What is CPT code for mastectomy for gynecomastia?
removing excess tissue or as an adjunctive procedure to contour the anterior chest wall. Applicable CPT Coding 19101 Biopsy of breast – incisional 19120 Excision of breast mass 19140 Mastectomy for gynecomastia 19182 Subcutaneous mastectomy 19318 Breast Reduction 15877 Suction assisted lipectomy, trunk Bilateral cases will be coded with the -50 modifier.
Is the CPT code the same as the procedure code?
When a service or procedure is described the same by both CPT coding and HCPCS coding, the CPT code is used. When a CPT code includes instructions to add more information, a HCPCS code is used. There are 16 sections in the HCPCS manual. ADVERTISEMENT.
What is the CPT code for removal of a cyst?
The CPT code is 11420- 11426. Pilonidal is the region where rear end buttock crease starts. The cyst in this region is removed by excisional procedure and the pus inside it is drained. During surgery, some tissues around the cyst are also removed. The CPT code for this procedure is 11770.
What is the CPT code for removal of a tumor?
The correct CPT code to report is CPT code 28043 (Excision, tumor, soft tissue of foot or toe, subcutaneous; less than 1.5 cm). You would not report a soft tissue tumor excision with the benign skin lesion excision codes.
What is the code for radical mastectomy?
The code for this type of more involved mastectomy is 19305 .
What is a complete mastectomy?
Radical mastectomy. For female patients, partial mastectomy involves excising the mass from the breast, taking along with it a margin of healthy tissue. The title of the procedure will be important when determining the physician’s intention for the procedure.
What is subcutaneous mastectomy?
During a subcutaneous mastectomy (19304), the surgeon dissects the breast away from the pectoral fascia and skin. As with the simple complete mastectomy, the surgeon removes all of the breast tissue, but spares the skin and pectoral fascia. The documentation should clearly illustrate the more complex nature of this procedure.
What is the procedure to transfer skin from another part of the body to the breast area?
Three additional reconstruction procedures include transferring skin from another part of the patient’s body to the breast area. The latissimus dorsi flap (19361) describes a procedure during which muscle and skin are taken from the patient’s back and used to reconstruct a breast.
Can breast implants be done at the same time as mastectomy?
Breast implants are, perhaps, the most well-known reconstruction methods. These can be done during the same surgical session as the mastectomy (19340) or at a later time (19342). If reconstruction is delayed, the surgeon may perform a tissue expansion (19357).
Is breast reconstruction surgery risky?
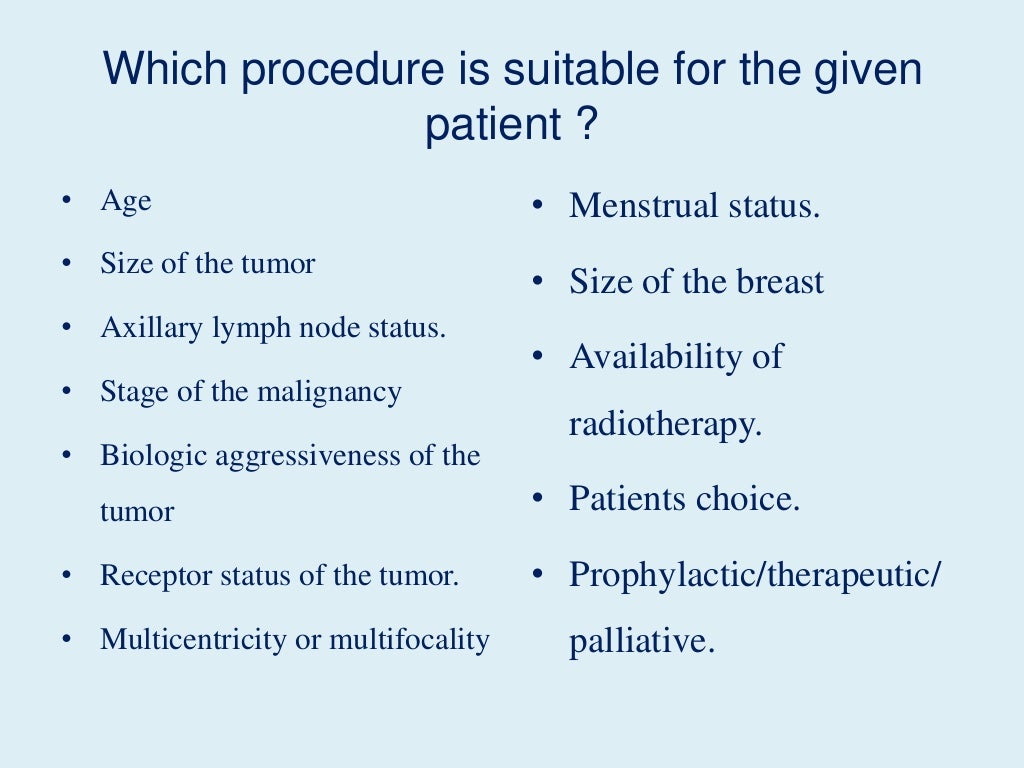
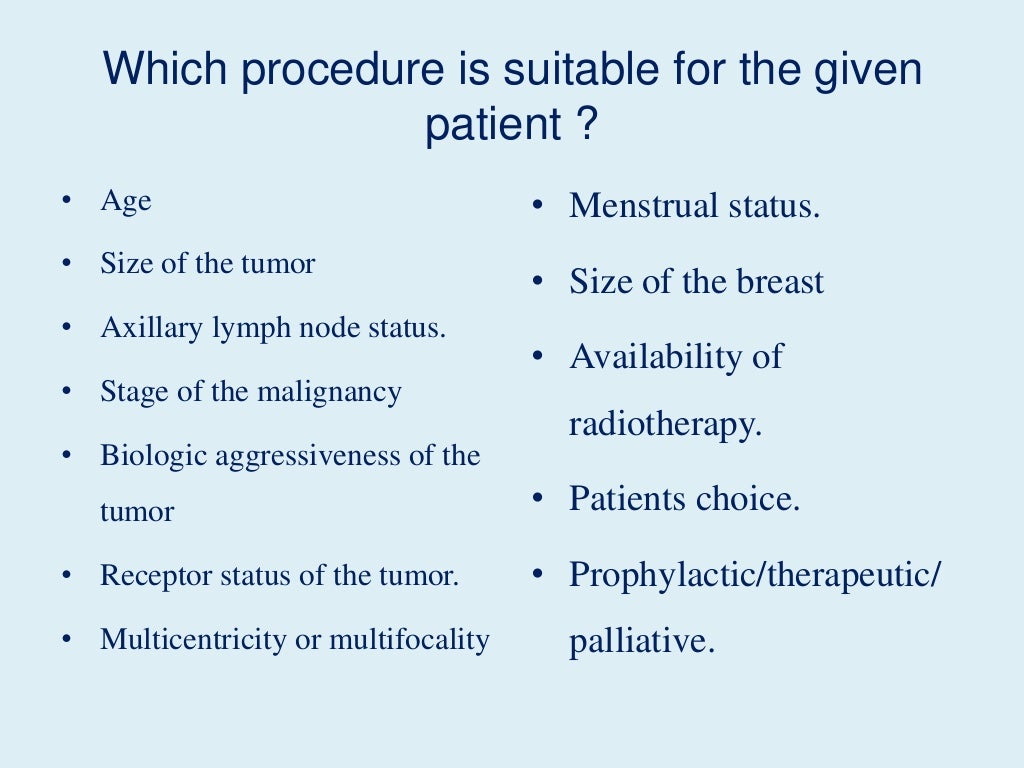
As with any surgery, there are risks to the reconstruction procedures, including the potential removal of the implanted prosthetic if a complication occurs. The size of the breast and the defect may also be factors in deciding which reconstruction method is best for the patient.
Can mastectomies be performed for cancer?
While some excisions may be performed for benign conditions, most mastectomies are performed for malignancy. About two-thirds of breast cancers require estrogen to thrive, and can therefore be managed with estrogen-blocking drugs. These drugs reduce the chance of the cancer recurring and improve survival rates.
What is the code for a mastectomy?
Report code 19303, Mastectomy, simple, complete, for the mastectomy. Sentinel node mapping is reported with code 38900, but it is an add-on code that may only be reported with select codes ( Report 38900 in conjunction with 19302, 19307, 38500, 38510, 38520, 38525, 38530, 38542, 38740, 38745 ). If an axillary lymph node biopsy was attempted but not performed, report 38525 and append modifier 53, Discontinued procedure, and report add-on code 38900 for the sentinel node mapping. If the payor prohibits reporting 38525-53, then the code for sentinel lymph node mapping (38900) also may not be reported because it is not an add-on code to 19303.
What is the correct code for a radical mastectomy?
However, removal of the implant in the right breast is a distinct operation. Because there is a code pair edit for 19307 and 19328, modifier 59, Distinct procedural service, is used instead of modifier 51, Multiple procedures. The correct codes and modifiers to report for these procedures are: 19307-LT , 19328-59- RT. NCCI edits are available online.
How many breasts did a surgeon remove?
The surgeon performed a partial mastectomy on one breast, but actually made two separate smaller incisions to remove two separate lesions (lumpectomy) from different non-contiguous areas of the breast.
What is the report code for gynecomastia?
Report code 19300, Mastectomy for gynecomastia, for this procedure. Removal of the mass was part of the mastectomy procedure. Remember, however, that in men, as in women, it is best practice to evaluate unspecified breast lesions with needle biopsy before a surgical biopsy.
What is the modifier 26 for imaging?
Modifier 26, Professional component, is appended to the imaging code when the services are performed in a facility setting. If an imaging service is performed in an office setting, then no modifier is appended because both the professional and technical components apply.
What is the code for a biopsy of breast?
Tru-Cut soft-tissue biopsy needles are considered core needles. So the correct code to report for this procedure is 19100, Biopsy of breast; percutaneous, needle core, ...
What is the code for a catheter and port placement?
The catheter and port placement is reported with code 36561, Insertion of tunneled centrally inserted central venous access device, with subcutaneous port; age 5 years or older. Append modifier 79, Unrelated procedure or service by the same physician or other qualified health care professional during the postoperative period, to code 36561. It would be inappropriate to append modifier 58, Staged or related procedure or service by the same physician or other qualified health care professional during the postoperative period, to code 36561 because the port is in a different anatomic location and is not a staged or more extensive procedure to the mastectomy.