Why do prescriptions need prior authorization?
What types of medications typically need approval?
- Those that may be unsafe when combined with other medications
- Have lower-cost, equally effective alternatives available
- Should only be used for certain health conditions
- Are often misused or abused
- Drugs often used for cosmetic purposes
What services require prior authorization?
- Substance abuse treatment
- Psychosocial rehabilitation
- Supportive housing
- Specialized residential treatment
- Most mental health tests done by your Case Manager/Agency or health provider
- Investigational and experimental procedures and treatments
- Nonemergency hospital services
What does prior authorization mean on a prescription?
Prior authorization is the formal approval issued by a health insurance provider that's needed before certain procedures may be performed or medications are prescribed. Without this approval, the insurer won't cover the cost of the procedure.
How to get a prior authorization request approved?
Work together
- Identify who at your doctor’s office handles prior authorizations. ...
- Ask your doctor for success stories of patients who have had similar requests. ...
- Someone in your doctor’s office likely has an existing pre-authorization process and knows the typical steps. ...
- Your doctor’s team may have an approach they use to show the medical necessity of a treatment. ...
What does prior authorization mean for a medication?
What is prior authorization? This means we need to review some medications before your plan will cover them. We want to know if the medication is medically necessary and appropriate for your situation. If you don't get prior authorization, a medication may cost you more, or we may not cover it.
Why do some medicines need prior authorization?
Your insurance company may require prior authorization before covering certain prescriptions. This is to ensure that the medication is appropriate for your treatment. It also helps to make sure it's the most cost-effective option. When prior authorization is granted, it is typically for a specific length of time.
How long does pre authorization take for medication?
How does the prior authorization process work? Typically, within 5-10 business days of receiving the prior authorization request, your insurance company will either: Approve your request.
What types of medication may require a prior authorization?
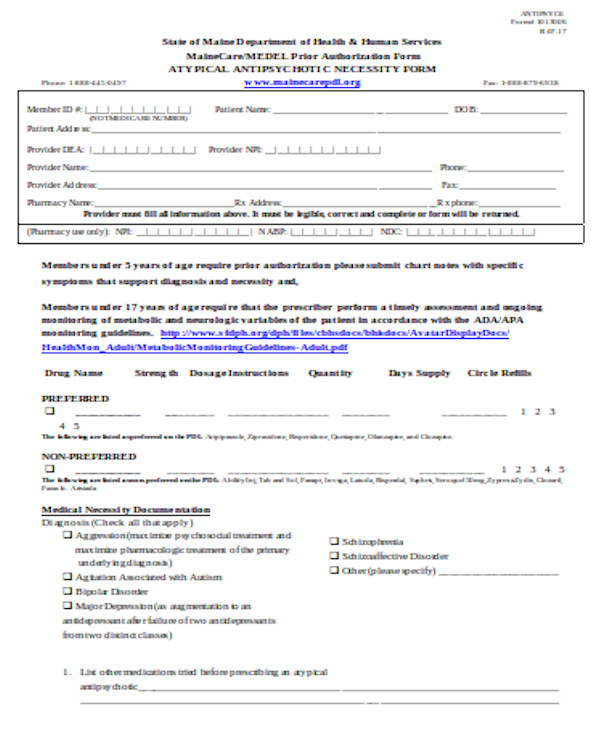
Most common prescription drugs requiring preauthorization:Adapalene (over age 25)Androgel.Aripiprazole.Copaxone.Crestor.Dextroamphetamine-amphetamine (quantity limit)Dextroamphetamine-amphetamine ER (over age 18)Elidel.More items...
How does the prior authorization process work?
Prior authorization (also called “preauthorization” and “precertification”) refers to a requirement by health plans for patients to obtain approval of a health care service or medication before the care is provided. This allows the plan to evaluate whether care is medically necessary and otherwise covered.
What happens if a prior authorization is denied?
What happens if prior authorization is denied? If your insurance company denies pre-authorization, you can appeal the decision or submit new documentation. By law, the insurance company must tell you why you were denied. Then you can take the necessary steps to get it approved.
How long do pre authorization holds last?
around 5 daysA pre-authorization (also “pre-auth” or “authorization hold”) is a temporary hold on a customer's credit card that typically lasts around 5 days, or until the post-authorization (or “settlement”) comes through.
Why do prior authorizations take so long?
Obtaining a prior authorization can be a time-consuming process for doctors and patients that may lead to unnecessary delays in treatment while they wait for the insurer to determine if it will cover the medication. Further delays occur if coverage is denied and must be appealed.
Can a pharmacist red flag you?
Although it is argued to be a breach of a person's privacy, the Red Flag system can be used to catch prescription drug abusers and medical identity theft. Pharmacies are allowed to deny purchases if they feel the person is buying too much of the same prescribed medication. Look into your medical history.
Why does Adderall need prior authorization?
Prior Authorization is a cost-savings feature of your prescription benefit plan that helps ensure the appropriate use of selected prescription drugs. This program is designed to prevent improper prescribing or use of certain drugs that may not be the best choice for a health condition.
Who is responsible for obtaining preauthorization?
healthcare providerThe healthcare provider is usually responsible for initiating prior authorization by submitting a request form to a patient's insurance provider. As mentioned in the “How does prior authorization work?” section above, this will then often prompt a time-consuming back and forth between the provider and payer.
Why does Express Scripts require prior authorization?
When your pharmacist tells you that your prescription needs a prior authorization, it simply means that more information is needed to see if your plan covers the drug. Only your doctor can provide this information and request a prior authorization. 2.
Who is responsible for obtaining preauthorization for patient hospitalization?
In most cases, your healthcare provider will start the prior authorization if they are in-network. However, if you are using a healthcare provider that is not in your plan's network, then you may be the one responsible for getting prior authorization.
How does Prior Authorization work?
Getting prior authorizations approved involves many people – primarily patients, healthcare professionals, and the patients’ health insurance companies.
Why do insurance companies require prior authorization?
These prior authorizations save money for insurers by bypassing unnecessary or expensive treatment options when other equally effective options exist that are included in the plan’s formulary. The formulary includes the list of medications that are covered under an insurance plan. This process is needed not only to ensure minimizing prescription costs, but also to verify that what is being prescribed is medically necessary and appropriate for the patient.
Why do insurance companies update their formularies?
Insurance companies continually update their formularies to include drugs that are most effective to treat different disease states that are also cost effective. This ensures that medications that are covered by plans will reflect guideline changes. Prior authorizations also verify that certain medications aren’t being duplicated if patients see multiple specialists. This keeps patients safe from potential adverse effects and encourages appropriate medication usage.
How many physicians believe prior authorizations have increased in the past 5 years?
A 2019 study from the American Medical Association reported that 86% of physicians believe that prior authorizations have increased in the prior 5 years. Physicians believe that they are too time consuming and detract from time spent with patients.
Why is it important to have a prior authorization certified specialist?
There are great benefits to having a Prior Authorization Certified Specialist on staff to help with the administrative process.
Why is it important to have documentation of step therapy?
It is also be important to have good documentation policies. If a prior authorization requires step therapy in its criteria, each trial will need to be documented. Having documentation of all prior attempts will help expedite the approval process.
What is a PA?
Prior authorization (prior auth, or PA) is a management process used by insurance companies to determine if a prescribed product or service will be covered. This means if the product or service will be paid for in full or in part. This process can be used for certain medications, procedures, or services before they are given to the patient.
What is prior authorization?
Prior authorization is a requirement that your physician or hospital obtains approval from your health insurance company before prescribing a specific medication for you or performing a particular medical procedure. Without this prior approval, your health insurance plan may not pay for your treatment, leaving you with the bill instead.
Why is prior authorization important?
The idea is to ensure that health care is cost-effective, safe, necessary, and appropriate for each patient. But prior authorization requirements are also controversial, as they can often lead to treatment delays and can be an obstacle between patients and the care they need.
How long does it take to respond to a non-urgent prior authorization request?
The ACA also grants enrollees in non-grandfathered health plans access to an internal and external appeals process. Insurers have 15 days 3 (or less, at state discretion) to respond to a non-urgent prior authorization request.
What is pre-authorization requirement?
In effect, a pre-authorization requirement is a way of rationing health care. Your health plan is rationing paid access to expensive drugs and services, making sure the only people who get these drugs or services are the people for whom the drug or service is appropriate.
Why are prior authorizations controversial?
But prior authorization requirements are also controversial, as they can often lead to treatment delays and can be an obstacle between patients and the care they need. Particularly for patients with ongoing, complex conditions that require extensive treatment and/or high-cost medications, continual prior authorization requirements can hinder the patient's progress and place additional administrative burdens on physicians and their staff. 1
Why do insurance companies require prior authorization?
Your health insurance company uses a prior authorization requirement as a way of keeping healthcare costs in check. It wants to make sure that: The service or drug you’re requesting is truly medically necessary. The service or drug follows up-to-date ...
What is a service or drug?
The service or drug follows up-to-date recommendations for the medical problem you’re dealing with. The drug is the most economical treatment option available for your condition. For example, Drug C (cheap) and Drug E (expensive) both treat your condition.
What Does Prior Authorization Mean?
Prior authorization for prescription drugs is required when your insurance company asks your physician to get specific medications approved by the insurance company. Prior authorization must be provided before the insurance company will provide full (or any) coverage for those medications.
How Long Does Prior Authorization Take?
Prior authorization can take days to process. Within a week, you can call your pharmacy to see if the prior authorization request was approved. If it wasn’t, you can call your insurance company to see why the authorization was delayed or denied..
What Kinds of Medications Warrant Prior Authorization?
There are several reasons a medication may require a prior authorization request. For example, the prescription may:
What to do if your doctor does not have prior authorization?
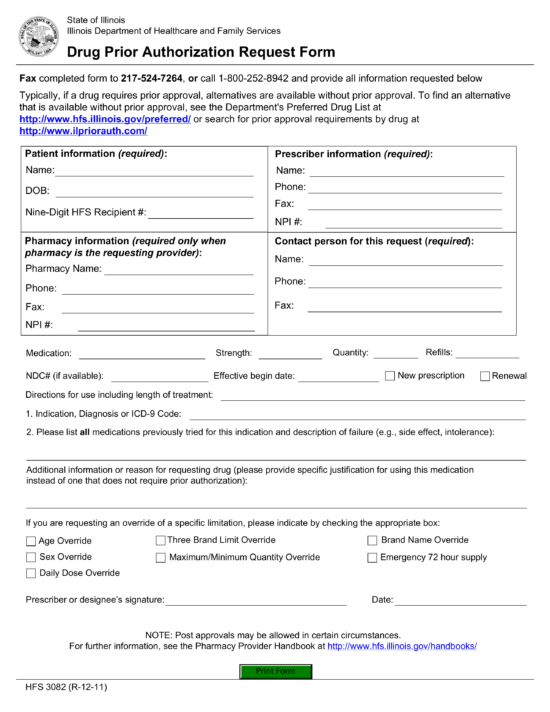
Step 1: Your pharmacy will contact if your doctor if he or she did not obtain prior authorization from the insurance company when prescribing a medication.
How to find out if you need prior authorization?
Also, pharmacies (like Caremark) often create lists of prescriptions that will require some form of pre-authorization. However, if your doctor has not filled out a prior authorization request, you will most likely find out at your pharmacy when you try to fill or pick up the prescription.
Why do insurance companies pre-authorize medications?
In short, health insurance companies pre-authorize medications in order to keep healthcare costs low. By ensuring that your medication is medically necessary, up-to-date, as economical as possible, and isn’t being duplicated, health insurance companies can afford to provide more expensive medications to those who truly need it.
What happens if you don't fill out a prior authorization?
However, if your doctor has not filled out a prior authorization request, you will most likely find out at your pharmacy when you try to fill or pick up the prescription.
What is a prior authorization?
Prior authorization is a restriction put in place by insurance companies, so they can decide whether or not they will pay for certain medicines. It doesn’t affect cash payment for prescriptions, and it’s only required on those prescriptions when billed through insurance —so if you’re uninsured or if you decide to pay in cash, you won’t need to worry about getting prior authorization.
What should I expect if my prescription needs a prior authorization?
If your prescription requires a prior authorization, the pharmacy will notify your healthcare provider, who will provide the necessary information to your insurance company. Your insurer will then decide whether or not to cover your medicine, and you should hear back from your pharmacist about their decision within two days. Remember, if you are approved, a prior authorization only lasts for a set period of time, and you will likely have to re-apply again for future fills.
Can insurance deny prior authorization?
Unfortunately, your insurer can deny you prior authorization, and you may be left on the hook for the full out-of-pocket price of your drug.
What is a prior authorization (PA) for a prescription drug?
Healthcare.gov defines prior authorization “approval from a health plan that may be required before you get a service or fill a prescription in order for the service or prescription to be covered by your plan”. The general process has many names including precertification, pre-authorization, prior approval, and predetermination.
Why are prior authorizations necessary in the first place?
While PAs may seem like a hassle to both patients and medical providers, they play a vital role in helping to manage prescription drug costs by ensuring that certain high-cost or high-risk medications are used in a manner that is both clinically and economically appropriate. “Think of it this way”, says VativoRx’s Clinical Pharmacy Director, William Lineberry, PharmD, BCGP. “We wouldn’t use a $5,000 IV antibiotic that works against rare strains of multi-drug resistant, or MDR, bacteria to treat a common case of strep throat. Sure, that IV antibiotic would be effective, but so would a $5 bottle of Augmentin.” Lineberry says “In a nutshell, the role of the PA process is to make sure that we aren’t using that $5,000 IV to treat strep throat, while also maintaining access to that $5,000 IV for someone with legitimate medical necessity.”
How does VativoRx make the prior authorization process better for everyone?
That’s where an experienced PBM can do better. While PAs may seem like a hassle to the patient, they help save money for everyone involved. “We understand that time is a finite resource,” said VativoRx CEO Lisa Quarterman. “If we can save time and worry for patients and their doctors, we’re happy.” “We take a balance approach when it comes to prior authorizations. We find the best approach is one the looks out for the best interests of the patient and our clients. We allow access to more expensive and clinically superior drugs if the benefit is justifiable while restricting the use of other drugs that have cheaper but equally effective options.”
How do you fight a prior authorization denial?
Ask your doctor or nurse if they can help you with preparing a response to a denial of prior authorization. There are several things they can do.
How Long Does it Take to Get Prior Authorization for a Prescription?
The speed of a prior authorization can vary drastically from hours to days de pending on a number of factors.
Why is prior authorization important?
Ultimately, a prior authorization is an annoying but necessary part of health insurance. It helps keep health insurance costs down which in turn makes health insurance plans more affordable for everyone.
Why Do Insurance Companies Require Prior Authorization?
In short, health insurance companies use pre-authorizations to keep costs low.
What Can I Do If My Prior Authorization is Denied?
If your request is rejected, you or your doctor can ask for a review of the decision.
Who is Responsible for Completing a Prior Auth Request?
Most of the time, your doctor is responsible for initiating a prior authorization.
What happens if your doctor prescribes a brand name drug?
If your doctor prescribes the more expensive brand name drug, the insurance company just wants an explanation, a prior auth, before they pay for it. When the explanation is acceptable to your insurance then the prior auth will be approved. When the explanation is not acceptable to your insurance, then your doctor can switch you to ...
What is NowRX pharmacy?
NowRx Pharmacy is a new kind of local pharmacy built from the ground up to deliver a better pharmacy experience. We use modern technology inside the pharmacy to provide better pricing, better service, and better convenience. Visit our NowRx Pharmacy Frequently Asked Questions to learn more.
What is the purpose of prior authorization?
The fundamental goal of prior authorization is to promote the appropriate use of medications. Pharmacists in all practice settings must develop specific guidelines to ensure that the prior authorization process is administered in the most efficient manner possible, is fully compliant with statutory and regulatory requirements, and provides members, prescribers and pharmacists with an evidence-based, rational process to promote appropriate drug use.
Why is prior authorization important?
Requiring prior authorization in a drug benefit can effectively help avoid inappropriate drug use and promote the use of evidence-based drug therapy. Such efficient and effective use of health care resources can minimize overall medical costs, improve health plan member access to more affordable care and provide an improved quality of life. 3
What is Prior Authorization and Why is it an Essential Managed Care Tool?
Prior authorization (PA) is an essential tool that is used to ensure that drug benefits are administered as designed and that plan members receive the medication therapy that is safe, effective for their condition, and provides the greatest value. Prior authorization requires the prescriber to receive pre-approval for prescribing a particular drug in order for that medication to qualify for coverage under the terms of the pharmacy benefit plan. 1 Drugs that require prior authorization will not be approved for payment until the conditions for approval of the drug are met and the prior authorization is entered into the system. Prior authorization procedures and requirements for coverage are based on clinical need and therapeutic rationale. The process gives the prescriber the opportunity to justify the therapeutic basis for the prescribed medication. 2 Administration of a prior authorization process must take into consideration the desired outcome for the patient, the design of the drug benefit, the value to the plan sponsor, and all statutory and regulatory requirements. Prior authorization may also be referred to as “coverage determination,” as under Medicare Part D.
What is closed formulary pharmacy?
Under a closed formulary pharmacy benefit, the health plan or payer provides coverage at the point-of-sale only for those drugs listed on the formulary. The prior authorization process can be used by prescribers and patients to request coverage for drugs that are not included on a plan’s formulary.
How many members does the Academy of Managed Care Pharmacy have?
AMCP has more than 4,800 members nationally who provide comprehensive coverage and services to the more than 200 million Americans served by managed care. More news and information about AMCP can be obtained on their website, at www.amcp.org.
Why would a patient need a non-formulary drug coverage exception?
For example, to protect against cardiovascular disease, a patient may need significant reductions in LDL (bad) cholesterol levels that may not be achievable with a health plan's formulary drug and therefore a coverage exception for a high-potency non-formulary medication would be requested using the plan's exception process provided certain circumstances are met to ensure patient safety and appropriate utilization.
Who develops prior authorization guidelines?
Guidelines and administrative policies for prior authorization are developed by pharmacists and other qualified health professionals Each managed care organization develops guidelines and coverage criteria that are most appropriate for their specific patient population and makes its own decisions about how they are implemented and used. Well-designed prior authorization programs consider the workflow impact on health care system users and minimize inconvenience for patients and providers.
