A retroperitoneal abscess is a collection of pus in this retroperitoneal space. It can develop due to spread of an infection from adjacent organs or an infection of the blood as is seen with other types of intra-abdominal abscesses ( abscess in the abdomen ).
Where is a retroperitoneal abscess?
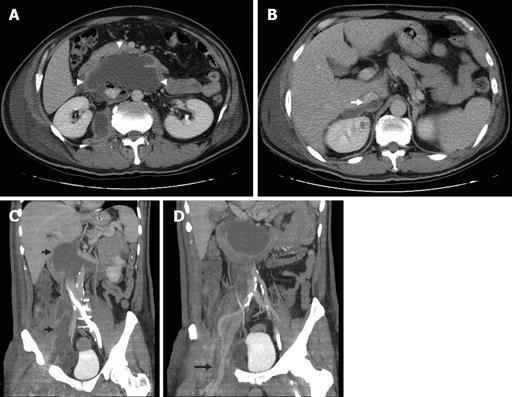
Retroperitoneal abscesses usually locate in the ilio-psoas compartment and can have varied etiologies ranging from acute spinal osteomyelitis, to Crohn disease or hematogenous spread. These abscesses will require CT guidance for drainage because of the deep location.
What is a retroperitoneal infection?
Retroperitoneal infection is a secondary infection caused by inflammation, injury, or perforation of organs adjacent to the retroperitoneum. It spreads easily, is persistent, and is often misdiagnosed. Early diagnosis and active treatment considerably improve its prognosis.
What is the definition of a retroperitoneal abscess?
An abscess located between the peritoneum and the posterior abdominal wall. It may arise from an abscess in the kidney or from the spread of an intraperitoneal infection posteriorly.
What does it mean to be retroperitoneal?
Listen to pronunciation. (REH-troh-PAYR-ih-toh-NEE-ul) Having to do with the area outside or behind the peritoneum (the tissue that lines the abdominal wall and covers most of the organs in the abdomen).
What causes retroperitoneal abscess?
Retroperitoneal abscess (RA) is an uncommon disease that is mainly caused by perinephric inflammation, infections of the gastrointestinal tract, and postoperative complications [1]. Patients usually have comorbidities, such as diabetes mellitus, malignancy, and renal failure.
How do you treat retroperitoneal abscess?
Conclusion: If there is clinical evidence for a retroperitoneal abscess, sonography generally leads to further diagnostic via computed tomography. Small abscesses may be treated by antibiotics alone. Abscesses larger than 3 cm and those not responding to medical treatment should be percutaneously or surgically drained.
What organs are in the retroperitoneum?
The retroperitoneal space is bounded by the posterior parietal peritoneum anteriorly and the lumbar spine posteriorly. The retroperitoneal space contains the kidneys, adrenal glands, pancreas, nerve roots, lymph nodes, abdominal aorta, and inferior vena cava.
Is retroperitoneal mass curable?
For patients with retroperitoneal sarcoma, surgery is still the only chance for cure.
What causes retroperitoneal lymph node swelling?
Retroperitoneal lymph nodes are located in the abdomen. They may become enlarged because of primary or secondary causes. Primary causes include things like infections or cancers that develop in the lymph nodes. Secondary causes include conditions affecting nearby organs like the kidneys or pancreas.
What is the example of retroperitoneal?
The primary retroperitoneal structures are the adrenal glands, kidneys, ureters, inferior vena cava, and the rectum. Secondary retroperitoneal structures include the duodenum (except for the proximal first segment), the pancreas (head, neck and body), ascending colon, and descending colon.
Why kidneys are called retroperitoneal?
The kidneys are considered “retroperitoneal” organs, which means they sit behind a lining in the abdominal cavity, unlike all other abdominal organs.
Which of the following organs is retroperitoneal in location?
The retroperitoneal organs are in the area between the peritoneum and the pericardium. They are located on the back of the abdominal cavity and are attached to it. The retroperitoneal organs include the pancreas, ascending colon, descending colon, and duodenum.
What are the signs and symptoms of a retroperitoneal bleed?
Although spontaneous retroperitoneal hemorrhage is commonly associated with Lenk's triad (acute flank pain, symptoms of internal bleeding, and tenderness to palpation), common signs and symptoms include pain, hematuria, and shock.
What organ is located in the retroperitoneal space?
The retroperitoneal space is bounded by the posterior parietal peritoneum anteriorly and the lumbar spine posteriorly. The retroperitoneal space contains the kidneys, adrenal glands, pancreas, nerve roots, lymph nodes, abdominal aorta, and inferior vena cava.
How long can you live with retroperitoneal fibrosis?
Malignant retroperitoneal fibrosis is associated with poor prognosis, and most patients have an average survival of approximately 3-6 months. Idiopathic retroperitoneal fibrosis carries a good prognosis, with little effect on long-term morbidity or mortality.
Why are kidneys called retroperitoneal?
The kidneys are considered “retroperitoneal” organs, which means they sit behind a lining in the abdominal cavity, unlike all other abdominal organs.
What causes a retroperitoneal abscess?
Other causes of abscesses in the retroperitoneum include traumatic duodenal injury and IPAs.
Where is a retroperitoneal abscess located?
Retroperitoneal Abscess. Retroperitoneal abscesses usually locate in the ilio-psoas compartment and can have varied etiologies ranging from acute spinal osteomyelitis, to Crohn disease or hematogenous spread. These abscesses will require CT guidance for drainage because of the deep location.
Why do you need CT guidance for abscesses?
These abscesses will require CT guidance for drainage because of the deep location. If the abscess involves the psoas muscle in the abdomen and the iliacus in the pelvis, it is often sufficient to place a catheter in the iliacus muscle as there is extensive communications between the iliacus and psoas muscles.
What factors should be considered when deciding the best approach for the management of retroperitoneal abscesses?
These include time since injury, clinical presentation and hemodynamic stability of the patient, as well as concurrent injuries or illnesses.
What is renal abscess?
Renal abscess or infected renal cyst that fails to improve with broad-spectrum antibiotics or a large infected renal or retroperitoneal fluid collection that requires drainage.
What causes an epidural abscess in the lumbar region?
Hematogenous spread from other sites of infection (e.g., skin, soft tissue, bone, respiratory or urinary tract) is the major source of spinal epidural abscess. Direct extension from local osteomyelitis or retropharyngeal, retroperitoneal, or abdominal abscess can also occur. 70a Spinal fracture, 100 penetrating injury, spinal surgery, and local invasive procedure (e.g., lumbar puncture, steroid injection, 101 epidural analgesia 102) have been identified as possible causes. Other mechanisms include: complication of meningitis, fistula in Crohn disease, 103 midline neuroectodermal defects (e.g., dermal sinus), and intradural tumors (e.g., lipoma). In almost one-third of reported cases, the pathogenesis is unknown.
What is the most common site of osteomyelitis in Crohn's disease?
The iliac bone and sacrum are the most frequent sites of osteomyelitis in patients with Crohn's disease. They are almost invariably the result of an adjacent pelvic abscess or enteric fistula. Accordingly, osteomyelitis is usually diagnosed on cross-sectional imaging when the abscess is identified. CT findings in osteomyelitis include cortical bone destruction, intraosseous gas, increased attenuation of the bone marrow, narrowing of the medullary cavity, serpentine drainage tracts, and the presence of an involucrum or sequestrum. On MRI, the marrow space of the involved bone demonstrates decreased signal on T1-weighted images and increased signal on T2-weighted images. Cortical destruction or thickening and edema or abscess formation in the soft tissues can also be demonstrated on MRI.
What is the best treatment for retroperitoneal abscess?
Several factors should be considered when deciding the best approach for the management of retroperitoneal abscesses resulting from duodenal pathology. These include time since injury, clinical presentation and hemodynamic stability of the patient, as well as concurrent injuries or illnesses. Any approach should accomplish drainage of the retroperitoneal abscess cavity and address the primary pathology of the duodenum.34–36 Possible surgical approaches include primary repair and drainage with or without pyloric exclusion versus a more aggressive approach of a pancreaticoduodenectomy. Successful percutaneous drainage also has been reported. 35 Nutritional support is important as enteral feeding will be precluded in the postoperative period. 34,36
What is renal abscess?
Renal abscess or infected renal cyst that fails to improve with broad-spectrum antibiotics or a large infected renal or retroperitoneal fluid collection that requires drainage.
How to treat psoas abscess?
Psoas abscesses are managed by drainage and antibiotic therapy. Except in the case of a known prior infection, empiric antibiotic therapy should cover S. aureus, the most common etiologic agent. Drainage has been accomplished by percutaneous US-guided aspiration or catheter drainage. 46,47 Retroperitoneoscopy and open operative approaches have been used when percutaneous drainage is not successful.
Can percutaneous abscess drainage cure renal abscesses?
Percutaneous abscess drainage can be expected to cure approximately 72% of renal and related retroperitoneal abscesses. This is a significant improvement compared to the results of surgical drainage and is due to the use of cross-sectional imaging techniques for evaluation, which allows the diagnosis of abscesses earlier in their development; needle aspiration to confirm the nature of a fluid collection; and also the efficacy of percutaneous drainage techniques.
What is retroperitoneal abscess?
Retroperitoneal abscess is an unusual type of abscess in surgical practice. It is often underdiagnosed due to the insidious onset of symptoms and its location in the retroperitoneal space making it hard to be assessed via the regular abdominal examination. It is most often due to Genitourinary infection ( Pyelonephritis) or gastrointestinal cause (i.e Inflammatory Bowel Syndrome ). CT & MRI are the cornerstones for diagnosis . Treatment is usually focused on surgical drainage either through open or percutaneous approaches usually accompanied with the use of IV antibiotics .
When was retroperitoneal abscess first described?
Retroperitoneal abscess was first described by Grassi and Serge in 1887.
What happens if you get an abscess and it shrinks?
If the body defenses are successful in eliminating the infection, the granulation tissue continues to grow and the abscess continues to shrink in size until it is only a scar.
What are the risk factors for a retroperitoneal abscess?
Any condition compromising the immune system is a risk factor for developing retroperitoneal abscess. The following were the risk factors in observed patients.
Why is abdominal pain not localized?
Abdominal pain : Not localized due to the unusual site of the abscess.
Is a retroperitoneal abscess secondary or primary?
A retroperitoneal abscess is usually secondary to spread from other primary site either through hematogenous or by contiguous spread.
Can a septic focus cause a retroperitoneal abscess?
Any septic focus can theoretically lead to retroperitoneal abscess. These are the primary foci in order of frequency of causing retroperitoneal abscess.
What is a spontaneous retroperitoneal abscess?
Spontaneous retroperitoneal abscess as the first clinical manifestation of a non-functioning retroperitoneal paraganglioma.
Where is the retroperitoneal abscess located?
retroperitoneal abscess. An abscess located between the peritoneum and the posterior abdominal wall. It may arise from an abscess in the kidney or from the spread of an intraperitoneal infection posteriorly. See also: abscess. Medical Dictionary, © 2009 Farlex and Partners.
What is the term for inflammation of the retroperitoneum?
Retroperitoneal inflammation is also known as retroperitonitis.
What causes retroperitoneal inflammation?
Retroperitoneal inflammation can happen when harmful bacteria come in contact with the organs in the retroperitoneal space or the lining that encloses your abdominal cavity . Possible causes of retroperitoneal inflammation include:
What is the space between the intestines and the back?
In less complicated terms, it’s the space in your abdomen between your abdominal cavity (the area where your intestines are) and your back. It houses several major organs, including: kidneys. bladder. abdominal aorta. adrenal glands. Inflammation often happens in response to an infection.
What tests are done to check for retroperitoneal space?
Your doctor will assess your symptoms. Then they will typically order an ultrasound, abdominal X-ray, CT scan, or MRI. These imaging tests will help reveal any abnormalities in the retroperitoneal space. This will allow your doctor to assess your condition.
How do antibiotics help with infection?
Antibiotics can help prevent inflammation caused by infection . The type of antibiotic prescribed and the length of your treatment will depend on the severity of the infection and the suspected bacteria.
What can cause bacteria to enter the retroperitoneal space?
A ruptured appendix, stomach ulcers, or a perforated colon can allow bacteria into your retroperitoneal space .
Is retroperitoneal space a serious condition?
It has a high mortality rate. However, early diagnosis and treatment can improve your outlook. The retroperitoneal space is the space between your peritoneum and your posterior abdominal wall.
Overview
Historical Perspective
- Retroperitoneal abscess was first described by Grassi and Serge in 1887.
- Dr. Hugh Cabbot presented the first case of retroperitoneal abscess in a case report in 1922.
Classification
- Retroperitoneal abscess may be classified according to the location in the retroperitoneal space into 5 categories : 1. Perinephricabscess 2. Upper retroperitonealabscess 3. Pelvicabscess 4. Combined retroperitoneal and pelvicabscess 5. Lٍٍocalized musculoskeletalabscess
Pathophysiology
- Pathogenesis
1. A retroperitoneal abscess is usually secondary to spread from other primary site either through hematogenous or by contiguous spread. 2. The bacteria causing the abscess depends on the primary site. When the bacteria invades the retroperitoneal tissue, toxins released from it destro… - Microscopic findings
1. The Abscess consists of a mixture of inflammatory cellstogether with debris tissue. 2. From the surrounding wall grows some capillaries to form granulation tissue. 3. If the body defenses are successful in eliminating the infection, the granulation tissue continues to grow and the absces…
Causes
- Retroperitoneal Abscess may be caused by : 1. E. Coli or Proteus spp (if the primary site is the urinary tract) 2. Multibacterial & anaerobes(if gastrointestinal tract (GIT) is the primary source) 3. Staphylococcus aureus (if from distant septic focus) 4. Tuberculosis (if secondary to Pott’s disease)
Epidemiology and Demographics
- Retroperitoneal abscess is far less common than intraperitoneal abscesses. 1. Males are slightly more susceptible than females. 2. Increased incidence between third and sixth decades. 3. Most common cause in developing countries is spread from distant septic focus. 4. Most common causes in developed countries are Renal and GIcauses.
Risk Factors
- Any septic focus can theoretically lead to retroperitoneal abscess. These are the primary foci in order of frequency of causing retroperitoneal abscess. 1. Renalinfections: 1. Spread from the urinary tract is the most common cause. 1. Gastrointestinaldiseases: 1. Spread from the gastrointestinal tract is the second common cause (e.g. perforated appendix, perforated colon c…
Natural History, Complications and Prognosis
- Natural history
If left untreated, retroperitoneal abscess may cause septicemia with very high incidence of morbidity and mortality. - Complications :
Most complications result from septicemiawhich presents late in the disease. 1. Pneumonia and respiratory failure type 1 is the most common complication with very high mortality. 2. Recurrent Abscessafter drainage. 3. Renal Failure 4. DVT 5. Small Bowel Obstruction 6. Arterial Thrombosi…
Diagnosis
- History
1. A detailed history should be obtained from the patient presenting with insidious onset of abdominal pain. 2. Common causes should be investigated (Kidney and gastrointestinal diseases) especially in the presence of any of the risk factors (e.g. DM and corticosteroidadministration). - Symptoms [1]:
Given that the presentation is usually insidious, nonspecific beside that it’s an unusual condition .. the diagnosis is usually delayed.
Physical Exam
- General Appearance
The patient is usually fatigued & looking ill due to the preexisting risk factor. In advanced cases with septicemia, the patient may be drowsy with decreased level of consciousness. - Vital signs
1. Fever 2. Tachycardia 3. Tachypnea 4. Hypotension (if patient is presenting with shock)