All ESBLs are acquired resistance mechanisms. ESBL hydrolyze 3GC and 4GC, but do not hydrolyze cefoxitin. ESBLs are inhibited by beta-lactamase inhibitors – clavulanic acid, sulbactam, & tazobactam. AmpC is also an acquired resistance in E. coli, K. pneumoniae, K. oxytoca, and P. mirabilis. AmpC is not inhibited by clavulanic acid, sulbactam, or tazobactam, but it may be inhibited by cloxacillin (new available inhibitors as avibactam and relebactam also have inhibitory activity).
What is the difference between ESBLs and AmpC-type β-lactamases?
AmpC β-lactamases, in contrast to ESBLs, hydrolyse broad and extended-spectrum cephalosporins (cephamycins as well as to oxyimino-β-lactams) but are not inhibited by β-lactamase inhibitors such as clavulanic acid. AmpC-type β-lactamase organisms are often clinically grouped through the acronym, "SPACE": Serratia,...
Are all ESBLs acquired resistance?
All ESBLs are acquired resistance mechanisms. ESBL hydrolyze 3GC and 4GC, but do not hydrolyze cefoxitin. ESBLs are inhibited by beta-lactamase inhibitors – clavulanic acid, sulbactam, & tazobactam. AmpC is also an acquired resistance in E. coli, K. pneumoniae, K. oxytoca, and P. mirabilis.
Are ESBL and AmpC-producing bacteria common in humans?
In recent years, various studies have been conducted on the occurrence of ESBL and/or AmpC-producing bacteria in humans. It is being observed more and more often that ESBL-producing bacteria play a major role in healthcare facilities as the pathogen that causes so-called nosocomial, or hospital-acquired, infections.
What is ESBL and how does it affect the body?
ESBL enzymes break down and destroy some commonly used antibiotics, including penicillins and cephalosporins, and make these drugs ineffective for treating infections. This resistance means that there are fewer antibiotic options available to treat ESBL-producing Enterobacterales infections.
What does AmpC mean?
AMPCAcronymDefinitionAMPCAssociated Mail & Parcel CentersAMPCAutomatic Mail Processing Centre (India)AMPCAutomatic Message Processing CenterAMPCclass C Betalactamse3 more rows
What are AmpC organisms?
Summary: AmpC β-lactamases are clinically important cephalosporinases encoded on the chromosomes of many of the Enterobacteriaceae and a few other organisms, where they mediate resistance to cephalothin, cefazolin, cefoxitin, most penicillins, and β-lactamase inhibitor-β-lactam combinations.
What is considered ESBL?
Extended spectrum beta-lactamases (ESBLs) are defined as enzymes produced by certain bacteria that are able to hydrolyze extended spectrum cephalosporin. They are therefore effective against beta-lactam antibiotics such as ceftazidime, ceftriaxone, cefotaxime and oxyimino-monobactam.
Is ESBL and E coli the same?
Although ESBLs can be made by different bacteria, they are most often made by E. coli (more correctly called Escherichia coli).
What bacteria produces AmpC?
Many organisms have inducible AmpC production, most commonly E. cloacae, Klebsiella aerogenes, C. freundii, S. marcescens, Providencia stuartii, P.
What antibiotic covers AmpC?
Antibiotics recognized as potent inducers of the previously described pathway of AmpC production include the aminopenicillins, amoxicillin-clavulanate, narrow-spectrum (ie, first-generation) cephalosporins, and the cephamycins [5, 14].
How many types of ESBL are there?
There are at least 200 different types of ESBL enzymes. Researchers still have a lot to learn about them, in part because the infections involving ESBLs were only recently discovered.
What does ESBL positive mean?
In healthy people, this often means urinary tract infections. ESBL germs have also been identified in people returning to the United States after traveling abroad, especially to places where these germs are more commonly found.
Do patients with ESBL need to be isolated?
Because ESBL is discovered on clinical specimen (e.g., urine cultures), you will still know when an infection occurs due to an ESBL-producing bacteria. Patients that we know are carrying ESBL-producing bacteria will no longer require isolation or Contact Precautions.
How does a person get ESBL?
ESBL bacteria can be spread from person to person on contaminated hands of both patients and healthcare workers. The risk of transmission is increased if the person has diarrhoea or has a urinary catheter in place as these bacteria are often carried harmlessly in the bowel.
What is the best antibiotic for ESBL UTI?
Carbapenems are considered the most reliable treatment for infections caused by ESBL- producing bacteria. Despite their utility, resistance has emerged, placing a focus on finding alternative antibiotics for UTIs so that carbapenems can be reserved for more serious infections.
Does ESBL ever go away?
Sometimes the strain will be lost naturally. In those with serious illnesses, ESBL-producing strains may be present for months or even years. Use of antibiotics probably does not help; antibiotics can treat infections but do not necessarily eliminate the bacteria from the body especially if there are some in the gut.
Are Cephamycin and cephalosporin same?
Cephalosporins include cephamycins, which differ from other cephalosporins in that they contain a 7-alpha-methoxy group, which imparts resistance to extended-spectrum beta-lactamases. The early cephalosporins differed mainly with respect to pharmacokinetic characteristics.
How is AmpC treated?
Suggested approach: Cefepime is suggested for the treatment of infections caused by organisms at moderate to high risk of significant AmpC production (i.e., E. cloacae, K. aerogenes, and C. freundii) when the cefepime MIC is ≤2 mcg/mL.
What does ESBL producer mean?
ESBL stands for Extended Spectrum Beta-Lactamase. Beta-lactamases are enzymes produced by some bacteria that may make them resistant to some antibiotics. ESBL production is associated with a bacteria usually found in the bowel.
What is the difference between a penicillin and a carbapenem?
In terms of structure, the carbapenems are very similar to the penicillins (penams), but the sulfur atom in position 1 of the structure has been replaced with a carbon atom, and an unsaturation has been introduced—hence the name of the group, the carbapenems.
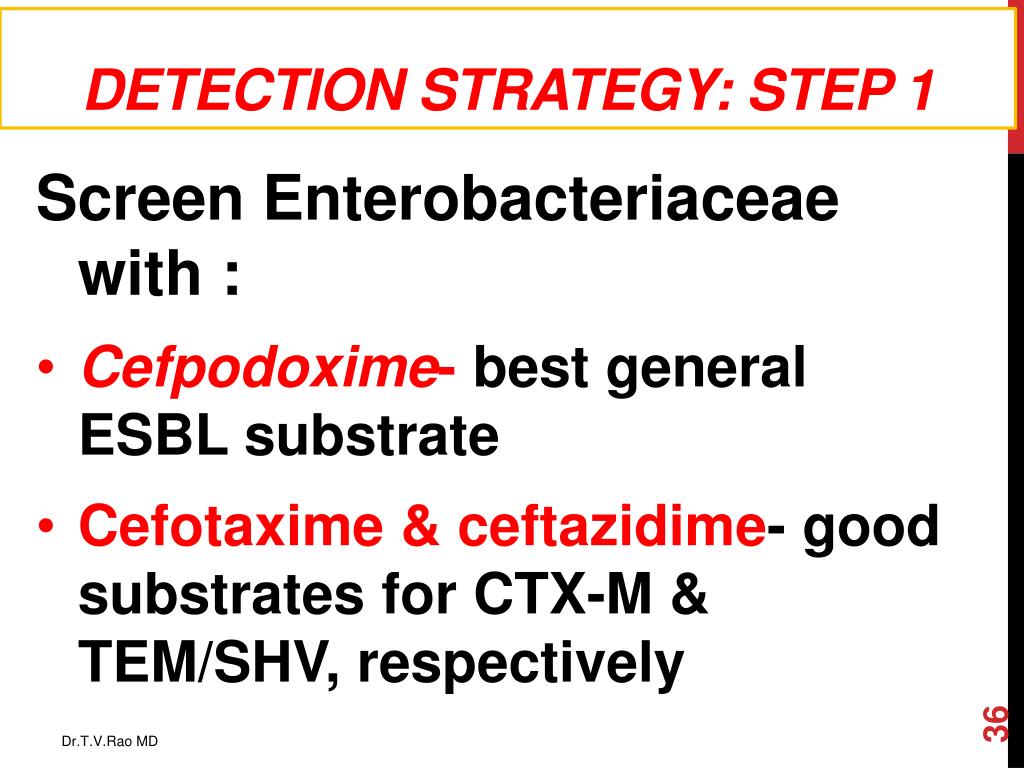
How to detect ESBL?
Let’s start some basic rules: 1 Screening and detection of ESBLs focuses on E. coli, K. pneumoniae, K. oxytoca, and P. mirabilis. This group of organisms do not carry intrinsic resistance against 3GC, 4GC or cefoxitin. 2 All ESBLs are acquired resistance mechanisms. ESBL hydrolyze 3GC and 4GC, but do not hydrolyze cefoxitin. ESBLs are inhibited by beta-lactamase inhibitors – clavulanic acid, sulbactam, & tazobactam. 3 AmpC is also an acquired resistance in E. coli, K. pneumoniae, K. oxytoca, and P. mirabilis. AmpC is not inhibited by clavulanic acid, sulbactam, or tazobactam, but it may be inhibited by cloxacillin (new available inhibitors as avibactam and relebactam also have inhibitory activity). AmpC has a high affinity to hydrolyze cefoxitin but not cefepime which results in AmpC being cefoxitin resistant and cefepime susceptible. 4 From an Infection Prevention perspective, AmpC has the same epidemiological importance as an ESBL, it is because AmpC is a plasmid-mediated acquired resistance (except for some E. coli with derepressed chromosomal AmpC) and could require isolation based on facility’s polices
How to confirm ESBL?
The most common method of ESBL confirmation is the phenotypic double-disk diffusion method (see image below) based on the inhibition of clavulanic acid over the ESBL enzyme recovering the activity of cefotaxime and/or ceftazidime. If the activity of either one of these two 3GC is recovered by clavulanic acid, then the presence of an ESBL is confirmed. Although the recovering of only one 3GC is required, it is recommended to test both agents with and without clavulanic acid to improve the sensitivity of this method. This technique is based on the principles that ESBL enzymes are inhibited by clavulanic acid and evidence of restored activity of the cephalosporin by this inhibitor indicates the presence of this resistance mechanism.
What are ESBLs inhibited by?
All ESBLs are acquired resistance mechanisms. ESBL hydrolyze 3GC and 4GC, but do not hydrolyze cefoxitin. ESBLs are inhibited by beta-lactamase inhibitors – clavulanic acid, sulbactam, & tazobactam.
Why is it important to test for ESBL?
Proper screening and testing for ESBL is critical for both epidemiology and antimicrobial stewardship.
Is ESBL testing necessary?
Since 2010, the Clinical and Laboratory for Standards Institute (CLSI) M100 Performance Standards for Antimicrobial Susceptibility Testing has stated “when using the current breakpoints, routine ESBL testing is no longer necessary before reporting results.” Therefore, many laboratories do not routinely perform ESBL screening or confirmation anymore. In addition, it is no longer necessary to edit the results for penicillins, cephalosporins, and aztreonam from susceptible to resistant for confirmed ESBL isolates. However, ESBL testing may still be useful for epidemiological or infection prevention purposes.
Can a SPICE-M carry an ESBL?
Yes, although it is important to always consider that SPiCE-M organisms to carry a chromosomal AmpC, they may also carry an ESBL as an acquired plasmid.
Is ESBL evident with 3GC?
At this point, an ESBL is evident and beta-lactam treatment options are likely limited to carbapenems. If a more specific antimicrobial therapy is desired, continue evaluation in Step 2.
What does ESBL mean in health?
In healthy people, this often means urinary tract infections. ESBL germs have also been identified in people returning to the United States after traveling abroad, especially to places where these germs are more commonly found. Top of Page.
How many cases of ESBL in 2017?
In 2017, there were an estimated 197,400 cases of ESBL-producing Enterobacterales among hospitalized patients and 9,100 estimated deaths in the United States [ Source: 2019 AR Threats Report ].
What is the treatment for ESBL?
Infections caused by ESBL-producing germs are treated with antibiotics, but because they are resistant to many commonly prescribed antibiotics, treatment options might be limited. People with these infections sometimes need to be hospitalized for treatment with IV antibiotics. Carbapenem antibiotics, which are typically reserved for highly ...
Can carbapenems kill ESBL?
Carbapenems are one of the few remaining antibiotics that can treat ESBL-producing germs, but resistance enzymes that destroy these antibiotics are on the rise, too. The more we rely on this important class of antibiotics, the greater the risk of spreading resistance to them.
Can you take oral antibiotics for ESBL?
Instead of taking oral antibiotics at home, patients with these infections might require hospitalization and intravenous (IV) carbapenem antibiotics. Carbapenems are one of the few remaining antibiotics that can treat ESBL-producing germs, but resistance enzymes that destroy these antibiotics are on the rise, too.
What is the structure of SBLs?
The structure of a Streptomyces serine β-lactamase (SBLs) is given by 1BSG. The alpha-beta fold ( InterPro : IPR012338) resembles that of a DD-transpeptidase, from which the enzyme is thought to have evolved from. Serine β-lactamases are grouped by sequence similarity into types A, C, and D.
When was ESBL first detected?
In the mid-1980s, this new group of enzymes, the extended-spectrum β-lactamases (ESBLs), was detected (first detected in 1979). The prevalence of ESBL-producing bacteria have been gradually increasing in acute care hospitals.
Is carbapenem a good antibiotic for ESBL?
Therefore, antibiotic options in the treatment of ESBL-producing organisms are extremely limited. Carbapenems are the treatment of choice for serious infections due to ESBL-producing organisms, yet carbapenem-resistant (primarily ertapenem resistant) isolates have recently been reported.
Is carbapenem stable to a metallo-lactamase?
Carbapenems are famously stable to AmpC β-lactamases and extended-spectrum-β-lactamases. Carbapenemases are a diverse group of β-lactamases that are active not only against the oxyimino-cephalosporins and cephamycins but also against the carbapenems. Aztreonam is stable to the metallo-β-lactamases, but many IMP and VIM producers are resistant, owing to other mechanisms. Carbapenemases were formerly believed to derive only from classes A, B, and D, but a class C carbapenemase has been described.