
Overall Function of Effectors -- Summary:
- Liver -- both releases glucose to blood and stores excess (as glycogen). a. ...
- Muscle -- stores or releases energy and protein. (Takes up glucose; stores excess as glycogen. ...
- Adipose Tissue -- stores or releases fat/ fatty acids. ...
How does blood glucose affect homeostasis?
Another process of homeostasis to do with blood glucose is involving glucagon, which is another hormone made in the pancreas. Glucagon is released when blood glucose levels are low, working similarly like insulin, but in a different way.
What is the hormone that controls glucose levels in blood?
The glucose levels in the blood are controlled by the hormonal system and these hormones are produced in the pancreas in the ares called islets of Langerans.
What stimulates the release of glucose into the bloodstream?
When blood glucose levels drop, such as after an overnight fast, the pancreas releases a hormone called glucagon. Glucagon binds a GPCR on liver and muscle cells called the glucagon receptor, which then stimulates the cells to release glucose into the bloodstream.
What are the organs involved in the homeostasis of blood sugar?
The main organs in this mechanism are the liver, the autonomic nervous system, pancreas and other glands of internal secretion called endocrine glands .” (Homeostasis of sugar, ©2012) In the control of blood glucose concentrations in the body are influenced by factors such as digestion of carbohydrates in food which...
Is the pancreas a receptor or effector?
Cells called receptors , which detect stimuli (changes in the environment). The coordination centre, such as the brain, spinal cord or pancreas, which receives and processes information from receptors around the body.
What kind of feedback is used for blood glucose regulation inside the body?
Negative feedbackNegative feedback If the blood glucose level is too low, the pancreas releases the hormone glucagon. This travels to the liver in the blood and causes the break-down of glycogen into glucose. The glucose enters the blood stream and glucose levels increase back to normal. This is an example of negative feedback.
What is the effector in a feedback loop?
An effector is the component in a feedback system that causes a change to reverse the situation and return the value to the normal range. Negative Feedback Loop. In a negative feedback loop, a stimulus—a deviation from a set point—is resisted through a physiological process that returns the body to homeostasis.
What does the effector do as the blood sugar falls?
Glucose, the regulated variable, is the principal source of energy for the organism in general, and particularly for the brain. During fasting, the liver (the main effector) breaks down stored glycogen, and glucose is secreted into the bloodstream.
Is blood glucose level a negative feedback loop?
The control of blood sugar (glucose) by insulin is a good example of a negative feedback mechanism. When blood sugar rises, receptors in the body sense a change. In turn, the control center (pancreas) secretes insulin into the blood effectively lowering blood sugar levels.
What are receptors and effectors in homeostasis?
The receptor senses the change in the environment, then sends a signal to the control center (in most cases, the brain) which in turn generates a response that is signaled to an effector. The effector is a muscle (that contracts or relaxes) or a gland that secretes.
What is the role of effectors in homeostasis?
An effector is any organ or tissue that receives information from the integrating center and acts to bring about the changes needed to maintain homeostasis. One example is the kidney, which retains water if blood pressure is too low.
Are sweat glands an effector?
For example, during body temperature regulation, temperature receptors in the skin communicate information to the brain (the control center) which signals the effectors: blood vessels and sweat glands in the skin.
Is blood sugar regulated by positive feedback?
Is blood sugar regulated by negative or positive feedback? Explain your answer. Blood sugar is regulated by negative feedback because insulin is released as a response to high blood sugar so that insulin can allow glucose to enter into cells in order to make blood sugar go back down to a normal level.
Is diabetes a positive feedback loop?
One example of a malfunctioning negative feedback loop is seen in type 1 diabetes. Insulin regulation is controlled through a negative feedback loop where pancreatic beta cells are the receptor cells. In type 1 diabetes, there are no pancreatic beta cells, they are destroyed by the immune system.
Is glucagon positive or negative feedback?
Insulin and glucagon work in what's called a negative feedback loop. During this process, one event triggers another, which triggers another, and so on, to keep your blood sugar levels balanced.
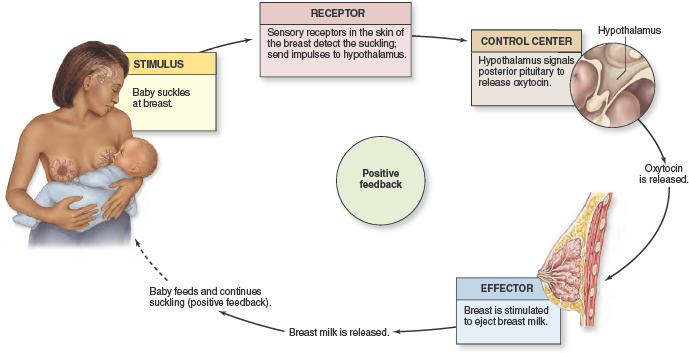
What's an example of a positive feedback loop?
Examples of processes that utilise positive feedback loops include: Childbirth – stretching of uterine walls cause contractions that further stretch the walls (this continues until birthing occurs) Lactation – the child feeding stimulates milk production which causes further feeding (continues until baby stops feeding)
What factors influence blood glucose levels?
In the control of blood glucose concentrations in the body are influenced by factors such as digestion of. carbohydrates in food which increases the production of glucose depending on how many carbohydrates. consumed.
What hormone is released when blood glucose levels are low?
Glucagon is released when blood glucose levels are low, working similarly like insulin, but in a different way. This hormone makes the liver release stored up glucose which then in turn raises the blood glucose levels to normal.
What is the difference between hypoglycaemia and hyperglycaemia?
Hypoglycaemia on the other hand is associated with low glucose levels and is considered less serious than hyperglycaemia as it is from too much administered insulin.
What happens when there is not enough insulin in the body?
When not enough insulin is available in the body, the. amount of glucose the cells are able to absorb will be reduced. From this the body will then respond to produce more insulin so that the amount of glucose absorbed is increased and able at higher levels to be absorbed. Another process of homeostasis to do with blood glucose is involving ...
What is the breakdown of glycogen?
The breakdown of glycogen is another which when detects an excess of glucose, glycogen is secreted returning the amount back to normal balance. Polysaccharide is made from excess glucose by glycogenesis, and glycogen becomes abundant in both liver and muscles. The pancreatic Islets of Langerhans are the sites of production of insulin, ...
Where is glucose produced in the pancreas?
The glucose levels in the blood are controlled by the hormonal system and these hormones are produced in the pancreas in the ares called islets of Langerans. “The maintenance of the blood sugar at normal levels is brought about by an efficient regulatory mechanism.
Is hypoglycaemia more serious than hyperglycaemia?
Hypoglycaemia on the other hand is associated with low glucose levels and is considered less serious than hyperglycaemia as it is from too much administered insulin. ( What is glucose homeostasis, ©2003-2012 ) The glucose molecules are broken down to produce ATP molecules; these cells power numerous cellular processes.
How does the body regulate glucose levels?
As described in the cell biology tutorial, the body requires volumes of glucose in order to create ATP. The amount of ATP demanded will fluctuate, and therefore the body regulates the availability of glucose to maximise its energy making potential. Two hormones are responsible for controlling the concentration of glucose in the blood. These are insulin and glucagon. The diagram illustrates the principle of negative feedback control in action involving blood/sugar levels. Pancreas Receptors The receptors of the pancreas are responsible for monitoring glucose levels in the blood, since it is important in every cell for respiration. Two types of cell release two different hormones from the pancreas, insulin and glucagon. These hormones target the liver, one or the other depending on the glucose concentration In cases where glucose levels increase, less glucagon and more insulin is released by the pancreas and targets the liver In cases where glucose levels decrease, less insulin and more glucagon is released by the pancreas and targets the liver The Liver The liver acts as a storehouse for glycogen, the storage form of glucose. When either of the above hormones target the liver, the following occurs Insulin - Insulin is released as a result of an increase in glucose levels, and therefore promotes the conversion of glucose into glycogen, where the excess glucose can be stored for a later date in the liver Glucagon - Glucagon is released as a result of an decrease in glucose levels, and therefore promotes the conversion of glycogen into glucose, where the lack glucose can be compensated for by the new supply of glucose brought about from glycogen Diabetes Diabetes insipidus is a condition where excess urine is excreted caused by the sufferers inability to produce ADH and pro Continue reading >>
What is the role of blood glucose regulation?
Blood glucose regulation involves maintaining blood glucose levels at constant levels in the face of dynamic glucose intake and energy use by the body. Glucose, shown in figure 1 is key in the energy intake of humans.
What is the purpose of homeostasis?
As you may remember, homeostasis is the maintenance of a stable internal environment within an organism, and maintaining a stable internal environment in a human means having to carefully regulate many parameters, including glucose levels in the blood. There are two major ways that signals are sent throughout the body.
Which organ is responsible for monitoring glucose levels in the blood?
Pancreas Receptors The receptors of the pancreas are responsible for monitoring glucose levels in the blood, since it is important in every cell for respiration. Two types of cell release two different hormones from the pancreas, insulin and glucagon.
Which hormones control glucose levels?
Two hormones are responsible for controlling the concentration of glucose in the blood. These are insulin and glucagon. The diagram illustrates the principle of negative feedback control in action involving blood/sugar levels.
Which hormones are released when there is high glucose in the blood stream?
In order to maintain this range there are two main hormones that control blood glucose levels: insulin and glucagon . Insulin is released when there are high amounts of glucose in the blood stream. Glucagon is released when there are low levels of glucose in the blood stream.
Where is insulin released?
Insulin is released from the beta cells in the islets of Langerhans found in the pancreas. Insulin is released when there is a high concentration of glucose in the blood stream.
What does my liver do with excess glucose?
When glycogen storage capacity of you liver is exceeded (200-300 g) you liver starts transforming glucose into fat.
How much glycogen does my liver store?
As a rule, maximun glycogen supplies in your liver are 200-300 g. This amount is enough to supply your brain with energy for 2 days. After that the energy is produced by breaking down fat stored in your body. This is important information for those fighting with excess weight: starving for 2 days won't make you lose any fat. Starving on and losing weight rapidly is dangerous.
What are the mechanisms of glucose homeostasis?
Mechanisms of blood glucose homeostasis. The mechanisms by which glycogen metabolism, glycolysis and gluconeogenesis are controlled in the liver both by hormones and by the concentration of glucose are reviewed .
Which enzyme controls glycolysis?
The control of glycolysis and of gluconeogenesis occurs mostly at the level of the interconversion of fructose 6-phosphate and fructose 1,6-bisphosphate under the action of phosphofructokinase 1 and fructose 1,6-bisphosphatase.
How is glycogen metabolism controlled in the liver?
The mechanisms by which glycogen metabolism, glycolysis and gluconeogenesis are controlled in the liver both by hormones and by the concentration of glucose are reviewed. The control of glycogen metabolism occurs by phosphorylation and dephosphorylation of both glycogen phosphorylase and glycogen synthase catalysed by various protein kinases ...
What is the hormonal effect of AMP?
The hormonal effect is to stimulate glycogenolysis by the intermediary of cyclic AMP , which activates directly or indirectly the protein kinases. The glucose effect is to activate the protein phosphatase system; this occurs by the direct binding of glucose to glycogen phosphorylase which is then a better substrate for phosphorylase phosphatase ...
What is the name of the enzyme that makes up fructose 2?
Fructose 2,6-bisphosphate is a potent stimulator of the first of these two enzymes and an inhibitor of the second. It is formed from fructose 6-phosphate and ATP by phosphofructokinase 2 and hydrolysed by a fructose 2,6-bisphosphatase.
Is glucose uptake the same as glucose 6-phosphatase?
Glucose uptake is indeed the difference between the activities of glucokinase and glucose 6-phosphatase. Since the Km of the latter enzyme is far above the physiological concentration of its substrate, the decrease in glucose 6-phosphate concentration proportionally reduces its activity.
Does phosphorylase a inhibit glycogen synthase?
Since phosphorylase a is a strong inhibitor of synthase phosphatase, its disappearance allows the activation of glycogen synthase and the initiation of glycogen synthesis. When glycogen synthesis is intense, the concentrations of UDPG and of glucose 6-phosphate in the liver decrease, allowing a net glucose uptake by the liver.
How does homeostasis control glucose levels?
The ideal level of blood glucose is 80 - 90mg of glucose per 100mls of blood. However this level is not static - it oscillates due to changes in the body which are brought about by actions such as eating a meal, exercising, or not eating for long periods. If blood glucose levels drop or rise dramatically there may be serious consequences such as hypo- or hyperglycaemia which can both cause death. Thus it is necessary for blood glucose levels to be …show more content… The level of blood glucose is constantly monitored by the beta cells. As the effects of insulin bring down the blood glucose level the cells secrete less and less of the hormone in accordance with the falling level of blood glucose - this continues until levels return to normal. The corresponding effect of this antagonistic mechanism occurs when blood glucose level have fallen too low - this is detected in the Islets of Langerhans by the alpha cells which are stimulated to produce glucagon. This hormone acts in two main ways to raise blood glucose concentration back to normal levels. Firstly, it stimulates the process of glycogenolysis whereby the liver and muscle cells convert glycogen into glucose to be discharged into the blood. In addition, it increases gluconeogenesis so that more glucose is synthesised from protein and fat sources. However if glucagon is allowed to encourage the production of glucose unchecked, the liver will begin to produce ketones which dangerously disrupt the acid/base balance in the body. The two… Continue reading >>
How does the body regulate glucose levels?
As described in the cell biology tutorial, the body requires volumes of glucose in order to create ATP. The amount of ATP demanded will fluctuate, and therefore the body regulates the availability of glucose to maximise its energy making potential. Two hormones are responsible for controlling the concentration of glucose in the blood. These are insulin and glucagon. The diagram illustrates the principle of negative feedback control in action involving blood/sugar levels. Pancreas Receptors The receptors of the pancreas are responsible for monitoring glucose levels in the blood, since it is important in every cell for respiration. Two types of cell release two different hormones from the pancreas, insulin and glucagon. These hormones target the liver, one or the other depending on the glucose concentration In cases where glucose levels increase, less glucagon and more insulin is released by the pancreas and targets the liver In cases where glucose levels decrease, less insulin and more glucagon is released by the pancreas and targets the liver The Liver The liver acts as a storehouse for glycogen, the storage form of glucose. When either of the above hormones target the liver, the following occurs Insulin - Insulin is released as a result of an increase in glucose levels, and therefore promotes the conversion of glucose into glycogen, where the excess glucose can be stored for a later date in the liver Glucagon - Glucagon is released as a result of an decrease in glucose levels, and therefore promotes the conversion of glycogen into glucose, where the lack glucose can be compensated for by the new supply of glucose brought about from glycogen Diabetes Diabetes insipidus is a condition where excess urine is excreted caused by the sufferers inability to produce ADH and pro Continue reading >>
How does glucagon affect the body?
Glucagon is a hormone that is produced by alpha cells in a part of the pancreas known as the islets of Langerhans. The role of glucagon in the body Glucagon plays an active role in allowing the body to regulate the utilisation of glucose and fats. Glucagon is released in response to low blood glucose levels and to events whereby the body needs additional glucose , such as in response to vigorous exercise. When glucagon is released it can perform the following tasks: Stimulating the liver to break down glycogen to be released into the blood as glucose Activating gluconeogenesis, the conversion of amino acids into glucose Breaking down stored fat (triglycerides) into fatty acids for use as fuel by cells Glucagon and blood glucose levels Glucagon serves to keep blood glucose levels high enough for the body to function well. When blood glucose levels are low, glucagon is released and signals the liver to release glucose into the blood. Glucagon secretion in response to meals varies depending on what we eat: In response to a carbohydrate based meal, glucagon levels in the blood fall to prevent blood glucose rising too high. In response to a high protein meal, glucagon levels in the blood rise. Glucagon in diabetes In people with diabetes, glucagon’s presence can raise blood glucose levels too high. The reason for this is either because not enough insulin is present or, as is the case in type 2 diabetes, the body is less able to respond to insulin. In type 1 diabetes, high levels of circulating insulin can inhibit the release of glucagon in response to hypoglycemia. Medications which affect gluca Continue reading >>
How does glucose work?
Here's how normal glucose metabolism works, and what happens when you have diabetes — a disease where your body either can't produce enough insulin or it can't use insulin properly. The food you eat consists of three basic nutrients: carbohydrates, protein and fat. During digestion, chemicals in your stomach break down carbohydrates into glucose, which is absorbed into your bloodstream. Your pancreas responds to the glucose by releasing insulin. Insulin is responsible for allowing glucose into your body's cells. When the glucose enters your cells, the amount of glucose in your bloodstream falls. If you have type 1 diabetes, your pancreas doesn't secrete insulin — which causes a buildup of glucose in your bloodstream. Without insulin, the glucose can't get into your cells. If you have type 2 diabetes, your pancreas secretes less insulin than your body requires because your body is resistant to its effect. With both types of diabetes, glucose cannot be used for energy, and it builds up in your bloodstream — causing potentially serious health complications. Continue reading >>
How does the pancreas regulate blood sugar?
Your pancreas constantly monitors and controls your blood sugar levels using two hormones. The best known of these is insulin. When your blood sugar levels rise after a meal your pancreas releases insulin. Insulin allows glucose to be taken into the cells of your body where it is used in cellular respiration. It also allows soluble glucose to be converted to an insoluble carbohydrate called glycogen which is stored in the liver and muscles. When your blood sugar levels fall below the ideal level your pancreas releases a different hormone called glucagon. Glucagon makes your liver break down glycogen, converting it back into glucose which can be used by the cells. Continue reading >>
How do hormones regulate blood sugar levels?
How do hormones regulate blood sugar levels? ‘Blood glucose testing’ is an activity designed to increase understanding of the hormones that control blood sugar in the body, and why this control is important in staying healthy. This activity is designed for students aged 11-14 and involves practical science techniques such as pipetting. Students can gain a practical understanding of the hormones that are secreted in the body when blood sugar levels are too high or too low. Aims: To introduce insulin and glucagon as hormones that help control blood sugar levels To give students the chance to develop practical science skills using pipettes and test tubes Curriculum links: Homeostasis Hormonal control in humans Hormones and eating Take home messages: blood glucose levels need to be kept in a very narrow “safe” range for our bodies to function correctly the hormones glucagon and insulin regulate blood sugar levels Glucagon is produced by the pancreas and stimulates glucose to be released from glycogen in the liver Insulin is produced by the pancreas and allows cells to absorb glucose from the bloodstream Discussion points: Diabetes occurs when blood glucose levels are not regulated properly. Type-1 diabetes is when you no longer produce insulin and your blood glucose level can become dangerously high unless you are given insulin regularly by injection. Type-2 diabetes is when you don’t produce enough insulin or no longer respond to the insulin you do produce. Type-1 diabetes is an autoimmune disease and tends to be diagnosed in children. Type-2 diabetes tends to affect older people or those who are over-weight. Continue reading >>
What organs regulate energy metabolism?
Go to: The pancreas is an exocrine and endocrine organ The pancreas has key roles in the regulation of macronutrient digestion and hence metabolism/energy homeostasis by releasing various digestive enzymes and pancreatic hormones. It is located behind the stomach within the left upper abdominal cavity and is partitioned into head, body and tail. The majority of this secretory organ consists of acinar—or exocrine—cells that secrete the pancreatic juice containing digestive enzymes, such as amylase, pancreatic lipase and trypsinogen, into the ducts, that is, the main pancreatic and the accessory pancreatic duct. In contrast, pancreatic hormones are released in an endocrine manner, that is, direct secretion into the blood stream. The endocrine cells are clustered together, thereby forming the so-called islets of Langerhans, which are small, island-like structures within the exocrine pancreatic tissue that account for only 1–2% of the entire organ (Figure 1).1 There are five different cell types releasing various hormones from the endocrine system: glucagon-producing α-cells,2 which represent 15–20% of the total islet cells; amylin-, C-peptide- and insulin-producing β-cells,2 which account for 65–80% of the total cells; pancreatic polypeptide (PP)-producing γ-cells,3 which comprise 3–5% of the total islet cells; somatostatin-producing δ-cells,2 which constitute 3–10% of the total cells; and ghrelin-producing ɛ-cells,4 which comprise <1% of the total islet cells. Each of the hormones has distinct functions. Glucagon increases blood glucose levels, whereas insulin decreases them.5 Somatostatin inhibits both, glucagon and insulin release,6 whereas PP regulates the exocrine and endocrine secretion activity of the pancreas.3, 7 Altogether, these hormones regul Continue reading >>
What hormone is released when blood glucose levels drop?
When blood glucose levels drop, such as after an overnight fast, the pancreas releases a hormone called glucagon. Glucagon binds a GPCR on liver and muscle cells called the glucagon receptor, which then stimulates the cells to release glucose into the bloodstream. Another hormone involved in glucose control is called glucagon -like peptide-1 (GLP-1).
What is the function of G-protein-coupled receptors in blood glucose control?
Blood glucose control depends heavily on proteins called G-protein-coupled receptors (GPCRs). GPCRs span cell membranes to relay signals from the outside in. Once activated by the binding of a substance, GPCRs trigger a cascade of responses inside the cell. These receptors are thus important targets for drug development.
What is the best medication to control blood glucose?
Medications such as insulin (which lowers blood glucose) and glucagon (which elevates it in an emergency) can help maintain blood glucose in a safe range. However, glucagon in particular can be difficult to administer. Blood glucose control depends heavily on proteins called G-protein-coupled receptors (GPCRs).
What are the glucagon receptors?
The glucagon and GLP-1 receptors are both important drug targets for type 2 diabetes and obesity. These results may help inform the design of new drugs to regulate blood glucose levels. —by Harrison Wein, Ph.D. References: Structure of the full-length glucagon class B G-protein-coupled receptor.
How does GLP-1 work?
It works by binding to another GPCR, the GLP-1 receptor, on cells in the pancreas. After a meal, the intestine produces GLP-1, which prompts the pancreas to produce insulin. Insulin, in turn, stimulates cells to take in glucose from the blood. The glucagon and GLP-1 receptors are both class B GPCRs. The structures of several class A GPCRs have been ...
Why are class B receptors not well studied?
The structures of several class A GPCRs have been solved, but class B receptors haven’t been as well studied because of technical challenges. Four international research teams reported the structures of the glucagon and GLP-1 receptors in Nature on June 8, 2017.
Who is the scientist who discovered the structure of the human glucagon receptor?
In one of the new papers, an international team led by Dr. Beili Wu from the Shanghai Institute of Materia Medica, Chinese Academy of Sciences, described the structure of the full length human glucagon receptor.
