What are reactionary dentin and reparative dentin?
Tunnels crossing the reparative dentin formation prevent the total closure of the bridge. Reactionary dentin ( rd) is separated from the dentin layer formed prior capping by calciotraumatic lines ( ctl ). The mesial and distal pulp horns remain non-mineralized ( white asterisks ).
Is the collagen framework of Reactionary dentin modified?
The collagen framework of reactionary dentin is modified and yet highly regular, patterned and non-stochastic. The altered collagen network parallels increased deposition of DSP as a putative calcium nucleation site.
Is deposition of Reactionary dentin a stochastic process?
Deposition by odontoblasts of a relatively atubular reactionary dentin is an efficient strategy to impede or delay microbial progression, evident from the protracted nature of dental caries [8]. While modified, the synthesis of reactionary dentin matrix is not a stochastic process.
What is newly secreted dentin?
Newly secreted dentin is unmineralized and is called predentin. It is easily identified in hematoxylin and eosin stained sections since it stains less intensely than dentin. It is usually 10-47μm and lines the innermost region of the dentin. It is unmineralized and consists of collagen, glycoproteins, and proteoglycans.
What is reparative dentin?
Introduction. Reparative dentinogenesis is the biological regeneration of dentin from new odontoblast-like cells when a dental injury is severe and reaches up to the dental pulp (Smith et al., 1995; Simon et al., 2012).
What are the 4 types of dentin?
General Dentistry Concepts: DentinDevelopment. The formation of dentin begins prior to the formation of the enamel. ... Structure. Dentin, unlike enamel, can be demineralized and stained for histological study. ... Types. ... Primary dentin. ... Secondary dentin. ... Tertiary dentin.
How does reactionary dentine affect progression of caries?
In addition to slowing down pathogen progression into the dental pulp, reactionary dentin formation provides a supportive matrix for nerve sprouting into the caries-affected area.
What are the three types of dentin?
There are three types of dentin, primary, secondary and tertiary.
What are the different types of dentine?
Dentine TypesPrimary dentine forms before tooth eruption.Secondary dentine forms after eruption, as the tooth develops with age. ... Reparative or tertiary dentine forms as a result of trauma to the odontoblasts; this can be thermal, chemical, bacterial or mechanical.
What is Eburnated dentin?
Eburnated dentin: It is type of reactive sclerotic dentin which is formed due to destruction by slow caries process or mild chronic irritation and results in hard, darkened cleanable surface on outward portion of reactive dentin.
How long does it take for reparative dentin to form?
Reparative dentin is observed at 2 weeks but does not cover exposed pulp tissue even at 3 weeks. D: dentin, P: pulp tissue, and R: reparative dentin.
How does Dycal work?
Our results evidence that pulp capping with Dycal, as well as with Hydrogel, stimulates the formation of reactionary dentin at the periphery of the pulp chamber. Dycal contributes to the partial closure of the pulp exposure, producing a defective reparative dentinal bridge.
What is Interglobular dentin?
Interglobular dentine (IGD) is an area of poorly mineralized dentine matrix. It has been reported that there is an association between the retraction of odontoblast processes (OP) and the formation of IGD. A variation of the extent of OP has been described depending on the region of the tooth and age.
What is Dentinogenesis imperfecta?
Dentinogenesis imperfecta is a disorder of tooth development. This condition causes the teeth to be discolored (most often a blue-gray or yellow-brown color) and translucent.
What is Intratubular dentin?
The intertubular dentin, which lies between the tubules, is a less-calcified matrix that consists of some apatite crystals embedded within a collagen matrix.
How do odontoblasts form dentin?
During odontogenesis, odontoblasts are critical for the formation of a primary dentin, until the tooth becomes functional. When contacts between antagonistic cusps are established, then the formation of secondary dentinstarts immediately, and continues throughout life. Initially, odontoblasts constantly produce matrix molecules that result in the formation of a 10 micrometers thick layer, reduced afterward to a daily 4 micrometers deposit. However, there is not much difference between primary and secondary dentin. The only major difference is morphological, and the S-curve of the tubules is more accentuated in the secondary dentin, due to the gradual space restriction of odontoblasts, located at the periphery of a withdrawing pulp.
Where are dentin cells located?
Phylogenetic studies have revealed that during evolution, originally dentin analogues were very similar to bone, with osteoblast/odontoblast-like cells located within alveoli, as it is the case for osteocytes surrounded by bone within lacunae [1,2]. This organization called osteodentin, is still observed during tooth development in some mammalian species such as rodents [3], and as reparative dentin in humans. Odontoblasts polarize, elongate and start to display two distinct parts: a cell body and a process. During the next step of evolution, the cell bodies are located outside the mineralized tissue, along the border of the mineralization front, and long processes occupy the lumen of dentin tubules. In contrast with bone, dentin is not vascularized, except in some fish teeth where the existence of vasodentinis well-documented [4]. When mammalian odontoblasts become terminally polarized, they produce an orthodentin, with cell bodies located outside the predentin/dentin layer at the periphery of the pulp and cell processes crossing the predentin and extending inside dentin tubules up to the dentin-enamel junction. Tubules are characteristic of orthodentin. The diameter of tubules varies between 2 and 4 micrometers. The number of dentine tubules is about 18 000 and 21 000 tubules per mm2 [5]. They are more numerous in the inner third layer than the outer third layer of the dentin.
What is the difference between intertubular and peritubular dentin?
Differences in the structure and composition of the two dentins are well documented. Type I collagen is the major protein of intertubular dentin (90%), whereas no collagen fibrils are observed in the peritubular dentin. Differences have been also reported in the composition of non-collagenous proteins of the two dentins [15–18]. Along these lines, some crystallo-chemical specificities of the inter- and peri-tubular dentins have been established.
What is the largest part of the dentin layer?
The circumpulpal dentin forms the largest part of the dentin layer. Thin at initial stages of dentinogenesis, its thickness continuously increases (about 4mm/day) at the expense of the space initially occupied by the pulp. Again, it is not a homogeneous dentin layer. The most prominent part of the circumpulpal dentin is formed by intertubular dentin, whereas peritubular dentinis found around the lumen of the tubules,. The ratio between inter-tubular and peri-tubular dentin is highly species dependant. Peritubular dentin is missing in the continuously growing rodent incisors. In contrast, in horses, the ratio is roughly 50%, and decreases in humans (about 10–20%), with huge variations depending on the area where the calculations are made.
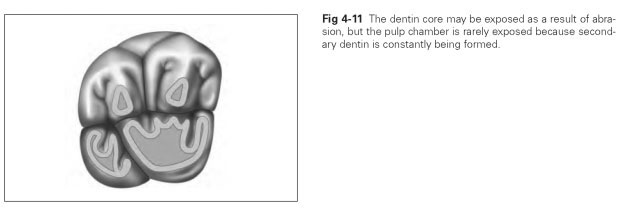
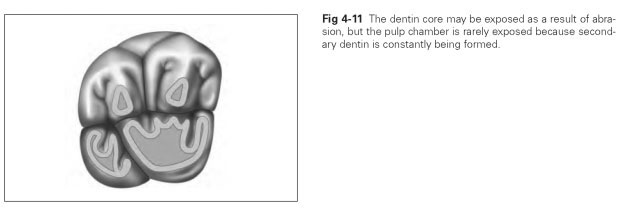
What is the thick layer of dental tissue?
A thick dentin layer forms the bulk of dental mineralized dental tissues. Dentin is capped by a crown made of highly mineralized and protective enamel, and in the root, it is covered by cementum, a structure implicated in the attachment of the teeth to the bony socket. Teeth contain in their central parts dental pulps, which are usually non-mineralized. This soft connective tissue also contains nerves and a vascular network connected with the surrounding tissues, the periodontal ligament and the bony socket. Taken as a whole, the general composition of dentin is summarized in Table 1.
What is the mantle dentin?
In the crown, the so-called mantle dentin, indentation measurements using Vickers microhardness show a gradual increase in hardness along the outer 200mm [7]. This outer layer is less mineralized and consequently the resilient mantle dentin may be adapted for dissipating pressures or forces which otherwise would induce enamel fissures and detachment of the fragmented enamel from the outer dentin-enamel junction. Dentin tubules are missing or reduced in number and bent in these layers of outer dentin. For some years, there was a debate about the observation that when using the “stains all” staining method [8] or antibodies raised against dentin phosphoproteins [9] the mantle dentin was unstained in contrast with the circumpulpal dentin, and consequently Takagi and Sasaki suggested that this layer was deprived of phosphorylated proteins [8]. However, chemical analysis revealed that proteins usually phosphorylated are actually present but in an underphosphorylated form or not phosphorylated at all [10]. In this context it is interesting to note that the mantle dentin is unaffected in X-linked hypophosphatemia [11] whereas in contrast rickets produces within the circumpulpal dentin enlarged non-mineralized interglobular spaces containing dentin ECM molecules [12]. Hence, the nature of the NCP’s differs between the mantle and circumpulpal dentins, the outer layer being not influenced by the organic phosphorous status. As a consequence, in the crown, the outer layers are less mineralized than the rest of the dentin. They display some elastic properties and therefore provide some resilience, important from a mechanical point of view and allowing dissipation of stress forces [7]. However, the thickness of the outer layer is about 200mm, therefore larger than the presumed width of the mantle dentin.
Where do odontoblasts secrete ECM?
Depending of the labeled precursor, secretion either occurs in the proximal predentin or at the distal predentin- inner dentin edge . The two different sites are related respectively 1- to the release of collagen fibrils and their associated proteoglycans in predentin, or 2- to the discharge of non-collagenous phosphorylated proteins and mineral associated proteoglycans that are secreted at the mineralization front or metadentin [22]. Some matrix components migrate directly from the serum to the dentin compartment. They follow mainly an intercellular pathway, albumin and phospholipids being implicated in the transport of mineral toward and therefore in the mineralization process of intertubular dentin.
What are the two types of pathological dentin?
In dental tissues, two types of pathological dentin have been identified after the adverse effects due to either slow dental caries or rapid pul p exposure. In carious-exposed teeth, odontoblasts and cells from the sub-odontoblastic Hoehl’s layer were implicated in the formation of reactionary dentin. Beneath calciotraumatic lines, indirect capping induced the formation of bone-like (osteo) dentin. Deeper lesions combined with pulp exposure contributed to the construction of reparative dentin by pulp cells. Indirect capping produced reactionary dentin, while direct pulp capping led to the formation of reparative dentin by a dentinal bridge, closing almost the whole pulp exposure.
How long after pulp capping does the reparative dentinal bridge form?
a, b Formation of a reparative dentinal bridge (rep) 4 weeks after pulp capping (Alizarin red and Masson’s trichrome). Tunnels crossing the reparative dentin formation prevent the total closure of the bridge. Reactionary dentin ( rd) is separated from the dentin layer formed prior capping by calciotraumatic lines ( ctl ). The mesial and distal pulp horns remain non-mineralized ( white asterisks ). Bars: 100 μm
How long after implantation of dentin is it measured?
Measurements of the thickness of reactionary dentin were performed on figures printed at the same magnification with ImageJ software (National Institutes of Health, MD), 4 weeks after implantation of the capping agent. Despite the complexity of the tri-dimensional coronal pulp structure, the specific distribution of reparative dentin was evaluated after 1 month in Dycal- and Hydrogel-capped molars. Results were compared with Kruskal Wallis and Mann Whitney U tests at p = 0.05.
Is hydrogel capping a reactionary or reparative?
To conclude, the formation of reactionary and reparative dentin was enhanced by Hydrogel capping compared to Dycal capping. The isthmus located between the pulp horns collapsed and merged. Three weeks after Hydrogel capping, the dentinal bridge occluding the pulp exposure was homogeneous, in contrast with the conclusions previously reported obtained after Dycal capping. Therefore, substantial differences were evident between a solid Hydrogel-induced dentinal bridge and tunnel disturbances shown after Dycal capping. Hence, Hydrogel might present some clinical advantages over Dycal capping.
What is a dentine?
FMA. 55628. Anatomical terminology. Dentin ( / ˈdɛntɪn /) ( American English) or dentine ( / ˈdɛnˌtiːn / or / ˌdɛnˈtiːn /) (British English) ( Latin: substantia eburnea) is a calcified tissue of the body and, along with enamel, cementum, and pulp, is one of the four major components of teeth.
How is dentin formed?
The formation of dentin, known as dentinogenesis, begins prior to the formation of enamel and is initiated by the odontoblasts of the pulp. Dentin is derived from the dental papilla of the tooth germ. The tooth germ is the primordial structures from which a tooth is formed, including the enamel organ, the dental papilla, and the dental sac enclosing them. After growth of predentin and maturation into dentin, the cell bodies of the odontoblasts remain in the pulp inside the tooth, along its outer wall, and project into tiny tubules in the dentin. Dentin continues to form throughout life and can be initiated in response to stimuli, such as tooth decay or attrition.
What is the term for a change in the structure of teeth characterized by calcification of dentinal tub?
Dentinal sclerosis. Dentinal sclerosis or transparent dentin sclerosis of primary dentin is a change in the structure of teeth characterized by calcification of dentinal tubules. It can occur as a result of injury to dentin by caries or abrasion, or as part of the normal aging process. Dentinal sclerosis.
What is the difference between dentin and enamel?
There are two main characteristics which distinguish dentin from enamel: firstly, dentin forms throughout life ; secondly, dentin is sensitive and can become hypersensitive to changes in temperature due to the sensory function of odontoblasts, especially when enamel recedes and dentin channels become exposed.
Why does dentin wear away faster than enamel?
Because dentin is softer than enamel , it wears away more quickly than enamel. Some mammalian teeth exploit this phenomenon, especially herbivores such as horses, deer or elephants. In many herbivores, the occlusal (biting) surface of the tooth is composed of alternating areas of dentin and enamel. Differential wearing causes sharp ridges of enamel to be formed on the surface of the tooth (typically a molar ), and to remain during the working life of the tooth. Herbivores grind their molars together as they chew ( masticate ), and the ridges help to shred tough plant material.
Where are dentinal tubules located?
The dentinal tubules extend from the dentinoenamel junction (DEJ) in the crown area, or dentinocemental junction (DCJ) in the root area, to the outer wall of the pulp. From the outer surface of the dentin to the area nearest the pulp, these tubules follow an S-shaped path.
Where do odontoblasts grow?
After growth of predentin and maturation into dentin, the cell bodies of the odontoblasts remain in the pulp inside the tooth, along its outer wall, and project into tiny tubules in the dentin. Dentin continues to form throughout life and can be initiated in response to stimuli, such as tooth decay or attrition.
What is the dentine-pulp complex response in deep caries?
The dentine-pulp complex response in deep caries is histological characterized by tertiary formation and mild chronic pulp inflammation. The quiescent primary odontoblasts are reactivated, laying down reactionary tertiary dentine. In more severe carious damage the primary odontoblasts die and reparative tertiary dentine is secreted by odontoblast-like cells, which are differentiated in adult teeth mainly from dental pulp stem cells DPSC. Though associated with reversible pulpitis DPSC still preserve in deep caries the capability of migration, proliferation and differentiation. Some common mechanisms of molecular signals involved in tertiary dentine formation might also explain the balance between inflammation and regeneration of dentine-pulp complex.
What are the non-collagenous proteins in dentine?
The non-collagenous proteins (NCPs) present in the dentine extracellular matrix (ECM) include growth factors (TGF-β1, BMP-7, FGF-2, IGF-1 and -2, NGF, and GDNF), extracellular matrix molecules (DSP, DPP, BSP, DMP-1, and DSPP), and both anti- and pro-inflammatory chemokines and cytokines (TNF-α, IL-1, IL-6, and IL-10). Molecules such as DSP and DPP are mainly expressed by odontoblasts, and they are cleaved products from dentine sialophosphoprotein (DSPP). Some molecules, such as TGF-β1, specifically interact with decorin/biglycan in dentine. Although TGF-β1 increases the expression and secretion of NGF in human pulp cells, NGF induces mineralization and increases the expression of DSPP and DMP-1. Furthermore, GDNF may act as a cell survival factor and mitogen during tooth injury and repair. Pulp capping materials, such as MTA and calcium hydroxide, can solubilize bioactive dentine molecules (TGF-β1, NGF, and GDNF) that stimulate tertiary dentineogenesis. The binding of these signaling molecules leads to activation of several signaling transduction pathways involved in dentinogenesis, odontoblast differentiation and inflammatory responses, such as the p38 MAPK, NF-kβ and Wnt/β-catenin signaling pathways. Understanding the cascade of cellular and molecular events underlying the repair and regeneration processes provides a reasonable new approach to VPT through a targeted interaction between tooth tissue and bioactive molecules.
How does dental infection affect the immune system?
Dental tissue infection and disease result in acute and chronic activation of the innate immune response, which is mediated by molecular and cellular signaling. Different cell types within the dentin-pulp complex are able to detect invading bacteria at all stages of the infection. Indeed, at relatively early disease stages, odontoblasts will respond to bacterial components, and as the disease progresses, core pulpal cells including fibroblasts, stems cells, endothelial cells, and immune cells will become involved. Pattern recognition receptors, such as Toll-like receptors expressed on these cell types, are responsible for detecting bacterial components, and their ligand binding leads to the activation of the nuclear factor-kappa B and p38 mitogen-activated protein (MAP) kinase intracellular signaling cascades. Subsequent nuclear translocation of the transcription factor subunits from these pathways will lead to proinflammatory mediator expression, including increases in cytokines and chemokines, which trigger host cellular defense mechanisms. The complex molecular signaling will result in the recruitment of immune system cells targeted at combating the invading microbes; however, the trafficking and antibacterial activity of these cells can lead to collateral tissue damage. Recent evidence suggests that if inflammation is resolved relatively low levels of proinflammatory mediators may promote tissue repair, whereas if chronic inflammation ensues repair mechanisms become inhibited. Thus, the effects of mediators are temporal context dependent. Although containment and removal of the infection are keys to enable dental tissue repair, it is feasible that the development of anti-inflammatory and immunomodulatory approaches, based on molecular, epigenetic, and photobiomodulatory technologies, may also be beneficial for future endodontic treatments.
What is the innate immune response in dental tissue?
Dental tissue infection and disease result in acute and chronic activation of the innate immune response, which is mediated by molecular and cellular signaling. Different cell types within the dentin-pulp complex are able to detect invading bacteria at all stages of the infection.
Is dental bioengineering a regenerative medicine?
Dentistry has not escaped the exciting new therapeutic advances of regenerative medicine. The accumulating knowledge about dental stem cells, differentiation, and the signaling cascades of tooth development and morphogenesis has enabled the implementation of dental biomimetics. This domain offers novel approaches to oral restoration, such as whole tooth organ bioengineering and targeted regeneration of specific dental and periodontal tissues, including bone, as recently achieved in rodent models in several laboratories. These procedures have resulted in successful growth of a tooth and its periodontium with appropriate functional properties, including vascularisation, innervation and responses to biomechanical forces (1). However, the length of time required to perform tooth bioengineering has hampered the application of these procedures to the clinical setting. Nevertheless, there are several strategies that can be used to regenerate specific parts of the dental-bone complex which have been destroyed by oral disease.
What is tertiary dentin?
Tertiary dentin (including reparative dentin or sclerotic dentin) forms as a reaction to stimulation, including caries, wear and fractures. Tertiary dentin is therefore a mechanism for a tooth to ‘heal’, with new material formation protecting the pulp chamber and ultimately therefore protects the tooth and individual against abscesses and infection. This form of dentine can be easily distinguished on the surface of a tooth, and is much darker in appearance compared to primary dentine. Tertiary dentine will often not be visible on the surface of a tooth, but because it is more dense it can be viewed on a Micro-CT scan of the tooth.
How does tertiary dentine increase?
Clinical studies have researched the properties of tertiary dentine formation, including anatomy in both humans and animal models, usually from an oral health perspective. Genetic changes in animal models can increase tertia ry dentine production. This suggests certain species may have evolved to produce tertiary dentin in response to dietary changes. For example, gorillas may have evolved high rates of tertiary dentin as protection against severe wear, since they consume a lot of tough vegetation.
Why do teeth have a white arrow?
Wear on the surface of a tooth can lead to the exposure of the underlying dentine. When wear is severe tertiary dentine may form to help protect the pulp chamber.
Why do gorillas have dentin?
For example, gorillas may have evolved high rates of tertiary dentin as protection against severe wear, since they consume a lot of tough vegetation.
Which animal has the highest dentin?
Gorillas have a high rate of tertiary dentin formation, with over 90% of worn teeth showing tertiary dentine. Hominins have a much lower rate of tertiary dentin formation, with around 15% of teeth that have dentin exposed through wear showing tertiary dentin formation.
Is dentine darker than primary dentine?
This form of dentine can be easily distinguished on the surface of a tooth, and is much darker in appearance compared to primary dentine. Tertiary dentine will often not be visible on the surface of a tooth, but because it is more dense it can be viewed on a Micro-CT scan of the tooth.

Overview
Types
There are three types of dentin, primary, secondary and tertiary. Secondary dentin is a layer of dentin produced after the root of the tooth is completely formed. Tertiary dentin is created in response to a stimulus, such as a carious attack or wear.
Primary dentin, the most prominent dentin in the tooth, lies between the enamel and the pulp chamber (near dentinoenamel junction). The outer layer closest to enamel is known as mantle d…
Dentinal sclerosis
Dentinal sclerosis or transparent dentin sclerosis of primary dentin is a change in the structure of teeth characterized by calcification of dentinal tubules. It can occur as a result of injury to dentin by caries or abrasion, or as part of the normal aging process.
Development
Prior to enamel formation, dentine formation begins through a process known as dentinogenesis, and this process continues throughout a person's life even after the tooth has fully developed. Events such as tooth decay and tooth wear can also initiate dentine formation.
Dentinogenesis is initiated by the odontoblasts of the pulp. Odontoblasts are specialised cells that lay down an organic matrix known as pre-dentine. This pre-dentine is subsequently mineralised i…
Structure
Unlike enamel, dentin may be demineralized and stained for histological study. Dentin consists of microscopic channels, called dentinal tubules, which radiate outward through the dentin from the pulp to the exterior cementum or enamel border. The dentinal tubules extend from the dentinoenamel junction (DEJ) in the crown area, or dentinocemental junction (DCJ) in the root area, to the outer wall of the pulp. From the outer surface of the dentin to the area nearest the pu…
Animal dentin
Elephant ivory is solid dentin. The structure of the dentinal tubules contributes to both its porosity and its elasticity. Elephant tusks are formed with a thin cap of enamel, which soon wears away, leaving the dentin exposed. Exposed dentin in humans causes the symptom of sensitive teeth. Dentin is best known for its occurrence in teeth, but in early vertebrates, it was an important part of the dermal skeleton that covered most of the body, and it persists today in a few taxa such a…
See also
• Dentinogenesis
• Dentinogenesis imperfecta
• Odontoblast
• Tooth development
External links
• Goldberg M, Smith AJ (January 2004). "Cells and Extracellular Matrices of Dentin and Pulp: A Biological Basis For Repair and Tissue Engineering". Critical Reviews in Oral Biology and Medicine. 15 (1): 13–27. doi:10.1177/154411130401500103. PMID 14761897.
• Miglani S, Aggarwal V, Ahuja B (October 2010). "Dentin hypersensitivity: Recent trends in management". Journal of Conservative Dentistry. 13 (4): 218–24. doi:10.4103/0972-0707.73385. PMC 3010026. PMID 21217949.