What is Stage 3 twin to twin transfusion syndrome? Stage 3: The imbalance of blood flow starts to affect the heart function in one or both babies. This is seen in abnormal blood flow in the umbilical cords or hearts of the twins.
What are the stages of TTTS in twins?
The Stages of TTTS. Stage 3: The imbalance of blood flow starts to affect the heart function in one or both babies. This is seen in abnormal blood flow in the umbilical cords or hearts of the twins. Stage 4: The imbalance of blood flow causes signs of heart failure in one of the twins.
What is twin-twin transfusion syndrome?
What is twin-twin transfusion syndrome (TTTS) Twin-twin transfusion syndrome (also called TTTS or twin to twin transfusion syndrome) is a condition in which the blood flows unequally between twins that share a placenta (monochorionic twins). TTTS occurs in about 10 to 15 percent of monochorionic, diamniotic (two amniotic sacs) twins.
What are the abnormal blood flow patterns in Stage 3 TTTS?
In stage 3 TTTS, abnormal blood flow patterns include reversed flow in ductus venosus (DV), and absent/reversed umbilical artery end-diastolic velocity (UAEDV). Abnormal dopplers (blood flow patterns) indicate the heart function of one or both twins is affected.
What are the signs of heart failure in twins with TTTS?
Evidence of overt heart failure in either twin. Each baby has circulatory problems as TTTS progresses. On the left, the donor has severe placental resistance and very low blood flow to the placenta. On the right, the recipient is struggling with heart failure, with blood running backward during the cardiac cycle. Intrauterine death of either twin.

What is the survival rate of twin to twin transfusion?
The majority of TTTS twins who have appropriate treatment during pregnancy will survive and the majority of survivors will be normal and healthy. If untreated, the survival rate for TTTS twins is approximately 10 to 15 percent. Once TTTS babies are born, blood supply sharing is no longer a factor.
What are the stages of TTS?
Stage I: One baby has too much fluid and the other baby does not have enough fluid. Stage II: Cannot see the bladder fill in the donor fetus on ultrasound. Stage III: Abnormal blood flow through the umbilical cord or fetal vessels around the heart for one or both babies. Stage V: The death of one or both babies.
What type of twins have twin to twin transfusion?
Twin to twin transfusion syndrome (TTTS) is a condition that occurs only in monochorionic pregnancies — ones in which two or more genetically identical babies (usually twins) share the same placenta. Although all identical twins share a placenta, TTTS develops in about 10 to 15 percent of those pregnancies.
What is TTTS 3?
Stage 3. In stage 3 TTTS, abnormal blood flow patterns include reversed flow in ductus venosus (DV), and absent/reversed umbilical artery end-diastolic velocity (UAEDV). Abnormal dopplers (blood flow patterns) indicate the heart function of one or both twins is affected.
How fast does TTTS progress?
Results: Among 132 consecutive cases of TTTS, 46 women presented with Stage I disease. In the majority (69.6%), disease remained stable (28.3%) or regressed (41.3%). Of cases that progressed, 79% did so within 2 weeks and 93% progressed to at least Stage III.
How successful is TTTS surgery?
Abstract. Purpose: Severe, progressive twin-to-twin transfusion syndrome (TTTS) is associated with near-100% mortality if left untreated. Endoscopic laser ablation of placental vessels (ELA) is associated with 75% to 80% survival of at least one twin.
Can both twins survive TTTS?
In most instances, the appropriate, optimal therapy will be fetoscopic laser intervention. Our center was one of the first in the world to perform fetoscopic laser to treat TTTS. Survival rates for at least one twin are greater than 85% and for both twins is approximately 60% at our center.
Is TTTS genetic?
The common placenta may also be shared unequally by the twins. The events in pregnancy that lead to TTTS are all random. TTTS is not hereditary or genetic, nor caused by anything the parents did or did not do.
What are the symptoms of twin-to-twin transfusion syndrome?
What are the signs of TTTS?A uterus that measures large for her stage of pregnancy.Feeling like her abdomen is growing or expanding rapidly.A sudden increase in body weight.Increased abdominal pressure or pain.Shortness of breath.Uterine cramping or contractions.Swelling of the hands and legs early in the pregnancy.
What causes twin-to-twin transfusion syndrome?
Twin-to-twin transfusion syndrome (TTTS) is a rare pregnancy condition affecting identical twins or other multiples. TTTS occurs in pregnancies where twins share one placenta (afterbirth) and a network of blood vessels that supply oxygen and nutrients essential for development in the womb.
How long does TTTS surgery take?
Laser photocoagulation is an in utero surgical treatment for TTTS. The surgery is done in an operating room using spinal anesthesia, and typically takes 30-to-60 minutes. The procedure involves placing a very thin camera, called a fetoscope, into the uterus through a tiny 2-3mm incision in the skin.
How does the death of a twin affect the other twin?
Twins literally do not know how to exist as one. When a twin dies, the twinless twin longs to reconnect. The twinless twin may have phantom pain or feel half dead. He or she may feel a need to represent both him or herself and the deceased twin or may even take on behaviors of the deceased twin.
What is TTS model?
Text-to-Speech (TTS) is the task of generating natural sounding speech given text input. TTS models can be extended to have a single model that generates speech for multiple speakers and multiple languages.
What is text-to-speech used for?
Text-to-speech (TTS) is a type of assistive technology that reads digital text aloud. It's sometimes called “read aloud” technology. TTS can take words on a computer or other digital device and convert them into audio.
When does twin to twin transfusion syndrome develop?
It usually develops between weeks 16 and 26 of pregnancy and can be easily detected with ultrasound.
What causes twin-to-twin transfusion syndrome?
There is no known genetic or other cause of twin-to-twin transfusion syndrome.
How does laser fetoscopy cure twin-to-twin transfusion syndrome?
Laser fetoscopy (selective laser photocoagulation) is the preferred method of treatment for TTTS. Yale New Haven Hospital is one of only 30 to 40 hospitals in the United States offering the procedure. Laser fetoscopy can be safely done up until 26 weeks of gestation.
Does Yale Medicine offer unique advantages in the treatment of twin-to-twin transfusion syndrome?
We receive referrals from around the Northeast for TTTS and are the only center in the state offering laser fetoscopy treatment.
What is TTTS in pregnancy?
TTTS is a rare, in utero condition that occurs only in monochorionic twins (identical twins who share the same placenta). Attached to the inside of the uterus during pregnancy and connected to the fetus by the umbilical cord, the placenta delivers nutrients and oxygen from the mother’s blood to the developing babies.
How to diagnose TTTS?
TTTS is diagnosed by measuring levels of amniotic fluid. If one twin has a high level of amniotic fluid in the amniotic sac and the other twin has a low level, it will be visible via ultrasound.
What is stage 1 amniotic fluid?
Stage I: There is an imbalance in amniotic fluid between the twins.
What is Twin-to-Twin Transfusion Syndrome?
Twin-to-twin transfusion syndrome (TTTS) is a rare pregnancy condition affecting identical twins or other multiples. TTTS occurs in pregnancies where twins share one placenta (afterbirth) and a network of blood vessels that supply oxygen and nutrients essential for development in the womb. These pregnancies are known as monochorionic.
What happens to a donor twin?
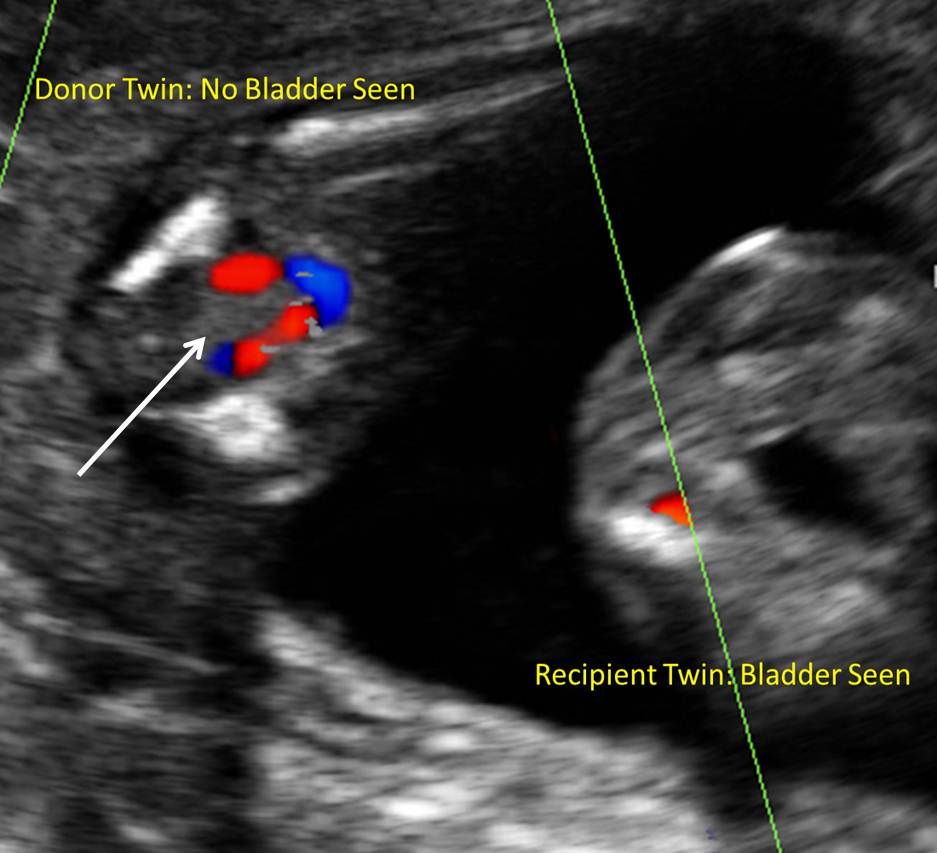
The donor twin. The donor twin experiences progressive loss of blood volume ( hypovolemia ). Therefore, its kidneys don’t have to filter as much fluid from the blood, and as a result, urination decreases. This affects development of the bladder and leads to low levels of amniotic fluid. Amniotic fluid, which consists of fetal urine, ...
What is the Quintero staging system?
Doctors can assess the severity of each case of TTTS using the Quintero staging system. Quintero stages I and II represent progressive stages of blood volume imbalance, while stages III and IV indicate progressive stages of cardiovascular dysfunction. Stage V refers to the death of one or both twins. Quintero staging is important because it provides a standardized prenatal estimate on disease severity and the likelihood the condition will worsen.
What is the prognosis of TTTS?
An important factor in determining the prognosis of TTTS is the state of cardiovascular dysfunction in the twins. This is why a diagnosis of TTTS will include a detailed examination of the fetal heart (fetal echocardiography) in both the recipient and donor.
What is the risk of twins urinating?
The recipient twin. The recipient twin is at risk for successively increasing blood volume ( hypervolemia ). Hypervolemia leads to increased urination, more frequent bladder filling and the production of larger amounts of urine every time the bladder is emptied.
Why do twins give away more blood than they receive?
One twin — the donor twin — gives away more blood than it receives in return and runs the risk of malnourishment and organ failure. The recipient twin receives too much blood and is susceptible to overwork of the heart and other cardiac complications.
Can you get pregnant with identical twins?
However, TTTS is an indiscriminate condition, occurring at random in monochorionic pregnancies.
What happens to a baby with TTTS?
Each baby has circulatory problems as TTTS progresses. On the left, the donor has severe placental resistance and very low blood flow to the placenta. On the right, the recipient is struggling with heart failure, with blood running backward during the cardiac cycle.
What is the phone number for TTTS?
Call for appointment: 410-328-3865. 410 -328-3865. You may encounter several definitions of TTTS. Many of these concepts are based on the pediatric literature - in other words, they are based on the rare survivors of untreated TTTS. We now understand that babies reported this way have the mildest or shortest forms of TTTS.
Who proposed the staging system?
In 1997, Dr. Ruben Quintero proposed a system based on ultrasound findings which made assessment much clearer. The use of this staging system has led to general agreement on the condition of the babies before treatment is started, making it possible for us to compare modern management options objectively.
What is TTTS in pregnancy?
Listen. Twin to twin transfusion syndrome (TTTS) is a rare condition that occurs during a twin pregnancy when blood moves from one twin (the “donor twin”) to the other (the “recipient twin”) while in the womb. [1] . TTTS is a complication that specifically occurs in identical (monozygotic) twin pregnancies that share the same "egg" sac ...
What is the treatment for a twin after birth?
The donor twin may need a blood transfusion to treat anemia. The recipient twin may need to have the volume of body fluid reduced. This may involve an exchange transfusion. Medications may be given to treat heart failure in the recipient twin.
When does TTTS occur?
TTTS is a complication that specifically occurs in identical (monozygotic) twin pregnancies that share the same "egg" sac (monochorionic) that may or may not share the same amniotic sac (monoamniotic). [2] . TTTS usually develops between 15 and 26 weeks of pregnancy. [3] . The donor twin may be born smaller, with paleness, anemia, and dehydration.
What is the most important step in evaluating a twin pregnancy for twin-twin transfusion syndrome?
Fetal ultrasound showing TTTS The most important step in evaluating a twin pregnancy for twin-twin transfusion syndrome is to determine whether the twins share a single placenta. An ultrasound examination early in pregnancy (during the first trimester) can best make this distinction.
What happens when there is unequal blood flow between twins?
In TTTS, unequal blood flow between twins sharing a placenta results in recipient twin (right) having too much amniotic fluid, and donor twin with no surrounding amniotic fluid. In twin-twin transfusion syndrome, there is an unequal sharing of blood that passes between twins through blood vessel connections on the surface of the placenta. One twin (called the donor twin) pumps blood to the other twin (called the recipient). This causes the recipient twin to receive too much blood and the donor twin to receive too little.
What are the features of TTTS?
Other features of TTTS include twins of the same gender, a difference in size between the twins, and a difference in the volume of amniotic fluid surrounding the two fetuses. A detailed sonographic assessment rules out any additional structural anomalies. A 3D fetal ultrasound shows twins with TTTS Twin-twin transfusion syndrome can also have ...
How to evaluate twins?
Your evaluation will involve the following exams: 1 High-resolution ultrasound – An examination to rule out structural abnormalities in the twins. This exam will also confirm placental location and umbilical cord insertions into the placenta, assess amniotic fluid levels in each sac and assess blood flow patterns in specific blood vessels for each twin. 2 Fetal echocardiogram – A focused ultrasound of each twin’s heart to look for any related heart conditions. Twin-twin transfusion syndrome may cause serious cardiac strain in the recipient twin, resulting in enlargement of the heart and cardiac dysfunction. All twins evaluated for TTTS should undergo a fetal echocardiogram. Fetal cardiology experts from CHOP’s Fetal Heart Program have developed a cardiac scoring tool to determine how severe the condition has become for the twins. This score helps the medical team determine need for treatment. (See “ The twin-twin transfusion syndrome: Spectrum of cardiovascular abnormality and development of a cardiovascular score to assess severity of disease .”) 3 Genetic amniocentesis – A procedure in which a small amount of amniotic fluid is removed from the sacs surrounding the fetuses and tested. In some cases, this genetic test may be needed if imaging studies identify structural malformations in addition to TTTS.
How long after fetal intervention do you have to have an ultrasound?
We will schedule you for an ultrasound exam at our Center one week after your procedure to re-evaluate the health of your twins.
What are the symptoms of a TTTS?
In TTTS, the increased volume of blood causes the recipient twin to produce more than the usual amount of urine, which can result in a large bladder, too much amniotic fluid (known as polyhydramnios) and hydrops, a prenatal form of heart failure. The donor twin, who receives too little blood, produces less than the usual amount ...
What is the name of the twin that pumps blood to the other twin?
One twin (called the donor twin) pumps blood to the other twin (called the recipient). This causes the recipient twin to receive too much blood and the donor twin to receive too little. There are no known genetic causes of TTTS.
How is twin to twin transfusion syndrome (TTTS) managed before birth?
Our prenatal management of babies with TTTS centers on monitoring the babies frequently with high-resolution fetal ultrasonography and fetal echocardiography. This testing allows us to measure the amount of amniotic fluid around your babies. It also allows us to assess how well blood is flowing within your babies’ umbilical cords, as well as within other blood vessels.
What is a twin to twin transfusion?
Twin to twin transfusion syndrome (TTTS) is a condition that occurs only in monochorionic pregnancies — ones in which two or more genetically identical babies (usually twins) share the same placenta. Although all identical twins share a placenta, TTTS develops in about 10 to 15 percent of those pregnancies. The condition does not occur ...
How many babies survive fetoscopic photocoagulation?
That percentage is dramatically improved for babies who undergo fetoscopic laser photocoagulation. In almost 90 percent of those pregnancies, at least one baby will survive and be healthy after leaving the hospital NICU. Having both twins survive advanced TTTS remains a challenge, however.
How is twin to twin transfusion syndrome diagnosed?
How is twin to twin transfusion syndrome (TTTS) diagnosed? A twin to twin transfusion syndrome diagnosis is confirmed by ultrasound. The condition becomes evident when the ultrasound images show that one child has extra amniotic fluid and the other child has significantly decreased amounts.
What is the staging system for TTTS?
When TTTS is diagnosed, a staging system is used to classify the severity of the condition. This system — known as the Quintero staging system — helps to determine whether an intervention is needed and which treatment option (s) might be most appropriate. Here is an explanation of twin to twin transfusion syndrome stages:
What happens when a baby donates blood to another baby?
But in cases of TTTS, the flow of blood becomes unbalanced, and one baby will actually donate blood to the other. When this happens, the baby donating the blood (the “donor” twin) becomes dehydrated and stops making urine. This results in a decrease in amniotic fluid, the protective liquid that surrounds the baby in the womb.
Can twin to twin transfusion be delivered?
Delivery: If TTTS is discovered later in the pregnancy, delivery of the babies may be the best option.
How to help a pregnant woman with twin to twin transfusion syndrome?
Family and friends can be a very important source of comfort and strength during a pregnancy diagnosed with twin to twin transfusion syndrome. It is often difficult, however, to have time to devote yourself to explaining the disease to them. If you would like a packet mailed to anyone in your family, for example, the babies’ grandparents or close friends, please call, or have them call the Foundation at 440-899-8887 and we will mail this to them and talk with them on the phone. If you are in the hospital, you may also call toll-free at 800-815-9211.
What happens if you transfuse blood from one twin to another?
Depending on the number, type and direction of the connecting vessels, blood can be transfused disproportionately from one twin (the donor) to the other twin (the recipient). The transfusion causes the donor twin to have decreased blood volume. This in turn leads to slower than normal growth than its co-twin, and poor urinary output causing little to no amniotic fluid or oligohydramnios (the source of most of the amniotic fluid is urine from the baby). The recipient twin becomes overloaded with blood. This excess blood puts a strain on this baby’s heart to the point that it may develop heart failure, and also causes this baby to have too much amniotic fluid (polyhydramnios) from a greater than normal production of urine.
What is TTTS?
Twin to twin transfusion syndrome (TTTS) is a disease of the placenta (or afterbirth) that affects identical twin pregnancies. TTTS affects identical twins (or higher multiple gestations), who share a common monochorionic placenta. The shared placenta contains abnormal blood vessels, which connect the umbilical cords and circulations of the twins.
How Often Does TTTS Occur?
Based on 2005, similar to 2018, USA National Center for Health Statistics (4,138,349 total births), the rate of multiple births per year is now 1:30 (3.4%), or approximately 139,816 twins or higher multiples.
Why are twins different sizes on ultrasound?
The twin’s size difference may be due to either the transfusion of nutrients or unequal sharing of the common placenta or both.
Why is my twin's bladder full on ultrasound?
The twin’s size difference may be due to either the transfusion of nutrients or unequal sharing of the common placenta or both. Degree of Discordance in Amniotic Fluid: The recipient may have quarts of excess amniotic fluid (polyhydramnios) and its bladder always appears full on ultrasound scan.
What happens if a twin gets overloaded with blood?
The recipient twin becomes overloaded with blood. This excess blood puts a strain on this baby’s heart to the point that it may develop heart failure, and also causes this baby to have too much amniotic fluid (polyhydramnios) from a greater than normal production of urine.