism could turn out to be correct, it is either unsupported or unable to meet its aims. The only way in which principlists can avoid these problems is to add to the current four principles.
What is the purpose of principles in medicine?
Principlism aims to provide a framework to help those working in medicine both to identify moral problems and to make decisions about what to do . For it to meet this aim, the principles included within it must express values that all morally serious people share (or ought to share), and there must b …
What is the principle of healthcare?
Principlism is also a consequential theory widely applied in the healthcare sector. The theory is based on four principles that include autonomy. The second principle is the non-maleficence, the third principle is beneficence, and the fourth principle is justice. Principles provided by the principles theory are less general several other theories in making ethical decisions but can be applied in the rules, cases, and virtues in the healthcare profession.
What are the weaknesses of the Principlism Theory?
Weaknesses. The theory replaces the moral theory and rules with principles that are one of the greatest we aknesses of the principlism theory. Hence, The theory misses several moral problems that are common in the healthcare environment. This makes the theory either misleading or impractical in such situations.
Why are ethical theories important in healthcare?
Ethical theories are a significant part of the healthcare profession. They help healthcare providers overcome challenges and conflicts that arise in the profession. These difficulties and conflicts stem from competing personal, organizational, professional and societal values through which healthcare professionals are required to make critical ...
What is utilitarianism in healthcare?
When applied in the healthcare setting, the theory gives a medical professional the power to decide what is best depending on the circumstance. The utilitarianism approach provides a solution when one is faced with a situation where a decision has to make on choosing one option of the other especially when the best alternative available is morally wrong. According to Mack (2004), the theory lays a strong emphasis on impartiality and unselfishness as it does not require one to refer to the precedent actions on if they worked for the decision or not
How can the theory of ethics be applied to healthcare?
In the healthcare sector, the theory can be applied in making ethical decisions in situations that require minimizing pain and maximizing pleasure even when the decision is morally wrong. It focuses on benefiting the majority while agrees with common sense making its principles fair and widely accepted.
How does the theory of ethics work in real life?
It dictates the ethical decisions made by an individual must behold his point of view and interests to promote the happiness of others, making the theory very practical in real life. The strengths of the theory have been very applicable in balancing the costs and benefits in health care.
What is beneficence in healthcare?
Beneficence focuses on compassion derived from the desire to do well and improve the wellness of others. The theory approaches beneficence as the basis of morality and human nature principles (DeMarco, 2005). Using this principle, the healthcare providers have a responsibility to consider the pain experienced by the patients in their decisions.