Is Surfactant therapy effective in the treatment of neonatal respiratory distress syndrome?
Exogenous surfactant therapy has an established role in the management of neonatal respiratory distress syndrome (RDS). This article summarises the current evidence on surfactant therapy. The use of surfactant for the treatment or prophylaxis of neonatal RDS results in a 30% to 65% relative reductio …
How do you administer surfactant to a newborn?
Surfactant therapy is given by inserting a tube into the trachea of respiratory tract. (endotracheal intubation). The baby is monitored while giving surfactant. This helps to understand the heart rate, respiratory rate and oxygen level of the baby.
What happens if you delay Surfactant therapy for newborns?
If surfactant therapy is given as early as possible, the surfactant spreads with that substance to almost the entire lungs, thus reducing the tension on the surface of the respiratory tract. Delaying surfactant therapy for baby can damage his/her lungs and cause inflammatory substances to build up in the lungs.
When is surfactant indicated in the treatment of intubated infants?
b.1 For infants intubated immediately after birth, it is recommended that surfactant be given as early treatment (<2 h of age), except if the infant is on room air and minimal ventilatory support on neonatal intensive care unit admission.
What does surfactant therapy do?
Many clinical trials have demonstrated that surfactant replacement therapy is a safe, effective and beneficial treatment as it significantly reduces respiratory morbidity (air leaks, pulmonary interstitial emphysema), ventilatory requirements and mortality in these neonates.
Why do newborns need surfactant?
Surfactant coats the alveoli (the air sacs in the lungs where oxygen enters the body). This prevents the alveoli from sticking together when your baby exhales (breathes out).
When should surfactant be given?
Sick newborn infants with pneumonia and an oxygenation index greater than 15 should receive exogenous surfactant therapy (grade C). Intubated newborn infants with pulmonary hemorrhage which leads to clinical deterioration should receive exogenous surfactant therapy as one aspect of clinical care (grade C).
What are the side effects of surfactant therapy?
Side effects of lung surfactants may include the following:Cyanosis (bluish skin coloration due to low oxygen)Airway obstruction.Bradycardia (slow heartbeat)Endotracheal tube reflux.Endotracheal tube blockage.Oxygen desaturation.Requirement for manual ventilation.Reintubation.More items...
How long does it take for baby lungs to develop?
The rate of lung development can vary greatly, and the lungs are among the last organs to fully develop – usually around 37 weeks. From fluid to air: While in the womb, lungs are filled with fluid and oxygen is supplied through the umbilical cord.
What causes lung problems in newborns?
Neonatal RDS occurs in infants whose lungs have not yet fully developed. The disease is mainly caused by a lack of a slippery substance in the lungs called surfactant. This substance helps the lungs fill with air and keeps the air sacs from deflating.
How many days after birth can you give surfactant?
Optimal timeframe for surfactant administration: a. The optimal time for rescue surfactant administration is within 2 to 6 hours of birth. b. In general, the literature does not support giving a first dose of surfactant past about 24 hours of life.
How much does surfactant cost?
Infants in the prophylactic trial were not eligible for the rescue trial. Results: For the rescue trial, there was a $16,600 reduction in average hospital costs (p = 0.18), which was larger than the cost of the surfactant ($450 to $900), yielding a probable net savings.
What are three signs of respiratory distress in the newborn?
Babies who have RDS may show these signs:Fast breathing very soon after birth.Grunting “ugh” sound with each breath.Changes in color of lips, fingers and toes.Widening (flaring) of the nostrils with each breath.Chest retractions - skin over the breastbone and ribs pulls in during breathing.
What is surfactant in simple words?
surfactant, also called surface-active agent, substance such as a detergent that, when added to a liquid, reduces its surface tension, thereby increasing its spreading and wetting properties.
What do they give premature babies for their lungs?
When premature lungs are treated with surfactant after birth, the infant's blood oxygen levels usually improve within minutes. Surfactant treatment reduces the risk and the severity of respiratory distress syndrome (RDS) in premature infants. It also reduces the overall risk of death. Surfactant also helps treat RDS.
What is surfactant example?
Sodium stearate is a good example of a surfactant. It is the most common surfactant in soap. Another common surfactant is 4-(5-dodecyl)benzenesulfonate. Other examples include docusate (dioctyl sodium sulfosuccinate), alkyl ether phosphates, benzalkaonium chloride (BAC), and perfluorooctanesulfonate (PFOS).
Why is surfactant important in the lungs?
Surfactant is released from the lung cells and spreads across the tissue that surrounds alveoli. This substance lowers surface tension, which keeps the alveoli from collapsing after exhalation and makes breathing easy.
Which action best explains the main role of surfactant in the neonate?
Which action best explains the main role of surfactant in the neonate? Surfactant works by reducing surface tension in the lung.
Why the lack of surfactant would result in respiratory distress?
Surfactant enables the lungs to expand more easily. Without surfactant, the air sacs in the lungs, also called alveoli, collapse very easily. This collapse leads to decreased amounts of air in the lungs. The lack of surfactant combined with alveolar collapse makes it very difficult for the infant to breathe.
When do babies start producing surfactant?
A baby normally begins producing surfactant sometime between weeks 24 and 28 of pregnancy. Most babies produce enough to breathe normally by week 34. If your baby is born prematurely, they may not have enough surfactant in their lungs. Occasionally, NRDS affects babies that are not born prematurely.
What is surfactant therapy?
Therapy with active instilled surfactant drugs leads to improved respiration (oxygenation, ventilator requirements) and significantly increased survival in preterm infants. Surfactant therapy is also associated with a decreased risk of pneumothorax, pulmonary interstitial emphysema, and bronchopulmonary dysplasia.
Why is surfactant therapy used for RDS?
Surfactant therapy was developed for RDS because of the understanding that surfactant deficiency was the cardinal element of lung immaturity that limited lung function. However, it was recognized that surfactant function could be inhibited by proteinaceous pulmonary edema and other products of lung injury and result in a secondary surfactant deficiency type syndrome ( 61 ). Surfactant treatment improves lung function in multiple experimental models of lung injury. Other than injury caused by mechanical ventilation, the common lung injury syndromes in infants are meconium aspiration syndrome, bronchopulmonary dysplasia and sepsis/pneumonia. As already illustrated in this chapter, lung injury caused by mechanical ventilation results in a less favorable response to surfactant treatment than treatment of the uninjured preterm lung ( 30) ( Fig. 4-8 ). Surfactant abnormalities in the other lung injury syndromes in newborns have two explanations: inhibition of surfactant function and/or altered surfactant metabolism. Either abnormality might be improved by surfactant treatment.
Is surfactant good for RDS?
Exogenous surfactant therapy has been a significant advance in the management of preterm infants with RDS and has become established as a standard part of the management of such infants. Both natural and synthetic surfactants lead to clinical improvement and decreased mortality, with natural surfactants having additional advantages over synthetic surfactants. The use of prophylactic surfactant, administered after initial stabilization at birth, in infants at risk for RDS has benefits over “rescue” surfactant given to treat infants with established RDS. In infants who do not receive prophylaxis, earlier treatment (before 2 hours) has benefits over later treatment. The use of multiple doses of surfactant is a strategy to the use of a single dose, and the use of a higher threshold for re-treatment appears to be as effective as a low threshold. Adverse effects of surfactant therapy are infrequent and usually not serious. Long-term follow-up of infants treated with surfactant in the neonatal period is reassuring. In the future we likely will see the development of new types of surfactants, and further research is required on the optimal use of surfactant in conjunction with other respiratory interventions.
Can surfactant therapy be used for respiratory failure?
Exogenous surfactant therapy as adjunctive treatment for near-term and term neonates with severe hypoxemic respiratory failure has been studied in RCT and has shown promise. There is evidence for surfactant deficiency in some patients with PPHN (240, 241 ). Studies have shown that surfactant therapy is associated with sustained clinical improvement in term infants with pneumonia and meconium aspiration syndrome ( 242 ), and can reduce the duration of ECMO ( 243 ). A multicenter, randomized, double-blind, placebo-controlled trial studied the role of surfactant treatment in term neonates with severe respiratory failure ( 220 ). Infants of 36 weeks or greater were randomly assigned to receive four doses of surfactant (beractant) or air placebo before ECMO treatment, if required. They found that the need for ECMO therapy was significantly less in the surfactant group than in the placebo group; this effect was greatest for infants within the lowest OI stratum – 15–22 ( 220 ).
Can surfactants be used to deliver steroids?
In the future, surfactants may have the potential to be used more extensively to deliver other drugs such as steroids directly to the lungs. A study from Taiwan randomly allocated 116 babies with severe RDS to either standard surfactant therapy with beractant or therapy with beractant mixed with an additional 0.25 mg/kg of budesonide. 120 The babies in the budesonide group had a lower incidence of the combined outcome of death or BPD (19 of 60 vs. 34 of 56) although the babies in budesonide group were less sick to start with. 120 Follow-up did not show a higher incidence of long-term adverse effects in babies treated with topical steroids in this way. 121 A large multicenter trial of this promising new therapy is under way.
Can surfactant be used for premature babies?
Surfactant therapy remains the cornerstone of successful management of premature babies with RDS. In the first decade of this century, the trend initially had been to move to earlier administration of surfactant, with many neonatal units developing protocols for delivery room prophylaxis for the majority of extremely preterm babies. In the light of evidence that this approach may be unnecessary and potentially even harmful, it is likely that in the near future we will see clinicians becoming increasingly comfortable with initiation of early CPAP ventilation in the delivery room for even the smallest infants and reserving intubation and immediate surfactant application for those in whom RDS develops. It is likely that clinicians will continue to work toward methods of delivering surfactant without causing lung injury.
Can surfactant therapy be used for lung function?
Clinical studies have shown that exogenous surfactant therapy is efficacious in term infants with meconium aspiration or pneumonia, and also can improve lung function and outcomes in children with ALI/ARDS. Surfactant therapy in adults with ARDS has had less success.
What is a surfactant for neonates?
A more viscous liquid yields a more homogeneous distribution, and a less viscous plug penetrates more deeply into the distal airways. There are several surfactant preparations available for use in neonates. A natural bovine lipid extract surfactant is used in the majority of Canadian neonatal units. The biochemical composition of each preparation generally reflects the composition of natural surfactant obtained from the alveolar spaces, at least with respect to the high content of phospholipids and the high proportion of disaturated dipalmitoyl phosphatidylcholine (DPPC). The production procedure should also, in principle, preserve the hydrophobic proteins SP-B and SP-C. Surfactants produced from bronchoalveolar lavage are, in principle, less contaminated with plasmatic and tissue components: bovactant, calfactant, bovine lipid extract surfactant, and a biological product produced from pig lungs in Cuba. Poractant alfa and beractant are examples of surfactant obtained from minced lungs. The resulting proportion of the main surface-active lipid component, DPPC, varies from 70% in beractant, 40% in calfactant, approximately 35% to 56% in poractant alfa, 41% in the bovine lipid extract surfactant and 45% in the biological product produced from pig lungs in Cuba.
When should surfactant be given?
b.1 For infants intubated immediately after birth, it is recommended that surfactant be given as early treatment (<2 h of age), except if the infant is on room air and minimal ventilatory support on neonatal intensive care unit admission.
How does viscosity affect surfactant?
Commercial surfactants also differ in surface viscosity. Viscosity is believed to influence the rate, extent and uniformity of distribution of surfactant in the lungs. Preparations with lower surface viscosity are preferred for endotracheal application because it allows a more uniform and rapid distribution of the instilled surfactant with less loss due to coating of the upper airways. The viscosity of surfactant preparations is directly dependent on phospholipid concentration and inversely related to temperature. After 15 min at a temperature of 37°C, viscosity increases exponentially. In fact, after 30 min at this temperature, the viscosity of calfactant and beractant were 20 times higher when compared with values measured at 10 min (17). In an animal experiment, Lewis et al (18) compared beractant and a bovine lipid extract surfactant. A significantly improved distribution was achieved with the bovine lipid extract surfactant, which was demonstrated to have a viscosity eight times lower than beractant.
How does breathing affect surfactant distribution?
Anderson et al (15) investigated the effects of breathing frequency on liquid distribution. At 60 breaths/min, the liquid is first deposited on the airway walls and then transmitted toward the gravity-dependent region of the lung over the ensuing breaths. A more uniform distribution of liquid throughout the lung was obtained. This phase lasted only a few minutes and facilitated the transport of liquid to its target location. After this initial targeted instillation is achieved, normal ventilation using appropriate ventilation rate can be used. The implication for surfactant delivery is that a slow rate of ventilation could result in nonhomogeneous surfactant distribution. This is not the desired outcome because it may inflate parts of the lung receiving surfactant, resulting in lung injury.
How does liquid instillation affect the distribution of surfactant?
Cassidy et al (7) showed that the method of liquid instillation affects how the liquid distributes within the lung. The best method allowed the formation of a liquid plug in the trachea at the beginning of surfactant instillation. The liquid was then driven to the distal parts of the lung by ventilation, resulting in quicker spread in a few breaths and more uniform liquid distribution throughout the lungs. Transit and delivery times depend on plug volume, among other factors. Although the exogenous surfactant takes in the order of minutes to reach the alveoli, the lowering of surface tension at the distal ends occurs very rapidly – within seconds – as the result of the compression of the endogenous surfactant (8).
How to deliver surfactant into the pulmonary airways?
There are two common modes of delivering surfactant into the pulmonary airways: bolus infusion (one or multiple aliquots); or continuous infusion (2) (Box 1). Surfactant has also been given by nebulization; however, because this method and preparation remain under investigation, it will not be reviewed here.
What are the aspects of surfactant administration?
The present article reviews several aspects of administration techniques that can influence the delivery of surfactant into the lungs: the bolus volume, injection rate, gravity and orientation, ventilation strategies and development of airway obstruction, alveolar recruitment, and viscosity and surface tension of the fluid instilled. A surfactant administration protocol that was developed and implemented in our unit, based on the best available evidence, is included in Appendix 1.
Is surfactant therapy an exogenous therapy?
Exogenous surfactant therapy has an established role in the management of neonatal respiratory distress syndrome ( RDS). This article summarises the current evidence on surfactant therapy. The use of surfactant for the treatment or prophylaxis of neonatal RDS results in a 30% to 65% relative reductio …
Is surfactant used for RDS?
Exogenous surfactant therapy has an established role in the management of neonatal respiratory distress syndrome (RDS). This article summarises the current evidence on surfactant therapy. The use of surfactant for the treatment or prophylaxis of neonatal RDS results in a 30% to 65% relative reduction in the risk of pneumothorax and up to a 40% relative reduction in the risk of mortality. Adverse effects, of which pulmonary haemorrhage is of most concern, are infrequent and long-term follow-up studies of treated patients are reassuring. Natural surfactants have advantages over synthetic surfactants, including a lower frequency of pneumothorax and a lower mortality. Prophylactic administration of surfactant is preferred over 'rescue' administration, especially in infants of < 30 weeks' gestation, as it decreases the risk of pneumothorax, pulmonary interstitial emphysema and neonatal mortality. Prophylaxis can be administered after initial resuscitation and stabilisation. In preterm infants who do not receive prophylactic surfactant, the first dose of surfactant should be administered as early as possible--early selective treatment decreases the risk of pneumothorax, pulmonary interstitial emphysema, chronic lung disease and neonatal mortality. A regimen of using multiple doses of surfactant if required has advantages over a single dose regimen. Exogenous surfactant therapy has also been used in neonatal respiratory disorders other than RDS. In trials in severe meconium aspiration syndrome, surfactant therapy reduced the need for extracorporeal membrane oxygenation. Its role in other disorders requires testing. The development and testing of newer surfactants is in progress.
What is the role of pharmacy in surfactant therapy?
The pharmacy will be responsible for ensuring proper preparation of the surfactant, verifying dosing and administration, and serving as a drug information resource to the rest of the team. Only with an interprofessional team approach and open communication can surfactant therapy optimally reduce the morbidity of respiratory distress syndrome in neonates. [Level 5]
How to administer surfactant?
Surfactant is administered in liquid form via an endotracheal tube in a single bolus dose as quickly as the neonate tolerates. Some studies recommend administering all the surfactant at once, while others advocate dividing the bolus into smaller aliquots.
What is surfactant in the lung?
Pulmonary surfactant is a lipoprotein complex that lines the alveoli and decreases the surface tension to prevent lung atelectasis. Surfactant deficiency is a documented cause of neonatal respiratory distress syndrome (NRDS), a major cause of morbidity and mortality in premature infants. Therapeutic indications for surfactant replacement therapy include neonates with clinical and radiographic evidence of respiratory distress syndrome (RDS) and infants who require endotracheal intubation and mechanical ventilation secondary to respiratory failure. Surfactant is prophylactically administered in neonates at risk of developing NRDS. This activity will discuss the biochemical structure of surfactant, its administration, related complications, and the future of surfactant therapy.
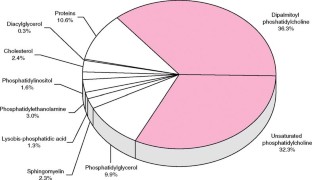
What are the components of surfactant?
Surfactant proteins comprise about 10% of the structure and interact extensively with phospholipids. They are SP-A, SP-B, SP-C, and SP-D. The SP-A and SP- D proteins are part of the innate immune response. These proteins coat bacteria and viruses, allowing phagocytosis and destruction by macrophages.[5] SP-A also appears to be a part of a negative feedback mechanism that controls surfactant release from type II alveolar cells. SP-B and SP-C are hydrophobic proteins that control the rate at which surfactant covers the surface of alveoli.
Where is pulmonary surfactant produced?
Its production begins around 26 weeks gestation and reaches mature levels at approximately 35 weeks. It is produced in the endoplasmic reticulum (ER) of type two pneumocytes and secreted from the lamellar bodies of type two pneumocytes.[4] Other cells in the lung, namely club or Clara cells, also produce surfactant. This lipoprotein mixture enhances lung compliance and aids in lowering the surface tension of the air-liquid interface within alveolar walls, which will ultimately prevent atelectasis. [1]
Is surfactant used for intubation?
Subsequently, in selected patients, surfactant administration may be considered an alternative to intubation with prophylactic or early surfactant administration. Surfactant replacement therapy is administered by trained personnel in a clinical setting where equipment for intubation and resuscitation are readily available.
Is surfactant toxic to the body?
Given that surfactant is a substance produced in the body and administered only when deficient, there have not been any serious reports of toxicities related to surfact ant administration. The prerequisites for administration, namely endotracheal intubation and CPAP usage, carry some inherent risks, as mentioned above.
What is the surfactant taken up by?
The Surfactant is taken up by the alveolar macrophages but more is taken by the endocytosis in type 2 epithelial cells.The major constituents of surfactant are dipa lmitoylphosphatidylcholine (lecithin), phosphatidylglycerol, apoproteins, and cholesterol. With advancing gestational age, increasing. The major constituents ...
How Surfactant Forms and Reabsorbed?
Type 2 Pneumocytes forms a membrane-bound organelle – lamellar inclusion bodies containing phospholipids. They are secreted into the alveolar lumen by exocytosis. The lamellar bodies are converted to phospholipid film. Lung surfactant has a very short half-life. It is about only 14 hours. The Surfactant is taken up by the alveolar macrophages but more is taken by the endocytosis in type 2 epithelial cells.The major constituents of surfactant are dipalmitoylphosphatidylcholine (lecithin), phosphatidylglycerol, apoproteins, and cholesterol. With advancing gestational age, increasing
What are the constituents of surfactant?
The major constituents of surfactant are dipalmitoylphosphatidylcholine (lecithin), phosphatidylglycerol, apoproteins, and cholesterol. With advancing gestational age, increasing a number of phospholipids are synthesized and stored in type-2 alveolar cell These surface active agents are released into the alveoli to maintain alveolar stability by ...
What happens if you don't have pulmonary surfactant?
Deficiency of pulmonary surfactant leads to alveolar atelectasis, edema, and cell injury. Subsequently, serum proteins that inhibit surfactant function leak into the alveoli. The Majority of RDS/HMD is self-limiting. Microscopically there are eosinophilic membranes in collapsed alveoli (so is the name HMD) and sometimes pulmonary hemorrhage and interstitial emphysema.
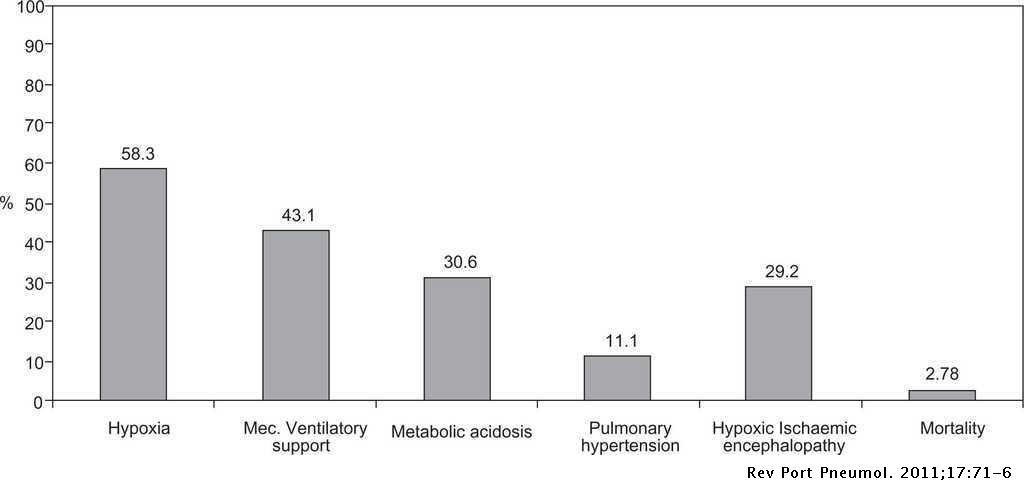
What is RDS in babies?
Respiratory distress syndrome (RDS) is defined as respiratory difficulty starting shortly after birth, commonly in a preterm newborn, and is due to deficiency of pulmonary surfactant. It occurs in 15-30% of those between 32 and 36 weeks of gestational age, in about 5% beyond 37 weeks and rarely at term. Deficiency of pulmonary surfactant leads ...
How to test for surfactant?
Test for surfactant function: Shake test (bed side test): Serial dilutions of ethanol are added to the amniotic fluid or gastric aspirate to allow for removal of non-surfactant foam. The sample is then shaken for 15 seconds to permit formation of a stable foam layer. The presence of bubbles in presence of adequate surfactant that persists on the surface for 15 minutes is considered a positive test; implying a very low risk for RDS.
What is the main function of surfactant?
The main function of surfactant is to reduce surface tension, so that decrease the work of breathing. Surfactant forms a thin monomolecular layer at the air fluid interface. Surfactant layer is not static. It is continuously secreting and reabsorbing. Deficiency of surfactant causes Respiratory Distress Syndrome (ARDS) in Newborn.
What is surfactant deficiency in newborns?
Surfactant Deficiency in Newborns is associated with Infant Respiratory Distress Syndrome, or IRDS. It is a breathing disorder in newborns, which results primarily due to premature delivery of the baby. The condition arises owing to reduced amounts of surfactants in immature lungs.
What is the purpose of surfactants in the lungs?
Surfactants are complex substances that help lower the surface tension of fluids in the lung. This helps keep the alveolar sacs (the sites of oxygen exchange) from collapsing. Thus, a deficiency of surfactants leads to non-compliant and stiff lungs
What is the name of the breathing disorder that occurs when a baby is born prematurely?
Infant Respiratory Distress Syndrome (IRDS) is a breathing disorder in newborns, which results primarily due to premature delivery of the baby. The condition arises owing to reduced amounts of surfactants in immature lungs
What is IRDS in babies?
Quick Summary: Infant Respiratory Distress Syndrome (IRDS) is a breathing disorder in newborns, which results primarily due to premature delivery of the baby. The condition arises owing to reduced amounts of surfactants in immature lungs.
What tests are needed for infant respiratory distress syndrome?
The diagnosis of Infant Respiratory Distress Syndrome may require chest X-rays and lab tests, apart from physical examination and symptom assessment
What is the most common condition in a baby born at 28 weeks?
It is estimated that about half of the babies born between weeks 28 and 32 of gestation develop Infant Respiratory Distress Syndrome, which is typically manifested as breathing trouble and bluish discoloration of the skin
Is infant respiratory distress syndrome good?
If diagnosed and treated promptly, the prognosis of Infant Respiratory Distress Syndrome is considered good. However, the prognosis also depends upon the severity of the condition
