CVVH uses convective clearance to remove toxins and solutes from the patients circulation, while CVVHD relies on diffusive clearance to remove these same toxins/solutes. This study will evaluate which of these two methods is more effective at clearing the body of waste/solutes. What type of dialysis
Dialysis
In medicine, dialysis is the process of removing excess water, solutes, and toxins from the blood in people whose kidneys can no longer perform these functions naturally. This is referred to as renal replacement therapy.
Full Answer
What is the difference between CRRT and CVVH?
CRRT. CRRT is continuous renal replacement therapy; extracorporeal blood purification over an extended period of time to replace kidney function; CVVH or CVVHF. CVVH is continuous veno-venous haemofiltration; convective dialysis + ultrafiltration; mid sized molecules (inflammatory cytokines)
What is the difference between CVVHD and CVVHDF?
CVVHD utilizes diffusion and convection. Replacement fluid is not used in CVVHD. CVVHDF uses a combination of convection and diffusion. Replacement fluid is also used to maintain euvolemia as in CVVH. Once deciding on the modality of choice, we must choose a dose. The dose of CRRT is often estimated by the effluent flow rate (mL/kg/hr).
Does continuous venovenous hemodialysis (CVVHD) provide both solute clearance and volume removal?
More commonly, when provided as continuous venovenous hemofiltration (CVVH), continuous venovenous hemodialysis (CVVHD), or continuous venovenous hemodiafiltration (CVVHDF), CRRT provides both solute clearance and volume removal, with the differences between these modalities related to the mechanisms for solute clearance ( Fig 1 ).
What is continuous renal replacement therapy (CRRT)?
Continuous Renal Replacement Therapy (CRRT) is a treatment option for patients in need of dialysis or fluid removal. It is typically only utilized in the ICU setting and patients require this particular therapy because of their hemodynamic instability.

Is Cvvhd a type of CRRT?
Continuous veno-venous haemodiafiltration (CVVHDF) uses the principles of both haemofiltration and haemodialysis, as described above. As this mode enables the ultimate removal and replacement of solutes and fluids within the blood, it is the most common mode chosen for CRRT.
What's the difference between Cvvh and CRRT?
The dose of CRRT is assessed based on the effluent flow rate, the sum of dialysate and total ultrafiltrate flow. During CVVH, the concentration of low-molecular-weight solutes such as urea in the ultrafiltrate is close to that in plasma water.
What does Cvvhd mean?
Two commonly used treatments are continuous venvenous hemofiltration (CVVH)and continuous venovenous hemodialysis (CVVHD). CVVH uses convective clearance to remove toxins and solutes from the patients circulation, while CVVHD relies on diffusive clearance to remove these same toxins/solutes.
What is Cvvhd used for?
CVVHD has been used primarily to provide renal replacement therapy in critically ill, hemodynamically unstable adult patients with acute renal failure. It also has been used to treat infants and children with inborn errors of metabolism.
Does Cvvh use dialysate?
Continuous veno-venous hemofiltration (CVVH) removes larger volumes of fluid mainly via convection. Replacement fluid is added. No dialysate is used. CVVH is effective method for removal of large molecules.
Is Cvvhdf better than Cvvh?
Abstract. We hypothesized that patients with sepsis and AKI, especially patients without preserved renal function, and treated with continuous veno-venous hemodiafiltration (CVVHDF), have lower risk for mortality than patients treated with continuous veno-venous hemofiltration (CVVH).
What are the types of CRRT?
CRRT comes in several forms. They include: slow continuous ultrafiltration, continuous venovenous hemodialysis, hemofiltration, hemodiafiltration, continuous arterio-venous hemofiltration, and slow low-efficiency daily dialysis.
How do you prescribe Cvvhd?
Blood flow rate prescription varies with modality. For CVVHD, the blood flow rate should be at least twice the dialysate flow rate to maximise the plasma to dialysate concentration gradient. For CVVH, blood flow rate should be titrated to prevent a filtration fraction (plasma water removal to plasma flow ratio) > 25%.
What is the difference between dialysis and CRRT?
CRRT is a slower type of dialysis that puts less stress on the heart. Instead of doing it over four hours, CRRT is done 24 hours a day to slowly and continuously clean out waste products and fluid from the patient. It requires special anticoagulation to keep the dialysis circuit from clotting.
How long can a patient stay on CRRT?
A general surgical patient may survive after 6 or more days of CRRT, and this survival is likely based on the presence of a correctable problem. We do not encourage the blanket statement that all general surgical patients with multiple-system organ failure should not be allowed to continue CRRT after 6 days.
Who needs CRRT?
You may get CRRT if your kidneys aren't working the way they should and you need a slower, gentler type of dialysis. CRRT may be used for kidney failure from an injury, an illness, or a reaction to medicine. Other organs such as the liver, heart, and lungs may not work as well either. Shock can cause this.
What does replacement fluid do in CRRT?
Replacement fluid is the fluid used to dilute the post-filter blood in haemofiltration, restoring volume and buffering the blood as it returns to the patient. In CRRT, these fluids are usually supplied as 5000ml bags, pre-packed and sterilised.
What are the disadvantages of CRRT?
The major disadvantage of CRRT is its relatively lower clearance rate when compared to standard intermittent hemodialysis. This large comparative advantage to hemodialysis has made the technique the gold standard for extracorporeal removal of xenobiotics.
What is the difference between hemofiltration and hemodialysis?
A: Haemodialysis – solute is driven across a semipermeable membrane by diffusion. B: Haemofiltration - fluid is driven across the semipermeable membrane by convection. The solute- containing plasma water is removed from the body and replaced with clean fluid.
What is the difference between hemofiltration and hemodiafiltration?
Hemofiltration (HF) is a technique based mainly on convection, whereas hemodiafiltration (HDF) combines convection and diffusion. Convection is the process during which solutes and solvent move according to the pressure gradient.
What is the most common indication for using CRRT?
The most common indications for CRRT are acute renal failure complicated with heart failure, volume overload, hypercatabolism, acute or chronic liver failure, and/or brain swelling.
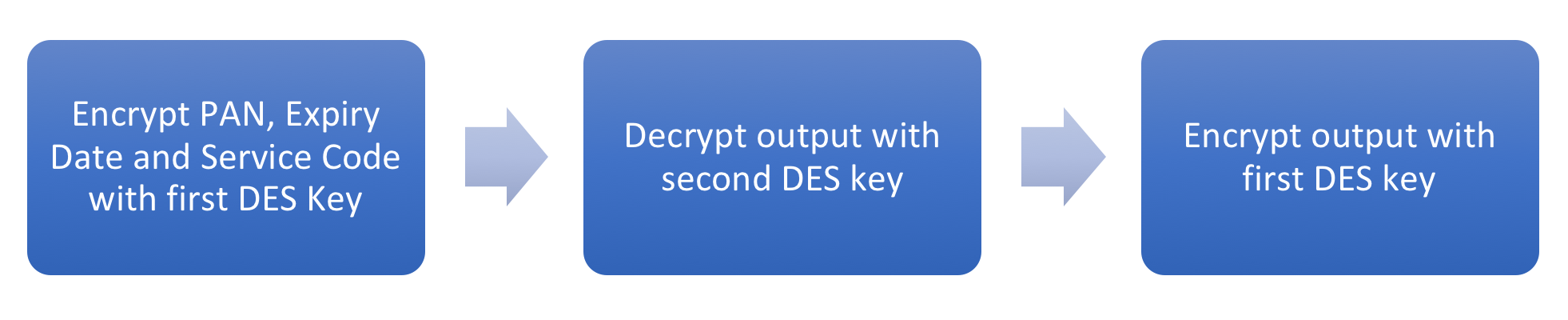
What is CRRT in medical terms?
CRRT = continuous renal replacement therapy. The most common complication during CRRT is circuit clotting, and the most common reason for circuit clotting is inadequate catheter function resulting in flow restriction and pressure alarms that interrupt blood flow.
How does ultrafiltration work in CVVH?
In CVVH, a high rate of ultrafiltration across the semi-permeable hemofilter membrane is created by a hydrostatic gradient, and solute transport occurs by convection ( Fig 2 A). Solutes are entrained in the bulk flow of water across the membrane, a process often referred to as “solvent drag.” 1, 27 High ultrafiltration rates are needed to achieve sufficient solute clearance, and the ultrafiltrate volume beyond what is required to achieve desired net fluid removal is replaced with balanced IV crystalloid solutions. These replacement solutions may be infused into the extracorporeal circuit either prior to or following the hemofilter. Because the high ultrafiltration rate hemoconcentrates the blood as it passes through the hemofilter fibers, the risk of sludging and fiber occlusion is increased. Prefilter infusion of replacement fluid dilutes the blood entering the hemofilter, mitigating this hemoconcentration. However, prefilter administration of replacement fluid dilutes the solute content of the blood, reducing effective solute clearance at a fixed ultrafiltration rate. Postfilter infusion has no such effects.
What is CRRT in AKI?
CRRT has become a mainstay in the management of AKI in critically ill patients. In patients who do not have objective indications for the emergent initiation of renal support, the optimal timing of RRT remains controversial. Although the use of continuous therapies may facilitate management in hemodynamically unstable patients, existing data do not show that use of CRRT results in improved survival or recovery of kidney function compared with alternatives such as conventional IHD and PIRRT. Large, well-designed clinical trials have established that for the majority of patients, augmenting solute clearance using effluent flow rates > 20 to 25 mL/kg per hour is not associated with improved outcomes; however, optimal strategies for volume management still must be defined. Similarly, other aspects of the management of CRRT are subject to substantial variations in practice, including strategies for anticoagulation. Finally, the role of CRRT needs to be considered in the setting of overall goals of care and the use of other life-sustaining treatments.
What is the criterion for discontinuing CRRT?
There are no specific criteria for discontinuation of CRRT because of recovery of kidney function or transition to other modalities of RRT. 59, 94, 95 An initial manifestation of recovery of kidney function is increased urine output, although specific criteria are sparse. In the observational Beginning and Ending Supportive Therapy for the Kidney (BEST Kidney) study, a urine output > 400 mL/d without concomitant diuretic therapy was a predictor of successful CRRT discontinuation. 96 In this observational cohort, patients who were successfully discontinued from CRRT without requiring re-initiation were more likely to survive to hospital discharge compared with those requiring re-initiation of CRRT. In another study, urine output > 500 mL/d was proposed as a criterion for discontinuation of RRT in a study of initiation and discontinuation of therapy in patients with AKI. 97 The usefulness of this criterion is uncertain, however, as the treating clinicians continued RRT despite this recommendation approximately two thirds of the time, citing continued volume overload as the most common reason for continuation of RRT. In the ATN study, a 6-h timed urine collection was obtained when the urine output was > 750 mL/d. 62 RRT was continued if the measured creatinine clearance was < 12 mL/min, was discontinued if > 20 mL/min, and was left to clinician judgment if the measured creatinine clearance was between 12 and 20 mL/min. Although these strategies can inform clinical decision-making, precise criteria for discontinuation of RRT are lacking.
What is the most common complication during CRRT?
Clotting of the extracorporeal circuit is the most common complication during CRRT. Practice patterns regarding the use of anticoagulation vary widely, with estimates of 30% to 60% of patients undergoing CRRT without anticoagulation. 62, 70 Although the use of anticoagulation is often avoided in patients who are coagulopathic, thrombocytopenic, or are having active hemorrhage, anticoagulation-free treatment may also be successful in the absence of coagulopathy and thrombocytopenia. Strategies to minimize the risk of clotting of the extracorporeal circuit include the following: use of higher blood flow rates; minimization of filtration fraction (the ratio of ultrafiltration to plasma flow) by using CVVHD rather than CVVH, or by infusing replacement fluids prefilter during CVVH and CVVHDF; ensuring optimal catheter function and responding promptly to machine alarms to minimize interruptions in blood flow; and increasing the frequency of scheduled replacement of the extracorporeal circuit. 62, 64 In the absence of anticoagulation, increased vigilance is required to ensure there is no compromise of delivered dose. 71
What is CRRT therapy?
Continuous renal replacement therapy (CRRT) is commonly used to provide renal support for critically ill patients with acute kidney injury, particularly patients who are hemodynamically unstable. A variety of techniques that differ in their mode of solute clearance may be used, including continuous venovenous hemofiltration with predominantly convective solute clearance, continuous venovenous hemodialysis with predominantly diffusive solute clearance, and continuous venovenous hemodiafiltration, which combines both dialysis and hemofiltration. The present article compares CRRT with other modalities of renal support and reviews indications for initiation of renal replacement therapy, as well as dosing and technical aspects in the management of CRRT.
What are the ethical issues associated with RRT?
Issues related to the clinical and ethical appropriateness of initiation or continuation of RRT often occur in patients with AKI. Discussions of initiation and discontinuation of therapy with patients and/or their family/surrogate decision-makers should be framed in light of the overall prognosis and goals of care, and need to consider other life-sustaining treatments in addition to RRT. It is important to ensure that both the primary managing service and nephrology consultants managing the RRT provide a consistent assessment of prognosis and treatment options, presented in a clear but sympathetic manner, to facilitate the process of shared decision-making. 98 The high mortality of AKI in the setting of critical illness and the complex and emotionally laden aspects of the decisions associated with initiating or discontinuing renal support suggest that early involvement of palliative care services may be of benefit. 99 Time-limited trials of RRT may be a useful strategy in circumstances in which there is uncertainty of prognosis or when the patient or family/surrogate decision-maker are not prepared to make a definite decision regarding initiating or discontinuing RRT and other life-sustaining care. 100
What is CVVH fluid?
CVVH utilizes convection. Replacement fluid is administer ed to maintain euvolemia and dilute the plasma concentration of solutes not present in the replacement fluid (i.e. urea nitrogen, creatinine).
How is CRRT dose calculated?
Once deciding on the modality of choice, we must choose a dose. The dose of CRRT is often estimated by the effluent flow rate (mL/kg/hr). It is commonly calculated as the ultrafiltration rate in CVVH, delivered dialysate flow rate in CVVHD, and a combination of both for CVVHDF.
How much effluent volume is required for CRRT?
The KDIGO clinical practice guideline for acute kidney injury (AKI) recommends “delivering an effluent volume of 20 to 25 mL/kg/h for CRRT in (AKI) .” However, the prescribed dose is not always delivered due to CRRT interruptions due to procedures, clotting, replacement of filters, and tubing changes. Therefore, the guidelines also recommend frequent evaluation and “assessment of the actual delivered dose in order to adjust the prescription.”
What is the effluent flow rate for CRRT?
So, for now, it seems that effluent flow rates of 20-25mL/kg/hr should be sufficient CRRT dosing in AKI – though careful attention should also be paid to actual delivered as well as clinical parameters that may justify dosing adjustments.
Easily Switch Between Therapies
PRISMAX and PRISMAFLEX Systems deliver multiple modes of Continuous Renal Replacement Therapy (CRRT) without the need for additional equipment.
Simplify Electrolyte Management With Our Comprehensive Portfolio of CRRT Solutions
Ready to use: Premixed solutions may help minimize preparation time, waste, and potential for medication errors 1,2
PHOXILLUM Solution
The ONLY FDA-approved premixed CRRT replacement solution with phosphate, available in 2 formulations
PRISMASATE Solution
Pam Waters, RN, explains the uses and benefits of CRRT replacement solutions, and the differences between pre- and post- replacement solutions.
What is CRRT in ICU?
Continuous Renal Replacement Therapy (CRRT) is a treatment option for patients in need of dialysis or fluid removal. It is typically only utilized in the ICU setting and patients require this particular therapy because of their hemodynamic instability. CRRT is a much slower type of dialysis than regular HD, as it pulls fluid or cleans the blood continuously, 24 hours a day, rather than over a 2-4 hr treatment. Some facilities only use this treatment option in ICU patients with renal failure, even if they are hemodynamically stable. This type of therapy relies on the bedside nurse, who has special training in this technology and the equipment. It requires you to be aware of how the patient responds to the treatment both metabolically and hemodynamically at all times.
What happens if a CRRT circuit stops cycling?
The bedside nurse should always have saline flushes and heparin (or the anticoagulant ordered) within reach if the machine decides to clot off and stop cycling the blood. If the machine stops cycling and appears to be trying to clot, the patient’s blood should be returned and therapy discontinued with the current circuit. Each circuit can hold approximately 150-250 mL blood, which can add up, especially if circuits are replaced 2-3 times a shift.
When in doubt of the circuit clotting, what to do?
When in doubt of the circuit clotting, rinse back. If the patient is getting more hypotensive or unstable, stop treatment and rinse back.
Can a fistula be used with a CRRT?
Fistulas are common for established dialysis patients but cannot be used with CRRT. This is because it is pump-driven and incorporates venovenous extracorporeal circuits. There is a red and a blue line, but it will both be venous and should never be arterial. Once the line is established, it needs to be anticoagulated as soon as it is inserted. The amount of required heparin will be labeled on each port hub. CRRT machine orders will be given by the nephrologist and can be adjusted during the treatment. Patients will either run with a positive, negative, even, or zero fluid balance. Blood flow rate can be adjusted to help prevent clotting, and dialysate rate is usually calculated depending on patient weight and electrolytes. Lab orders and ABGs are followed based on physician preference, patient condition, and/or for any acute change.
Which circuit is blood driven through?
blood driven through a highly permeable membrane by a peristaltic pump and via an extracorporeal circuit originating in central vein and terminating in a central vein
What is negative pressure in the dialysate compartment?
negative pressure in the dialysate compartment facilitates ultrafiltration, created by decreasing the oncotic pressure of plasma by pre-dilution
What is the fraction of plasma that is removed from blood during haemofiltration?
Filtration fraction is the fraction of plasma that is removed from blood during haemofiltration.
Which direction does dialysis run?
during dialysis the electrolyte solution (dialysate) runs in the opposite direction (countercurrent) to blood flow separated by a semi-permeable membrane.
What is the coefficient of ultrafiltration?
a membrane’s effectiveness to ultrafiltrate fluid is described by the ultrafiltration coefficient (KUF), which is QUF/ deltaP (volume of ultrafiltrate per unit time, divided by the pressure gradient across the membrane)
Does continuous venovenous hemofiltration lower mortality?
We hypothesized that patients with sepsis and AKI, especially patients without preserved renal function, and treated with continuous veno-venous hemodiafiltration (CVVHDF), have lower risk for mortality than patients treated with continuous veno-venous hemofiltration (CVVH). Patients were included i …
Is CRRT good for AKI?
CRRT has been associated with improved renal recovery, but it should be started earlier in AKI evolution with still preserved hourly urine output which is the most sensitive and prognostic marker of survival in septic patients with AKI.